Pasteurella species are a component of the normal oropharyngeal flora in canine animals. In humans, the skin and soft tissue are the most common sites for Pasteurella infection and, less commonly, the respiratory tract can also be affected. We report a case of pneumonia by Pasteurella canis in a chronic respiratory disease patient with a history of permanent contact with a dog.
Pasteurella is a genus of the Gram-negative bacteria which belongs to the Pasteurellaceae family, in which the species are small, nonmotile, nonspore-forming, facultatively anaerobic, and generally appear as a single bacillus. Nonetheless, they may also be found in pairs or short chains.1
The members of this genus are primarily commensals or pathogens of animals. In humans, they are known to cause zoonotic infections which have been described from Pasteurella multocida (the most commonly isolated), Pasteurella canis, Pasteurella dagmatis and Pasteurella stomatis. Most human infections are caused by dog or cat bites, although licks from these animals have also been associated with infection.1
Case reportAn 89-year-old Caucasian male was presented to the emergency room (ER) with a history of productive cough and dyspnea which lasted for several weeks. There was no mention of fever. The examination in the ER demonstrated that the respiratory rate was 28breaths/min with a peripheral oxygen saturation of 90%, the blood pressure was 122/78mmHg, the heart rate was 88beats/min (irregular pulse) and the auricular temperature was 37.7°C. The Glasgow Coma Scale was 14 (E4V4M6). The lung auscultation showed bilateral rhonchi, with an increased expiratory time, while the cardiac auscultation revealed a systolic ejection murmur.
Laboratory exams revealed hemoglobin of 12.0g/dL, leucocytes of 19.13×109/L (neutrophilia of 17.31×109/L), urea of 52mg/dL and creatinine of 1.07mg/dL, C-reactive protein of 368.5mg/L and lactates of 1.50mmol/L. The blood gas analysis revealed a hypoxemic respiratory failure (paO2/FiO2 ratio=291) and the chest radiography demonstrated bilateral interstitial/alveolar infiltrates (Fig. 1). Two blood cultures were collected and empirical antibiotic therapy with ceftriaxone (2g/day, intravenously) and azithromycin (500mg/day, intravenously) was established, assuming the diagnosis of community-acquired pneumonia with severity criteria (PSI=119 and CURB-65=2). The patient was admitted to the Internal Medicine ward.
To what concerns the previous medical history, the patient has an unstudied chronic respiratory disease, possibly related to his smoking history, valvular heart disease, atrial fibrillation, chronic kidney disease, cerebrovascular disease, hypertension and dyslipidemia. Regarding the epidemiological context we emphasize the poor social environment and a close and prolonged contact with a dog, with no history of bites. There was no history of antibiotic therapy nor any contact with the healthcare system within the last 3 months.
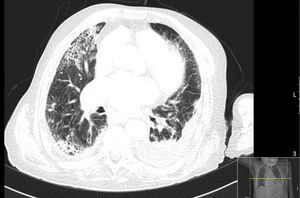
The chest CT revealed pulmonary emphysema, a left pleural effusion of minor volume with an uptake of the pleural surfaces suggesting that it was an exudate, consolidation/atelectasis of the lung adjacent to the pleural effusion and bilateral ground glass opacities (Fig. 2). It was decided not to perform a diagnostic thoracentesis as it would be an invasive and technically difficult procedure (pleural effusion showed a small volume). Thus, it was assumed the definitive diagnosis of community-acquired pneumonia with probable parapneumonic pleural effusion.
Taking into account the initial unfavorable clinical course, particularly the worsening of the respiratory failure, the microbiology laboratory was contacted on the 3rd day of hospitalization, and we were able to obtain provisional information that there was colonies growth with a morphology suggestive of Brucella in the two blood samples. A bacteriological examination and culture of respiratory secretions was not performed because the patient was already undergoing antibiotic therapy and because of a probable low diagnostic yield. The echocardiogram showed no signs of endocarditis. The antibiotic therapy was changed to doxycycline (100mg 2 times a day, orally) even though there was still no definitive microbial identification of Brucella, but also taking into account the epidemiological context and radiological profile showing bilateral opacities (although pneumonia is a rare form of presentation of brucellosis). These facts led us to consider the possibility of unusual microbiological agents as being responsible for the pneumonia.
On the 8th day of hospitalization, it was known the final result of the blood cultures with the identification of P. canis by VITEK® 2 system (there was no automatic antimicrobial susceptibility testing available and, taking into account the clinical stability of the patient with the prescribed antibiotic therapy, no manual susceptibility testing was performed). The control blood cultures (on the 6th day of doxycycline) were negative and the patient completed 21 days of antibiotic therapy after culture conversion (10 days of doxycycline that was changed to oral levofloxacin 750mg/day due to gastrointestinal intolerance). The clinical outcome was favorable.
DiscussionP. canis infection is a rare entity, particularly the respiratory infection or bacteremia. After a review of the literature we found three cases of bacteremia and only one case with the diagnosis of pneumonia.2–4
P. canis is a species that typically does not affect humans and is usually transmitted through animal bites or licks. Nonetheless, some patients develop infections after other animal exposure.1 The skin and soft tissue are the most common site for Pasteurella infection and, less commonly, respiratory infections, septic arthritis, osteomyelitis, endocarditis, meningitis and peritonitis may occur. The clinical course of Pasteurella respiratory tract infections is nonspecific and the onset of the illness may be gradual or abrupt.1–3 We emphasize that the accuracy rate of the VITEK® 2 system for identification of Gram-positive bacteria is greater than 90%, but no data are available regarding the identification of Pasteurella spp. specifically.5
In this case there was no bite history or skin lesions, only a close and permanent contact with a dog. However, the epidemiological context, the gradual onset of the illness and the radiological pattern were considered suggestive of a less common microbiological agent (e.g. Coxiella burnetii, Francisella tularensis, Brucella spp., Pasteurella spp., Yersinia pestis) which allowed us to have an appropriate antibiotic coverage since the 3rd day of hospitalization.
Immunocompromised individuals (including those with cirrhosis, hematologic malignancies, or solid organ transplantation) and the extreme ages of life are particularly at risk for Pasteurella severe infections, even though they can also occur in healthy individuals. Comorbidities that increase the risk of particular Pasteurella infections include a prosthetic joint for septic arthritis, underlying lung disease for pneumonia, and peritoneal dialysis for peritonitis. Most patients with Pasteurella pulmonary infection are elderly with pre-existing chronic lung diseases like chronic obstructive pulmonary disease.1,6
Pasteurella spp. are usually susceptible to several antibiotics including penicillin, amoxicillin/clavulanate, piperacillin/tazobactam, cephalosporins (e.g. cefixime, ceftriaxone, ceftaroline), carbapenems, doxycycline, fluoroquinolones and trimethoprim/sulfamethoxazole.1,2,7 In this case, because there are no clinical trials evaluating specifically the efficacy of different antibiotic agents for Pasteurella infections, the antibiotic strategy was maintained.
Data on the management of Pasteurella pulmonary infections are limited to case reports and the duration of therapy is generally the same as for other infections at the same site.2 In this case, taking into account the slow clinical response (particularly with regard to respiratory failure), the unusual and less common pathogen involved, the severity of the disease (with bacteremia) and because it was not possible to exclude that it was an empyema, the duration of the antibiotic therapy was extended.
This case highlights the particular importance of a detailed epidemiological history, especially for animal exposure, and the need to be vigilant to less common microorganisms in order to get the right diagnosis.
Conflicts of interestThe authors declare no conflicts of interest.