We present a case of exogenous lipid pneumonia treated with WLL and subsequent respiratory improvement.
Lipoid pneumonia is a rare interstitial lung disease (ILD) caused by the presence of intra-alveolar lipids. It is classified depending on the origin as endogenous or exogenous. Symptoms can vary from asymptomatic to severe. Possible complications include pulmonary fibrosis, respiratory failure and infections. The diagnosis is based on a history of oil exposure and the presence of foamy alveolar macrophages in a respiratory sample.1 Treatment protocols are poorly defined.2 A systematic review suggests whole lung lavage (WLL) as a treatment option for these patients.3
Our case is about a 64 year old woman, ex-smoker (50 packs a year since 2019) with obesity (BMI 38kg/m2), fibromyalgia, anxious-depressive disorder and chronic rhinitis. Consulted in our center (August 2023) with respiratory failure.
Patient was cataloged as asthma because of respiratory symptoms in 2019. In 2023, she needed hospitalization thrice in another center for respiratory failure and interstitial infiltrates. She was treated with corticosteroids 1mg/kg/day. Video-assisted thoracoscopic surgery (VATS) was performed.
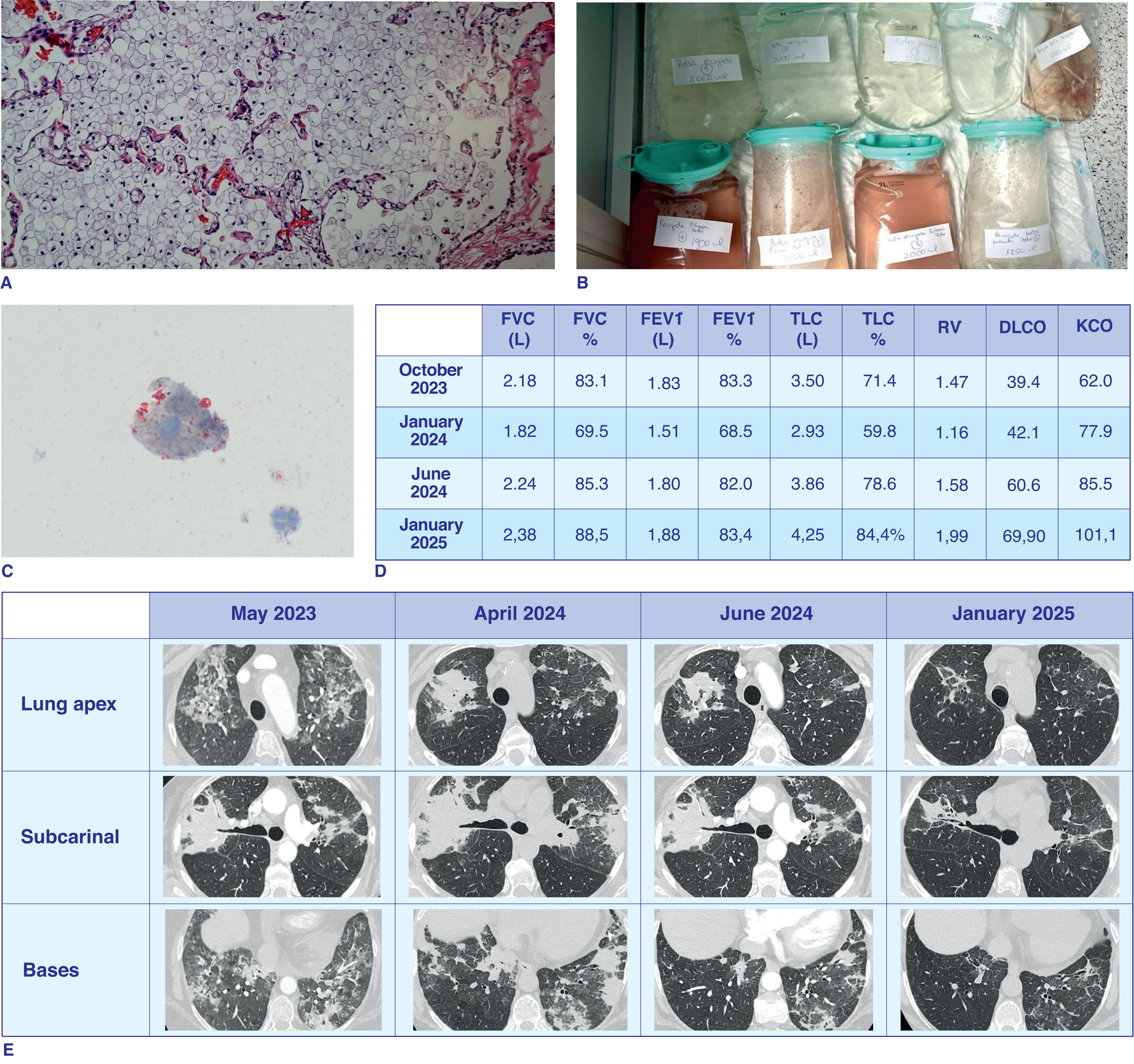
In August 2023 she was admitted due to respiratory failure and progression of lung infiltrates. Revision of VATS biopsy confirmed intra-alveolar foamy macrophages being diagnostic of exogenous lipoid pneumonia (Fig. 1A).
(A) Intra-alveolar lipids diagnostic of exogenous lipoid pneumonia obtained by lung biopsy (VATS) in July 2023. (B) Liquid obtained from the total BAL. Left lung. (C) Lipid drops obtained from a sample of the total BAL. (D) Functional evolution since August 2023 to July 2024. *FVC: Forced Vital Capacity, FEV1: Forced Expiratory Volume in 1second, TLC: Total Lung Capacity, RV: Residual Volume, DLCO: Diffusion Capacity of the Lungs for Carbon monoxide, KCO: Carbon monoxide Transfer coefficient. (E) Radiologic evolution from May 2023 to June 2024.
Patient admitted that she was abusing intranasal oxymetazoline (containing glycine) 4–6 times/day for rhinitis over the last 4 years. Corticosteroids were tapered until their complete stop in October 2023 and discontinuation of intranasal oxymetazoline was advised.
On follow up (November 2023) showed clinical, functional and radiological worsening. Patient confessed to continuing abusing intranasal oxymetazoline. We postponed WLL until she stopped using oxymetazoline.
Then, the patient lost 30kg in 4 months. A new thorax scan was performed (February 2024), showing parenchymal consolidations aggravation. Once assured no consumption of nasal oxymetazoline since November 2023, the multidisciplinary ILD committee discard malignancy and fungal infection with a PET/CT and transthoracic biopsy.
WLL was successfully performed in the critical care service over two consecutive days in May 2024. On the first day, selective intubation using a double-lumen endotracheal tube allowed for isolation and lavage of the right lung, during which 7l of warm sterile physiological saline were instilled and drained until the return fluid became cleaner. On the second day, a similar procedure was performed on the left lung, using a total of 8l of saline (Fig. 1B). RedOil dye showed intra-alveolar lipid-laden macrophages (Fig. 1C). As a complication the patient presented a respiratory infection treated successfully with amoxicillin for 7 days.
Clinical follow-up after the WLL (July 2024) confirmed clinical (no cough, no dyspnea, no use of oxygen on exertion and increase of weight), functional (Fig. 1D) and radiological improvement (Fig. 1E), which continue to ameliorate in the next follow up (January 2025, Fig. 1D and E).
Although exogenous lipoid pneumonia is a rare disease, WLL has shown promising results, as demonstrated in the review by Shang et al.3 In other cases, such as Wong et al.4 multiple treatments were required to see the improvement. However, in our case with just one WLL procedure and discontinuation of the lipid exposure, we observed a great clinical and radiological improvement.
In conclusion, we report a case of exogenous lipoid pneumonia caused by intranasal glycine. WLL in this case was safe and improved the respiratory clinical situation. A multidisciplinary expert team is needed to guarantee these results.
Informed consentThe authors declare that they have the patient's consent for publication.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsMP, SO and VVZ take care of medical management of the patients. LP and RL made the anatomical pathology diagnosis. BDR made the radiological diagnosis and MDF and MPFC made the WLL. MP and VVZ wrote the manuscript. All authors revised the final version of the manuscript.
Conflicts of interestThe authors declare not to have any conflicts of interest that may influence directly or indirectly the content of the manuscript.
Acknowledgements to patient, anatomopathological technicians from Pathology department, doctors and nursery from respiratory endoscopic Unit, radiology and critical care service for their support.