Aspergillosis includes a broad spectrum of syndromes caused by the Aspergillus fungus that can lead to pulmonary disease, ranging from allergic manifestations to severe parenchymal destruction. The disease's severity and course are mainly determined by the interaction between the host's immunological system and the fungus, along with the presence of comorbidities. Chronic pulmonary aspergillosis (CPA) presents with nonspecific manifestations and a prolonged course, that combined with low clinical suspicion, contributes to its high morbidity and mortality. Differentiating between CPA subtypes, such as aspergillomas, cavitary, and necrotizing forms, is complex and frequently complicated by overlapping features, given that they can evolve depending on the host's immunological state and treatment initiation. As a result, early diagnosis and treatment remain a challenge. This case highlights the importance of clinical suspicion in patients at risk, conducting proper testing, and prompt treatment. Furthermore, it exposes a striking radiological evolution as well as an uncommon surgical management, that could offer insights into alternative strategies for this challenging condition.
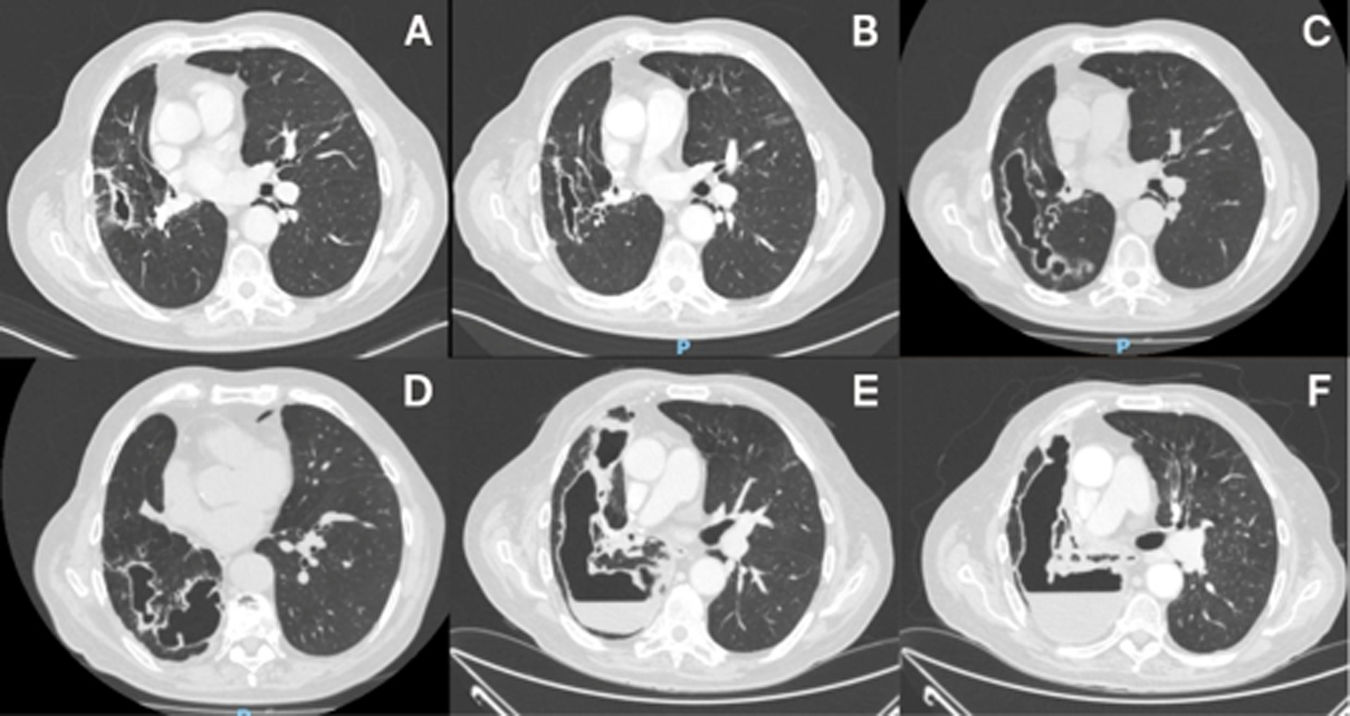
An 83-year-old male with chronic obstructive pulmonary disease and recurrent metastatic lung adenocarcinoma, previously treated with surgery, was receiving chemotherapy and immunotherapy. During follow-up, a nodule enlargement in the right lower lobe was treated with stereotactic radiotherapy, resulting in a 10cm cavity (Fig. 1A). Successive imaging revealed new multiple, irregular, destructive lesions in the treated location (Fig. 1B–D). The patient developed productive cough, hemoptysis, and fever, without improvement despite multiple courses of empirical antibiotics and corticosteroids. Amidst clinical deterioration, he was admitted to the hospital. A CT scan exposed enlarged coalescing cavities with liquid content (Fig. 1E and F). Bronchoscopy revealed elevated galactomannan levels and a positive culture for Aspergillus fumigatus in the bronchoalveolar lavage, and serological testing demonstrated elevated Aspergillus IgG levels. Chronic cavitary pulmonary aspergillosis (CCPA), a frequently overlooked and underdiagnosed condition, was diagnosed. Voriconazole 200mg twice daily with broad-spectrum antibiotics were initiated. Despite this, intracavitary drainage was required, obtaining purulent material. After discharge, the patient continued voriconazole for up to 6 months and died a year later from cancer progression with pulmonary, lymph node and bone metastases.
CPA is a chronic, destructive lung disease by Aspergillus fungus, mainly A. fumigatus,1–3 involving lung invasion in patients with a history of lung disease.1–5 It can occur in immunocompetent or mildly immunocompromised hosts.2,3,5 The prevalence of CPA is variable, with an estimated prevalence worldwide of 42 per 100,000.1 Nonetheless, it is likely underestimated given the underrecognition of the disease.1 CPA subtypes can evolve and overlap,1,3 with CCPA being the most frequent within the spectrum.5 Diagnosing CPA can be challenging since it requires the combination of persistent clinical manifestations for at least 3 months, radiological findings, and microbiological confirmation.1,4,5 Clinical presentation includes productive cough, hemoptysis,2,4,5 fever and fatigue.2,5 Radiological findings may include nodules, cavity formation,1,4 expansion or thickening of preexisting cavities, pleural thickening, and effusion.3,5 First-line treatment includes voriconazole and itraconazole1,3–5 for at least 6 months.4,5 Surgical treatment although uncommon, is reserved for cases involving aspergillomas,1,2,4 chronic necrotizing forms, massive hemoptysis,2,3,5 or when absence of response to antifungal therapy.4,5
Declaration of generative AI and AI-assisted technologies in the writing processThe material has been produced by the authors, without partial or total help of artificial intelligence software or tools.
FundingThis manuscript did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.