Pathologic upstaging (PU) in early-stage non-small cell lung cancer (NSCLC) after sublobar resection (SLR) remains challenging. Identifying risk factors may improve preoperative staging accuracy and patient selection. We conducted a retrospective cohort study evaluating predictors of PU and its impact on survival in 88 patients with clinical stage IA NSCLC who underwent SLR at our institution between 2019 and 2022. This study was approved by the institutional ethics committee (approval number: PR223/23), and informed consent was waived due to its retrospective design.
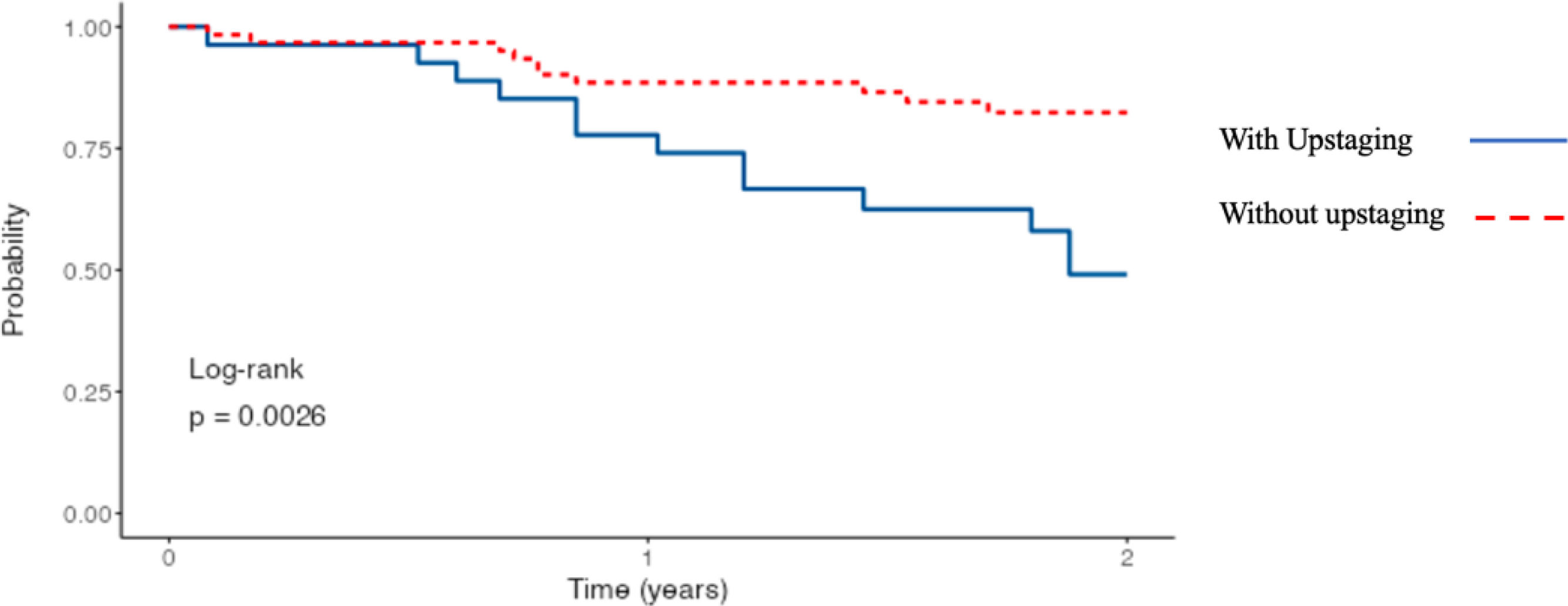
Patients underwent preoperative staging with high-resolution computed tomography (CT), positron emission tomography (PET-CT), and endobronchial ultrasound when indicated. Exclusion criteria were prior lung surgery, pulmonary metastases, previous oncological treatment, and poor surgical fitness based on multidisciplinary assessment. The decision between wedge resection and segmentectomy was based on tumor location, lung function, and patient comorbidities. PU was defined as upstaging to ≥pT2 or N1 based on final pathology. Logistic regression identified predictors of PU, and survival analysis utilized Kaplan–Meier curves.
PU occurred in 30.7% (n=27) of cases. Independent predictors included solid radiological lesions (OR=8.27; p=0.005) and visceral pleural invasion (VPI; p<0.001). Patients with PU had significantly lower 2-year disease-free survival (48.8% vs. 82.4%; p=0.0026) (Fig. 1) and lower overall survival (83.9% vs. 96.7%; p=0.050). The majority of unexpected PU cases were related to occult VPI rather than nodal involvement.
Solid tumor morphology and VPI significantly increase PU risk in early-stage NSCLC. While solid lesions on imaging represent true preoperative predictors, VPI is a postoperative histological finding and contributes to staging discrepancies. The prognostic importance of VPI is reflected in the latest TNM staging guidelines (9th edition).1,2 Careful attention to tumor margins, particularly in wedge resections, is essential, as previous studies link close margins to decreased disease-free survival.3 Despite the increasing adoption of SLR, lobectomy remains standard treatment for small tumors,4 and PU can significantly influence adjuvant therapy decisions.5
Limitations of this study include its retrospective nature, modest sample size, and short follow-up duration. Future prospective studies should explore advanced imaging modalities and biomarkers to refine preoperative staging accuracy.6
In conclusion, PU following SLR in early-stage NSCLC negatively impacts survival. Solid lesions and postoperative detection of VPI remain critical factors. Enhanced preoperative evaluation strategies are necessary to optimize patient selection and outcomes.
FundingNo external funding was received for this study.
Authors’ contributionsAll authors contributed to the study design, data collection, analysis, and manuscript drafting.
Conflicts of interestThe authors declare no conflicts of interest.