Portugal is characterized by a high prevalence of overweight and obesity among women, whose weight increases most rapidly in early adulthood. Individual genetic features and behaviours, along with social, cultural and environmental factors interact in complex relationships with body weight and with its variation throughout time. Motherhood may trigger an increase in weight, potentially influencing the associations between excessive weight and several other health determinants. Taking into account the quality of prenatal care within Portugal's health care system, regarding coverage and success in improved outcomes, we theoretically demonstrate why pregnancy and motherhood should be seen as opportunities for prevention and why a deeper knowledge about the interplay of biological, social and psychological determinants of weight at this stage of life can be useful to design more effective weight control interventions towards this population.
Motherhood is one of the most challenging experiences that can occur in women's life and it can be concomitantly distressing and meaningful. These ambivalent feelings are not necessarily a problem, but more research is needed to understand their specificities and how they can interact with weight management in this period of life. The growing number of obese women worldwide has many implications, not only on mother's health outcomes but also for their children, as demonstrated by the association between prepregnancy obesity and certain major birth defects1 and a higher likelihood of having macrosomic infants.2 Additionally, caesarean delivery risk is increased by 50% in overweight women and is more than double for obese women compared to women with normal body mass index (BMI).3
The postpartum period can be critical for the development of obesity in midlife. Evidence consistently shows that excessive gestational weight gain (GWG) contributes to higher postpartum body weight4–6 and that overweight and obese women have more than double the chance to exceed the weight gain recommendations during pregnancy than other BMI groups.2,7 Moreover, excessive GWG is associated with abdominal adiposity 8 years after delivery, which may increase a woman's risk of cardiovascular and metabolic diseases.8
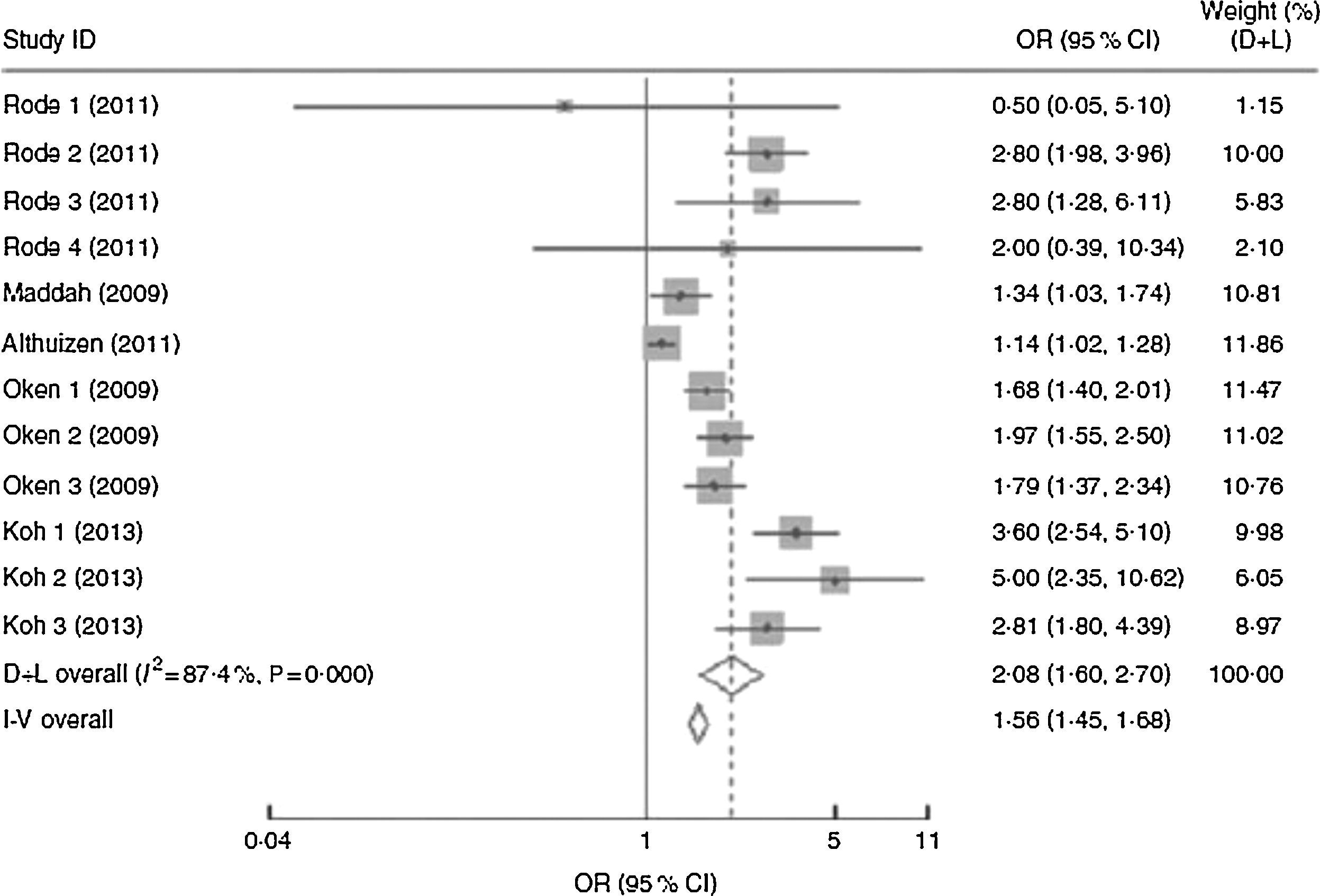
Several pregnancy cohort studies from developed countries have reported independent direct associations between prepregnancy body weight or BMI and postpartum weight retention.9,10 However, a recent meta-analysis analyzed the association of GWG or prepregnancy BMI with postpartum weight retention and, as illustrated in Fig. 1, GWG, rather than prepregnancy BMI, determines the shorter- or longer-term postpartum weight retention. When postpartum time spans were stratified into 1–3 months, 3–6 months, 6–12 months, 12–36 months and ≥15 years, the association between inadequate GWG and postpartum weight retention faded over time and became insignificant after 15 years.11
Forest plot of the studies on the risk of postpartum weight retention of ≥5kg for women with excessive gestational weight gain (GWG) vs. women with adequate GWG. The study-specific OR and 95% CI are represented by the grey square and horizontal line, respectively; the size of the data marker (grey square) is proportional to the weight of the study in the meta-analysis (note: weights are from random-effects analysis). The centre of the open diamond presents the pooled OR and its width represents the pooled 95% CI.11 Reprinted with the permission of Cambridge University Press.
Most studies conducted so far focus on weight change only until the first year postpartum, and few studies have obtained serial measurements for longer periods to assess patterns of weight change. Characterization of the interrelationships between prepregnancy body weight, GWG and postpartum weight retention is essential for a deeper knowledge of weight changes after pregnancy and obesity rates in childbearing age. Given the modifiable nature of this risk factor, the preconception, prenatal, and postpartum periods may present critical windows to implement interventions to prevent weight retention and the development of overweight and obesity in women of childbearing age.12
Increasing parity contributes to the long-term development of obesity in women13–15 but this relationship differs by maternal BMI in young adulthood, number of births, race-ethnicity and length of follow-up. Findings from a representative cohort from the United States of America (USA) showed that black and white primiparae and multiparae tended to have greater BMI increases than nulliparae over 10 years, this association being stronger among women with high BMI before pregnancy. However, 25 years later, the same study showed that only black women who were overweight at baseline and delivered more than one child gained significantly more weight than those not giving birth.16 Women often report their obesity to be triggered by pregnancy – as many as 40–50% in one Swedish study. Yet, for 30% of the women in the same study, pregnancy was associated with weight loss.17 Additionally, place of residence, ethnicity, as well as individual socioeconomic position (SEP) and lifestyle factors can considerably explain this association.18,19 All of these data allude to a complex parity–weight relationship for women with a range of confounding factors that act across the life course, with the possibility for further variations.20 Thus, further research is needed to confirm the links between parity and weight gain, as well as more information regarding confounders of this association framed in social and current economic conditions.
The risk of weight gain is not equal throughout all pregnancies. In large cohort studies, when comparing nulliparous with primiparous women, weight gain due to childbearing was greatest after the first birth, and weight gain was greater with increasing baseline maternal body weight. Average weight gain associated with having a first child was 3–6kg among women who were overweight before pregnancy, and about 1kg among women with normal BMI. After the first pregnancy, weight gain is smaller in subsequent pregnancies.12,21,22 Furthermore, multiparity is positively associated with abdominal girth from preconception to several years after delivery.21,23
Despite some disparities, evidence supports that substantial weight gain associated with childbearing is an important risk factor for the development of overweight and obesity in adult women. Future studies should identify women more susceptible to benefit from interventions to prevent weight gain and which are the critical periods to intervene most effectively: before, during or after pregnancy.
The impact of psychosocial determinants on weight, around motherhoodSince social10 and psychological characteristics24 have impact on maternal excessive weight, the psychosocial context should be studied in depth. A review of the implications of body image and socioeconomic position is provided below.
Body imagePregnancy, due to its concomitant changes in body size and shape, can have a significant impact on a woman's body image.25 This is often the first time weight gain is expected and accepted and some women view body changes as transient and unique to the childbearing endeavour so they are able to assimilate these changes without distress.26
Research results on body image in pregnancy have been contradictory, with some studies highlighting that women are able to assimilate the bodily changes of pregnancy without a negative shift in body image satisfaction (BIS),27,28 and other studies finding a decreased BIS during pregnancy29 and postpartum.30 Also, prepregnancy BMI has an impact on BIS during pregnancy, with overweight women reporting an increase in their satisfaction and women with normal BMI reporting a decrease.29 Those who had been overweight before their pregnancy may view their pregnancy as excusing them from unpleasant comments or feeling uncomfortable in activities exposing their body, such as swimming.31
In the postpartum period, despite some variation, body image is generally more negative, when women's constructions of their postpartum body indicate that once the baby was born, they no longer perceived any excuse to not adhere to their perceived socially constructed ideal silhouette.32 Harris and colleagues also found that women who were less satisfied with their bodies postpartum had significantly greater long term weight gains than those women who displayed no increase in dissatisfaction with their bodies after pregnancy.14 One possible reason for this disappointment is that women (especially primiparous women) tend to expect that their bodies will return to their pre-pregnancy weight and shape shortly after the birth of their child.33
A recent review synthesized the existing qualitative literature describing women's experiences of their pregnancy and postpartum body image. Hodgkinson and colleagues25 highlighted that women's perception of their pregnancy body image is varied and depends on the strategies they use to protect against social constructions of female beauty. Women often perceived the pregnant body to be out of their control and as transgressing the physical manifestation of the socially constructed ideal, against which they tried to protect their BIS. Body dissatisfaction dominated the postpartum period, emphasizing the women's need for additional support at this moment. Moreover, health professionals are reported to feel uncomfortable about discussing weight as an aspect of body image due to lack of knowledge and fear of being considered insensitive.34 However, since during pregnancy women are more receptive to conversations about weight-related aspects of their body image, communication skills training could increase professionals’ confidence in exploring women's body image in order to improve their weight management strategies independently of their BMI.25
While it seems clear that BIS before pregnancy has a considerable impact on postpartum weight changes, further research is needed to assess if this same construct can influence weight over a longer-term.
Socioeconomic positionFemale reproductive health is highly sensitive to the physical and social environment throughout life. Women are currently less likely to be married and more likely to be single or cohabiting,35,36 more women are remaining childless or having fewer children and the proportion of women's lives spent rearing their children has been reduced.37 If social factors change, their impact on women's reproductive life can also change; therefore, a deep study of this relation, together with psychological and biological attributes, is still a challenge to be faced.
Maternal SEP is known to be a strong correlate of numerous maternal and child health outcomes. Low individual SEP (e.g. education and income) has been associated with adverse pregnancy and birth outcomes38,39 and delayed prenatal care.40 A recent large population-based study compared the direction and magnitude of individual and neighbourhood social inequalities across multiple maternal and child health outcomes (maternal and infant health status indicators; prenatal care; maternal experience of labour and delivery; neonatal medical care; and postpartum infant care and maternal perceptions of health care services) and revealed that SEP measures had stronger associations with outcomes belonging to the health status of the mother and infant, as opposed to the other groups. The magnitude of maternal and child health inequalities was higher when individual-level SEP was used than when considering neighbourhood SEP. In particular, education showed the greatest gradients compared to household income, neighbourhood SEP, and combined SEP (combination of low and high individual and neighbourhood SEP).41
A relation between SEP and obesity has been well established for a long time,42 also in childbearing women,43 with those who have a lower SEP being the ones with a higher risk of being obese. However, some specificities of this association considering young adult women remain unclear. In adulthood, reproduction may have an added influence on obesity risk in women, although research is lacking on how adult influences combine, namely social and psychological ones, for the development of excessive weight in this particular period.
Additionally, research on childhood growth has pointed to the possibility that early life may be an important stage in the development of obesity and longitudinal studies consistently show that a lower SEP in childhood increases the risk of excessive weight in adulthood.44 These associations between childhood SEP and adult health are also observed in the context of motherhood. In the British 1958 birth cohort study,45 it was observed that, as the level of poverty in childhood increases, the proportion of women having their first baby by the age of 20 also increases.
This continuity in disadvantage throughout life is an important part of the link between childhood disadvantage and poor adult health, with SEP across childhood and adulthood emerging as a stronger predictor of adult health than SEP at any one point in time.45
Social trajectory is a lifelong evolution of the volume and composition of an individual's capital (social, cultural, economic and/or symbolic), combined with his/her parents’ asset volume and structure and can be described as upward, downward or stationary.46
Most of the findings concerning obesity and socioeconomic characteristics have been based on women's SEP in adulthood but, recently, evidence is emerging about the impact of intergenerational social trajectory taking into account a life course perspective. In order to study the influence of social class in childhood, young adulthood and middle age, and intergenerational mobility, on adult central and total obesity, a study was conducted using a population-based birth cohort. In women at 53 years, father's social class was inversely associated with all measures of obesity, both adult social classes (at ages 26 and 43 years) were inversely associated with all obesity measures at age 53 and women with an upward intergenerational social mobility had lower levels of central and total obesity compared with those who remained in the same social class as their father.47
Changes in social circumstances, or intergenerational movement between social classes, might entail a transition in terms of priorities and resources related to weight and appearance, or a shift in experience of social norms regarding the appeal of particular body types,48 particularly when considered in the context of women who have recently given birth. Knowing that society influences women's perception of good or bad appearance, future studies should better assess the social determinants of BIS in childbearing women, considering a life course approach.
Motherhood as an opportunity for preventionSome authors defend that the preconception period should be seen as a privileged time for prediction and prevention of noncommunicable diseases, thus not only improving pregnancy outcomes and maternal health, but also promoting long-term beneficial effects for both the mother and the child.49 Prepregnancy weight loss can reduce obesity-related complications, which can have a considerable impact on improving obesity-related perinatal complications – gestational diabetes mellitus, hypertensive disorders, macrosomia, and large for gestational age babies.50
Women's health in Portugal has experienced a huge overall improvement since the late 1970s and the implementation of the National Health System, which ensures all citizens nearly free access to primary care centres and public hospitals.51 Moreover, prenatal care is one of Portugal's health care system's most successful areas, with practically 100% coverage and adequate prenatal care in the vast majority of pregnancies.52 However, a study performed in the north of the country showed that, whilst good prenatal surveillance exists, only 27% of the puerperal women had preconception care.53 Also, a study performed in mothers of the Generation XXI birth cohort showed an adverse cardiovascular risk profile since the preconception period,54 supporting the idea that interventions should start earlier in childbearing women.
The label “teachable moment” has been used to characterize life transitions or health events that increase perceptions of personal risk and outcome expectancies, prompt strong affective or emotional responses, and redefine self-concept or social roles. In other words, a cognitive response precedes motivation, skills acquisition and self-efficacy that in turn, increase the likelihood of ceasing adverse lifestyles. Additional key factors to consider are predisposing factors such as age, dispositional and cultural characteristics that may influence an individual's cognitive and emotional response. Pregnancy has been widely referred to as a teachable moment because of mothers’ strong motivation to protect the well-being of the foetus and strong social pressure to avoid unhealthy habits, such as smoking during pregnancy.55,56
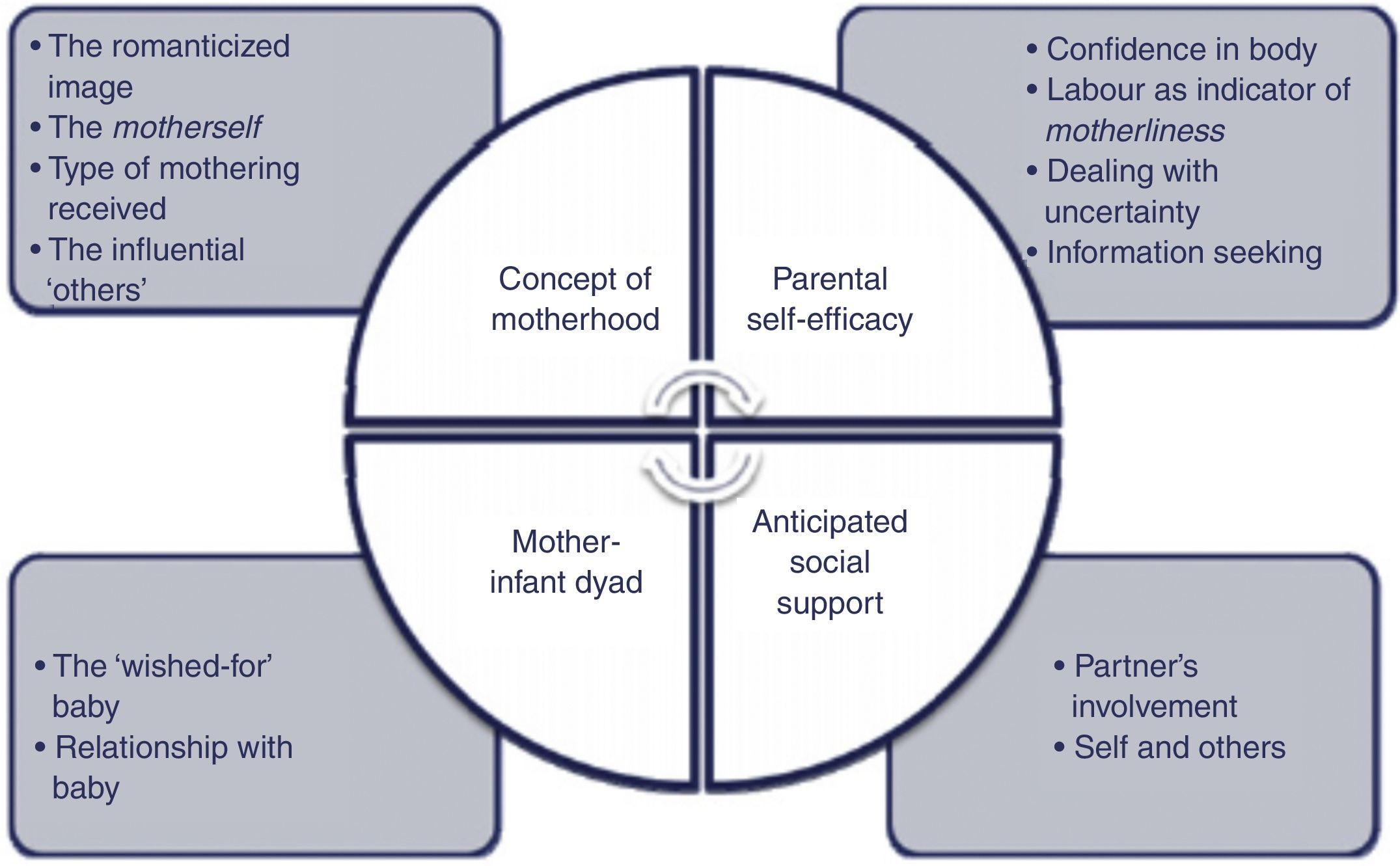
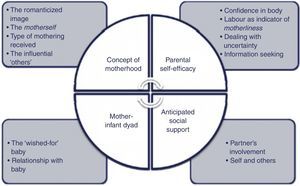
Some psychological issues should also be highlighted when discussing a pregnancy's impact on women's life. A qualitative study explored beliefs and expectations about motherhood, and the main themes are illustrated in Fig. 2. Since a discrepancy between women's expectations and reality was found, a psychological preparation for motherhood should be considered when preparing women for their new role. Such preparation promotes a sensible image of motherhood, the infant, the novelty of the future and relationships with others, and discussing these themes may be particularly relevant to women vulnerable to postnatal psychological adjustment difficulties.57
Themes and sub-themes identified within the ‘Expectations and beliefs about motherhood views’.57 Reprinted with the permission of Elsevier.
According to a study performed in the United Kingdom between 1998 and 2003, there was a significant reduction in smoking, alcohol consumption and intake of caffeinated drinks when women became pregnant, although little change occurred in fruits and vegetables intake.58 In Portuguese mothers, although almost half of smokers ceased tobacco consumption during pregnancy, approximately two thirds resumed smoking within 4 years after delivery,59 leading us to believe that, although pregnancy enhances the perceived need of adopting healthy lifestyles, that does not mean that healthy habits will persist throughout time. Since fertile age women are prone to change healthy habits when they receive health care provider's advices,60 interventions to this segment of the population should be restructured, focusing more on women's intrinsic motivations and expectations, which is proved to result in long-lasting behaviour change.61
In summary, weight management before, during and after a pregnancy has advantages for both mother and child. Monitoring of prepregnancy BMI, GWG, and postpartum weight will allow the identification of women who are more susceptible of having an inadequate weight throughout childbearing years. Preconception is an important period and obese women should be targeted for intervention before they get pregnant for the first time. Likewise, healthcare providers involved in the care of pregnant women should be trained to provide a more effective approach for weight control.
Metabolic features after pregnancy: the healthy obesity phenotypeThe numbers regarding obesity are alarming, largely due to its association with several cardiovascular diseases. However, a healthy obese phenotype has been recently identified and these individuals appear to be at no increased cardiovascular risk.62,63 This clinical condition, termed benign obesity or metabolically healthy obesity, is restricted to a unique subset of the obese population which, despite excessive BMI, are insulin sensitive and have a normal blood pressure, lipid, inflammation and hormonal profile.62–66 The relevance of establishing such a phenotype is underlined by data that suggests that weight loss among healthy obese may adversely impact their favourable cardiometabolic profile.67
The absence of a uniform definition for this subtype of obesity is one of the main limitations of this topic, with prevalences ranging from 6% to 37%,68–70 depending on the criteria to define the phenotype. However, even when unique criteria are used, considerable variability in the prevalence of healthy obesity is found across different European countries71 and, to the best of our knowledge, there are no estimates for Portugal. Normally, metabolically healthy obese persons have family members with uncomplicated obesity, early onset obesity, fasting plasma insulin within a normal range and a normal distribution of the excess fat.72 Additionally, some lifestyle features are associated with this metabolic profile, such as moderate and higher levels of physical activity and higher dietary quality.70
Some controversy exists considering the relevance of this phenotype. A recent systematic review and meta-analysis showed that, compared with metabolically healthy normal weight individuals, obese persons are at an increased risk of adverse long-term outcomes even in the absence of metabolic abnormalities, suggesting that there is no healthy pattern of increased weight.73 Also, another study that evaluated the 3-year incidence of cardiometabolic risk factors concluded that an increase in BMI during the follow-up period was significantly associated with the occurrence of cardiometabolic alterations.74 More research concerning this subject is still needed and longer longitudinal analyses should be provided in order to clarify if these individuals are protected during their entire life or whether healthy obesity simply represents delayed onset of obesity related cardiometabolic problems. Also, most of the studies that assessed healthy obesity used samples comprising women above 40 years of age66,75,76 and information concerning childbearing women is still lacking.
The increase in deposition of fat in abdominal visceral adipose tissue is favoured after pregnancy, due to increased abdominal compliance, rendering women more susceptible to abdominal obesity after childbirth.13 Abdominal fat distribution, visceral and ectopic fat accumulation are also key characteristics for the development of unhealthy obesity.77 Thus, it would be interesting to characterize the obesity phenotype in women who had a child, to assess to which extent their obesity is healthy or is conveying a higher risk of CVD, thus supporting or not the need for preventive action directed at this segment of the population. Further studies examining different subtypes of obesity will allow for understanding obesity's heterogeneous nature that could result in more appropriate weight loss recommendations, even among childbearing women.
ConclusionIn conclusion, the accumulated evidence suggests that there are several factors that could lead a childbearing woman to be overweight or obese and a biopsychosocial approach contributes to understand these relations comprehensively.
Pregnancy has been widely referred to as a teachable moment and future research should identify women more susceptible to benefit from interventions to prevent weight gain during this period, preferably, starting at the preconception period. BIS, socioeconomic economic characteristics across the lifespan and metabolic features should be considered when designing future interventions for weight management targeting this specific population and longitudinal research is needed in order to assess if the impact of these variables on weight is observed throughout time.
Conflicts of interestThe authors declare no conflicts of interest.
A grant from Fundação para a Ciência e Tecnologia is gratefully acknowledged (SFRH/BD/72723/2010).