Obstructive mullerian anomalies are uncommon in gynecologic practice. Pelvic pain, abdominopelvic mass, and abnormal vaginal discharge are common symptoms.
Case reportWe describe a case of mullerian anomaly that was presented 9 years after menarche. Patient presented after delivery with offensive vaginal discharge and pelvic pressure 7 month after delivery without fever. She was diagnosed with bicornuate uterus, septate cervix along with obstructed hemivagina with pus collection and ipsilateral renal agenesis. She was successfully managed by transvaginal septum resection and drainage of pus.
Las anomalías müllerianas obstructivas son poco frecuentes en la práctica ginecológica. El dolor pélvico, la masa abdómino-pélvica y un flujo vaginal anormal son los síntomas más comunes.
Reporte de un casoSe describe un caso de anomalía de Müller que clínicamente se presentó nueve años después de la menarquia. La paciente se presentó después del parto con flujo vaginal fétido y con sensación de presión pélvica siete meses después del parto. A través de un estudio de resonancia magnética, a la paciente se le diagnosticó un útero bicorne, cuello del útero tabicado, junto con hemivagina obstruida con presencia de una colección de pus y agenesia renal ipsilateral. Su tratamiento establecido fue la resección quirúrgica del tabique transvaginal y el drenaje del absceso.
It is difficult to estimate the exact incidence of Uterus didelphys with obstructive hemivagina and ipsilateral renal anomaly as it is a rare congenital abnormality but it is reported to be around 0.1-3.8%.1,2 It is difficult to diagnose this condition due to variable presentation and variations regarding the age at diagnosis. It may be undetected early in reproductive years and present after sexual activity or when childbearing is attempted. Diagnosis time and clinical presentation are affected by level of obstruction and degree of completeness of the uterovaginal obstruction.
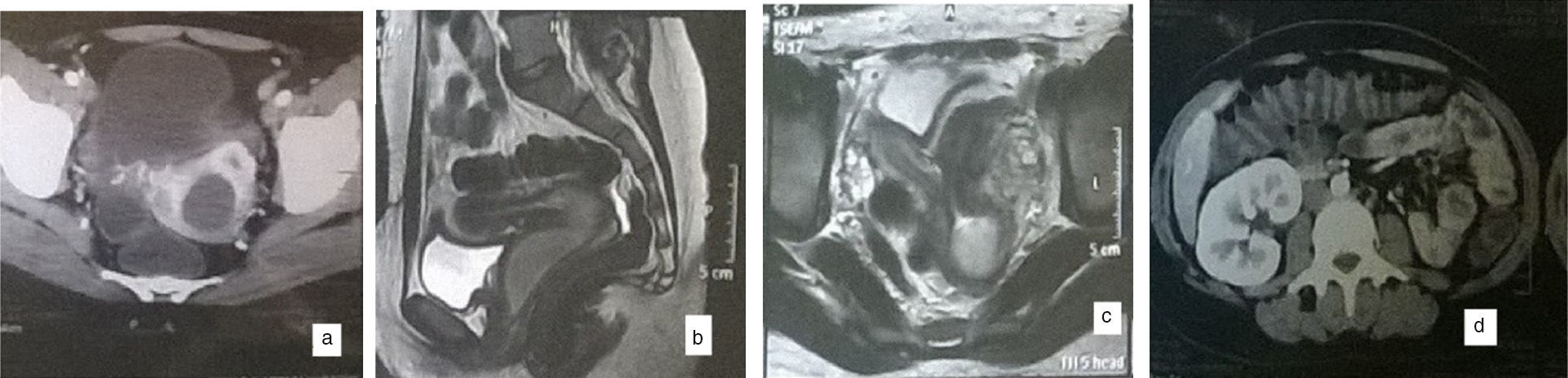
Case reportA 21 years old female, Gravida 1Para 1, previous I cesarean section, lactating on minipills presented to the gynecology department with lower abdominal pain and foul smelling discharge per vagina since four months. Her last menses was at end of puerperium. She had delivered since 7 months. Her operative data were not available as she delivered in a private hospital. She sought medical advice but she was not diagnosed correctly but managed as PID and tub-ovarian abscess. Computerized tomography was done revealing non visualized left kidney with compensatory hypertrophy of the right side. Uterine didelphus with oblong cysic mass along left hemivagina and left hemicervix as a sequel of obstructed hemivagina (Fig. 1). Magnetic resonance imaging revealed bicornuate bicollis uterus with turbid fluid collection in left cervix and vagina measuring 8cm×3cm suspicious of infected fluid collection (Fig. 1).
She was vitally stable. Abdominal examination revealed tenderness in left iliac fossa with no palpable mass. Vulval inspection revealed purulent vaginal discharge. Swab was taken for culture and Sensitivity. Vaginal examination revealed cervix felt high up and to the right side, cephalad, very adjacent and posterior to a tender cystic mass of about 10cm on the left side, uterine body was normal in size with purulent discharge drained on pressure on the mass. Laboratory investigations showed normal hemoglobin level, white blood cell count was 17,000 with neutrophilia with normal renal function tests. USG revealed uterus didelphys with a large cystic collection of 10cm with air inside on the left side and posterolateral to the bladder. Normal ovaries and absent left kidney were detected. Obstructive mullerian anomaly was suspected.
Antibiotics were started and surgery was planned after 48 h under regional anesthesia.
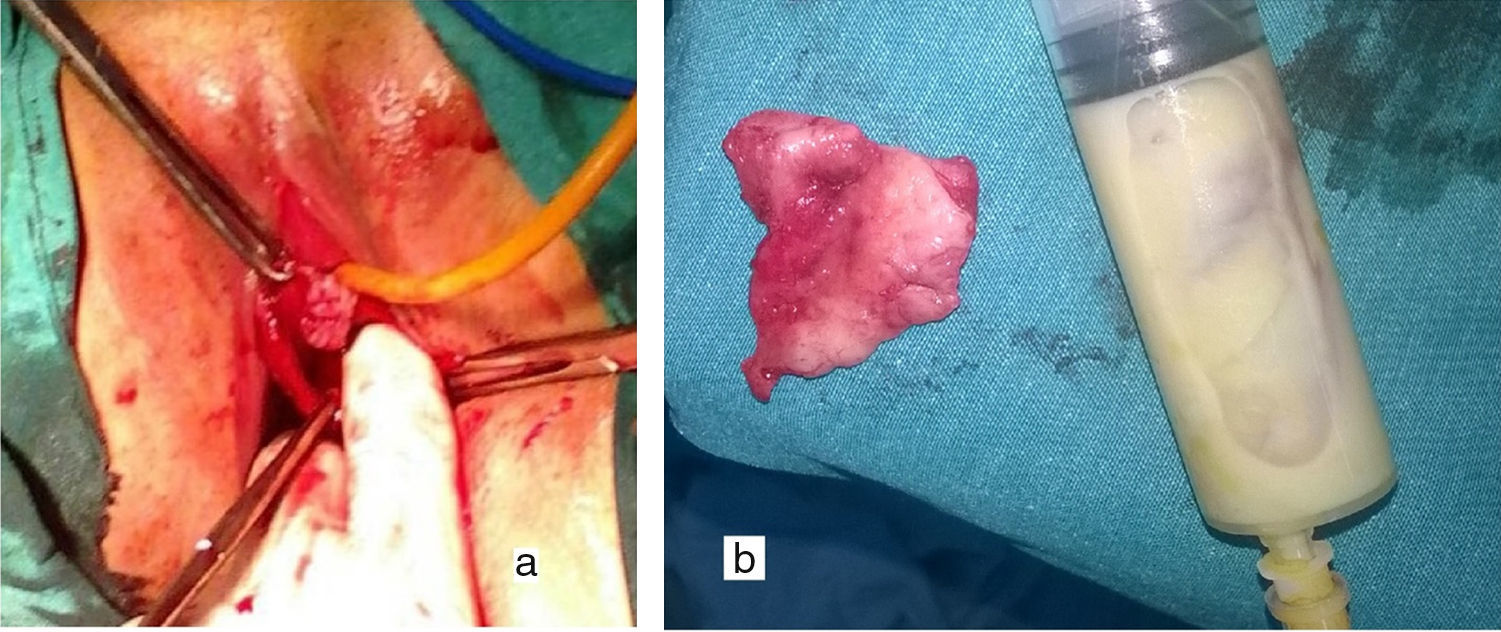
Left lateral vaginal mass was palpated. Foley's catheter was placed to identify the limits of the bladder. The left paravaginal mass was 5cm from hymen intraoperatively. Cruciate incision was done transvaginally, between the bulge and vaginal mucosa in a dependent site after aspiration from the bulge revealing pus with no fistula on the longitudinal septum detected, and 200ml of foul smelling, purulent material was drained out and specimen was sent for culture and sensitivity. Digital palpation through the incision determined the extent of the septum. It was excised with electro cautery until the cervix was reached which was a single body with a septum dividing the external os (Fig. 2). Fine absorbable sutures were placed on the resected septum. Postoperative period was smooth. The excised specimen was sent for histopathology excluding vaginal adenosis. Coitus was allowed after 2 weeks.
DiscussionUterus didelphys, obstructed hemivagina with ipsilateral renal anomaly is a well-Recognized syndrome as Herlyn Werner Wunderlich syndrome.1,3,4 The acronym obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) is used now to describe two out of the three of the triad5 including uterine anomalies other than uterus didelphys, as septate and bicornuate uterus as our case. It occurs in about 20% of cases.
Uterus didelphys results from complete failure of lateral fusion of the paramesonephric ducts with incomplete fusion and resorption leading to bicornuate and septate uterus. Partial or complete vaginal septum is due to vertical fusion defect with the urogenital sinus. Associated arrest in metanephric ducts usually leads to renal tract abnormalities.6
Obstructed hemivagina leads to hemato-metro-colpos and reverse menstruation effects as endometriosis and pelvic adhesions. Cyclic abdominal pain, lower abdominal mass,7 dyspareunia, and abnormal vaginal discharge are among the symptoms. The vaginal collection with blood can be infected.2 History of regular menstrual cycles is reported by some patients and can be asymptomatic for years after menarche. Our case was diagnosed late maybe for the small fistula that became occluded by blood clot, from postpartum hemorrhage or remnants of conception and became infected with time.8 Diagnosis requires high clinical suspicion. Magnetic resonance imaging (MRI) is the gold standard in the diagnosis.2 It identifies associated tubo-ovarian pathologies, the thickness and location of the septum, the type of collection, and associated malformations of the urinary tract. The treatment is complete resection of the vaginal septum especially under laparoscopic or ultrasound guidance. Transvaginal resection can be performed as a single or a double stage procedure especially in infected cases where 2cm incision is done with excision of part of the septum, and after 2 month reassess and remove the rest after resolution of edema and infection.5 Laparoscopy prior to resection rules out adnexal pathology and confirm the diagnosis if MRI is not feasible. Resection under laparoscopic control avoids and detects bladder injury as the paravesical anatomy is distorted. Hysteroscopic vaginal septum resection under transabdominal ultrasound guidance can be done in young females to preserve the hymenal integrity.9 The surgical outcome is good with successful reproductive performance in future life.2,3,10–12
ConclusionsImaging methods need high expertise in assessment of mullerian anomalies. Renal anomalies should be screened for with mullerian anomalies. Vaginal compartment with collection may be mistaken for adnexal masses on ultrasound in unexperienced hands. Ultrasound should be assessed with clinical examination in less experienced sonographers. Obstructed hemivagina may present with no amenorrhea especially after delivery with obstruction of communicating canal pyocolpos may follow hematocolpos.
FundingThis study was not funded.
Ethical approvalAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentInformed consent was obtained from the patient included in the study.
Authors’ contributionsEl-Agwany had done the diagnoses and surgery along with writing the article.
Conflict of interestThe author has nothing to declare.