Due the increase incidence of Dementia, the creation, implementation and evaluation of the effectiveness of training programmes for family caregivers of people with dementia living at home should be a goal of health professionals. The aim of this paper is to describe the randomised control trial protocol that will assess the effectiveness of the training programme for family caregivers who care for people with dementia at home “Living together with Dementia”.
MethodsRandomised control trial. Family caregivers of people with dementia in early and moderate stages will be recruited through a neurology appointment at the São João Hospital Centre, Porto-Portugal. The inclusion criteria employed will be as follows: to be the main caregiver of the person with dementia; to be literate; the care target has dementia in early or moderate stage; the person with dementia does not suffer from any other severe mental pathology. Caregivers will be randomised and assigned to control and experimental groups. 3 assessment moments will take place: initial, after the intervention and a follow up of 3 to 6 months. The assessment instruments include a survey containing sociodemographic data, Caregiver Burden Scale, Caregiver Assessment Satisfaction Index and Caregiver Assessment Difficulties Index. The participants of the experimental group will be submitted to a 7-week individual psychoeducational programme. The study was approved by the Health Ethics Committee of the São João Hospital Centre in September 2015.
DiscussionThis programme might prove an asset to family caregivers of people with dementia living at home, since it pinpoints understanding and preparation of their role. It also facilitates the intervention of health professional, as it features as a guideline for their performance with this target population.
In the present sociodemographic context, dementia assumes itself as an emerging Public Health problem, and the involvement of family members in the assisting plan is increasing.1 Training family members who undertake the responsibility of caring for people with dementia who remain at home is paramount, so these acquire knowledge and skills to cope with the disease and its evolution.
In the early and moderate stages of the pathology, psychological and behavioural alterations are a main overload factor for family caregivers, since these lack strategies to manage these changes. So as to address this need, an increasing greater number of countries have been developing training programmes designed to assist family caregivers of people with dementia living at home. These sort of intervention are beneficial for the person with dementia, for the caregiver and for the health service, since institutionalisation is delayed.2
Diverse interventions with family caregivers of people with dementia are to be found in literature, such as family and personal counselling, psychoeducation, emotional support groups, skill training programmes, multiple component programmes, psychotherapy programmes, cognitive and behavioural programmes, and “technology” based interventions, among others.3 However, training a caregiver entails providing knowledge and skill, in which psychoeducation appears to be the most efficient type of intervention, due to the consistency of the results when it comes to the increase of the competences of the family caregivers and both overload and depression reduction.4,5
An integrative review including training programmes for family caregivers of people with dementia has proved it necessary to systematise programmes according to the stage of dementia, so as to facilitate the comparison of results, the verification of efficiency levels and the assessment of health gains induced by their application, given the fact that this is the only possibility to assess their quality.6 The review established also that training programmes for family caregivers of people with dementia living at home produce positive results for participants; notwithstanding, results need to be deepened and validated. The conceptual characteristics of these programmes require improved definition, as for instance via focus groups or Delphi studies, as well as by proving their effectiveness, e.g., by using controlled experimental studies with more significant samples.6
In Portugal a gap of training programmes for family caregivers of people with dementia living at home is felt, which substantiates the present study. The programme “Living together with Dementia” has been created with resource to an integrative revision of literature,6 a focus group7 and a Delphi study. It is a psychoeducational study featuring individual sessions, aiming at the training of the family caregiver of people with dementia living at home.
So as to validate the programme, a randomised controlled pilot study is taking place, whose protocol is presented in this study. The goals of the pilot study are as follows:
- •
To assess the effectiveness of the programme “Living together with dementia” when compared to the ordinary nursing care provided to these caregivers;
- •
To assess overload, satisfaction and difficulties of the family caregivers after participating in the programme.
The hypothesis that we endeavour to prove is that the family caregivers who integrate the experimental group and participate in the “Living together with dementia” programme will present lower overload levels, greater satisfaction levels and less difficulties associated with the caregiver role than the control group participants.
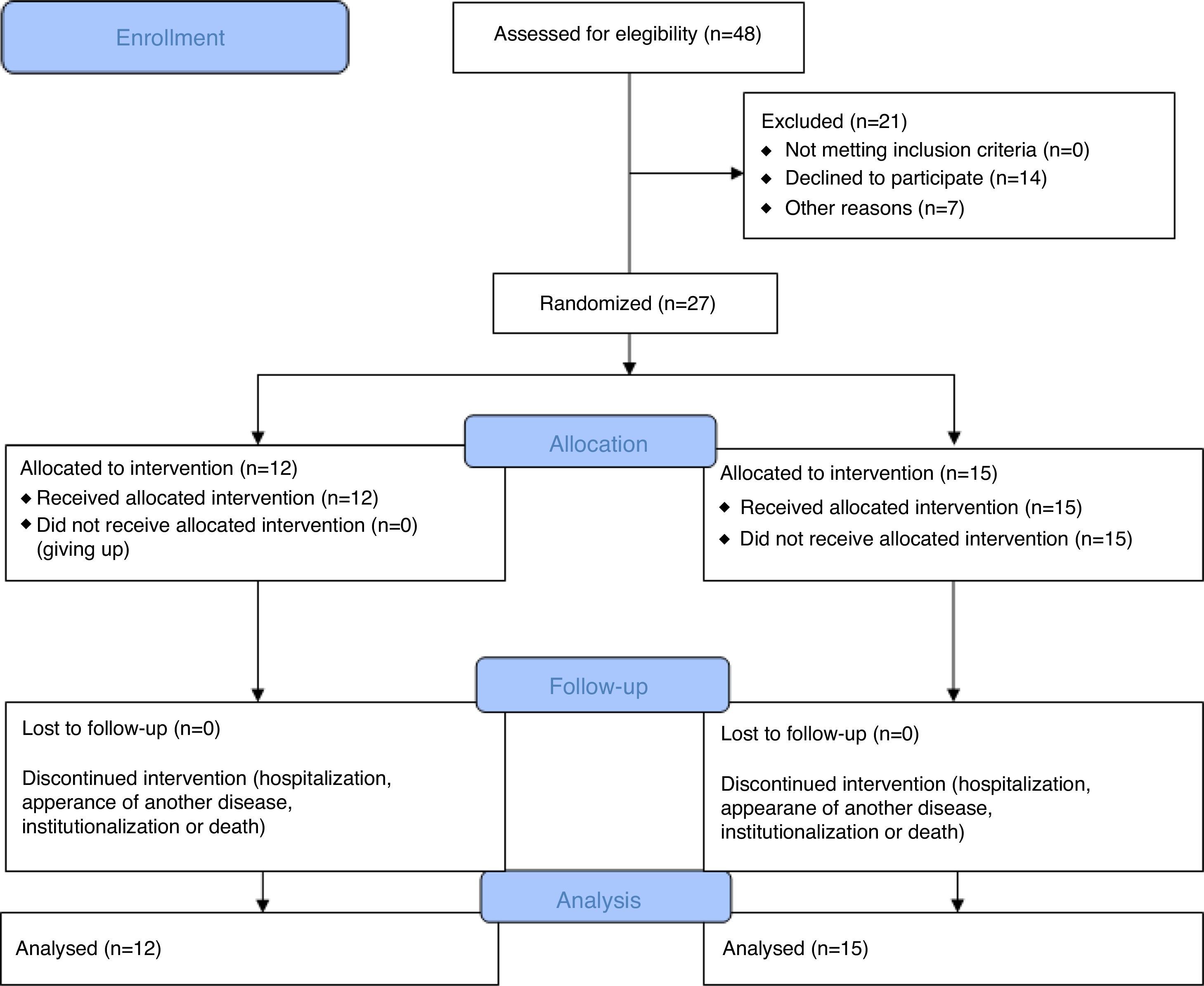
MethodsStudy designThe “Living together with dementia” programme has been designed as a randomised control trial with follow up (4 months, after the end of the intervention). All procedures are in accordance with consolidated standards of reporting trials (CONSORT)8 presented in Fig. 1.
SettingThe study will take place at the São João Hospital Centre, EPE, Porto-Portugal, at the neurology outpatient consultation, namely, the dementia consultation.
ParticipantsInclusion criteriaThe following inclusion criteria should be met to allow family caregivers to be eligible to participate in the “Living together with dementia” programme: (a) To be the main caregiver of the person with dementia in early or moderate stages; (b) to be literate; (c) to be motivated to participate in the programme; and (d) to reside in Porto.
Exclusion criteriaFamily caregivers were excluded if: (a) the target population of care does not have dementia in early or moderate stage; and (b) the person with dementia suffers from other severe mental pathology.
Recruitment/randomisationFor a 6-month period (from October 2015 to March 2016), the family caregivers were recruited subsequent to the neurology outpatient consultation, namely the dementia group of the São João Hospital Centre – EPE – Porto. The neurologists attending the dementia consultation (auxiliary researchers) have identified the caregivers who met the inclusion criteria and requested their permission to be afterwards reached per telephone, in order to provide information about the study and to accept or not to take part in it. The telephone contact that took place afterwards has been performed by one of the auxiliary researchers. The family caregivers who accepted to participate in the study have been classified in a random numeric listing, and had a participation code assigned (from FC1 to FC27). The allocation has been performed by the drawing of lots of numbered slips of paper performed by the research supervisors. The first 12 caregivers whose numbers have been drawn integrated the experimental group. Helsinki Declaration9 ethical principles have been considered throughout the entire process.
Ethical considerationsThe study and its protocol were accepted by the Health Ethical Commission of the São João Hospital Centre in September 2015. The study is registered in www.clinicaltrials.org with ID number NCT 03015428. All family caregivers who will participate in the study signed a free, prior and informed consent required for a health institution.
InterventionsConventional careThe family caregivers who integrate the control group will have access to standard health care in the health institution where the study is taking place, such as a neurology appointment every 6 months and the possibility of solving any queries about the pathology, care provision and therapeutic regime with the healthcare professionals’ team (doctor, nurse, social worker, psychologist). The participants of the control group will be assessed in the beginning of the study (T1), 7 weeks after (T2) and in a 4-month follow up (T3).
“Living together with dementia” programmeThe family caregivers who integrate the experimental group will be submitted to the “Living Together with Dementia” programme, an individual psychoeducational programme, developed and applied by mental health and psychiatry specialist nurses which aims at training the family caregiver who undertakes the care of people with dementia living at home. This is a 7-week programme, composed by 7 individual sessions with a one weekly session load and an average duration of 60min each and 2 group sessions with all the caregivers present with an average duration of 90min. The individual sessions encompass the following topics: dementia, its stages and symptoms; communication and behaviour management; pharmacologic intervention; emotions, expectations and demands of being a caregiver; assistance strategies for the basic and instrumental daily life activities; cognitive stimulation and environment management; coping strategies and problem solving techniques; the caregiver physical and mental health management; existing resources in the community. In the group sessions challenges, emotions, expectations and strategies of being a caregiver of a person with dementia will be shared. Throughout the programme, the methodologies that will be utilised are topic presentation, discussion, practical examples/demonstrations, skill training, practical exercises and movie display. The researcher (nurse) who will apply the programme will always be the same so as to reduce distortion. The participants of the experimental group will be assessed in the beginning of the study (T1), in the end of the programme – 7 weeks after (T2) and in a 4-month follow up (T3).
Data collection and outcomesOutcomesAll the family caregivers who integrate the study will be assessed in the three moments by means of:
- a.
Characterisation of the family caregiver (age, gender, schooling, professional occupation, marital status and kinship with the person with dementia). This evaluation also includes questions that seek to characterise the care for the person with dementia, in this fashion: For how long are you a family caregiver?; How many hours a day do you dedicate to the care of the person with dementia?; Do you rely on any help in the care for the person with dementia?; On whose help do you rely on?; What was the previous relation with the person with dementia?; Do you have any training as caregiver?);
- b.
Three open questions about the strategies that are a daily resource (In your daily routine as a caregiver how do you handle unexpected happenings/problems?; In your daily routine as a caregiver how do you deal with stress symptoms?; In your daily routine as a caregiver how do you regard less good happenings?);
- c.
Scale of Caregiver Burden (SCB) (validated for the Portuguese population10);
- d.
Caregiver Assessment of Difficulties Index (CADI) (validated for the Portuguese population)10,11;
- e.
Caregiver Assessment of Satisfaction Index (CASI) (validated for the Portuguese population),10,11 and;
- f.
Pinpoint the 5 major daily needs from a supplied list (the 16-needs list was collected by means of an integrative review of the literature and includes items concerning: management of emotions, feelings, expectations and demands associated with the caregiving process; the development of effective coping techniques, conflict resolution and decision-making techniques; the development of strategies for mental and physical health maintainance; the acquisition of knowledge about dementia, its stages, psychologic and behavioural alterations, communication and behaviour management, adaptation strategies for the basic and instrumental daily life activities and general cognitive stimulation; environmental adjustment; family, social and work relations management and the knowledge of and access to the community resources).
In the first assessment moment (T1), people with dementia are assessed as well so that identification of the exact stage of the condition is pinpointed and their main handicaps, so that individual intervention with the caregivers might be adjusted to the real needs. To perform such assessment, the following will be applied:
- a.
Characterisation of the person with dementia (age, gender, schooling, professional occupation, marital status for how long has dementia been diagnosed and type of dementia);
- b.
Mini mental state examination (MMSE) (validated for the Portuguese population)12;
- c.
Dementia Clinical Scale (DCS) (validated for the Portuguese population).13
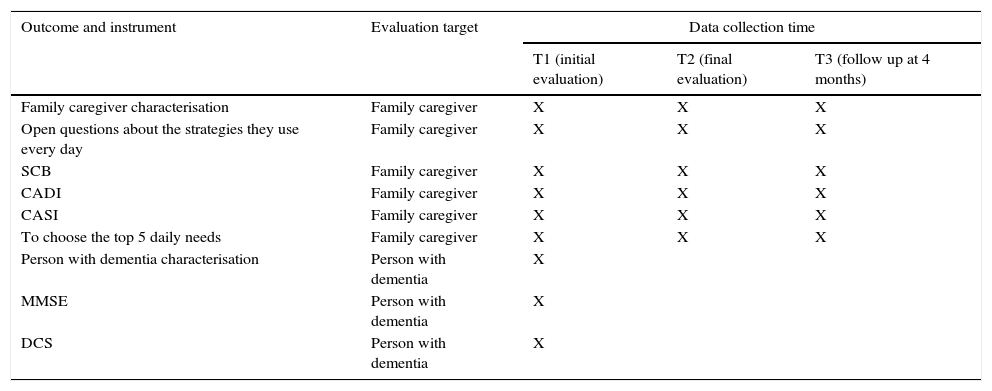
In Table 1 the outcomes measures are to be observed as well as data collection of family caregivers of people with dementia and people with dementia.
Outcomes measures and data collection of family caregivers of people with dementia and people with dementia.
| Outcome and instrument | Evaluation target | Data collection time | ||
|---|---|---|---|---|
| T1 (initial evaluation) | T2 (final evaluation) | T3 (follow up at 4 months) | ||
| Family caregiver characterisation | Family caregiver | X | X | X |
| Open questions about the strategies they use every day | Family caregiver | X | X | X |
| SCB | Family caregiver | X | X | X |
| CADI | Family caregiver | X | X | X |
| CASI | Family caregiver | X | X | X |
| To choose the top 5 daily needs | Family caregiver | X | X | X |
| Person with dementia characterisation | Person with dementia | X | ||
| MMSE | Person with dementia | X | ||
| DCS | Person with dementia | X | ||
The validated SCB for the Portuguese population by Sequeira10 is composed by 22 items that evaluate the objective and subjective overload of the family caregiver. Each item is scored by the caregiver from 1 (never) to 5 (always), with a global score varying between 22 and 110, in which a score less than 46 indicates absence of overload, between 46 and 56 mild overload and over 56 intense overload.
The validated CADI for the Portuguese population by Sequeira10 is composed by 30 potential difficulties related with the caregiver. Each item is scored by the caregiver from 1 (does not take place in my case) to 4 (it happens and disturbs me very much). Higher scores mean greater difficulties.
The validated CASI for the Portuguese population by Sequeira10 is composed by 30 items containing positive items associated to the provision of care. Each item is scored by the caregiver from 1 (provides no satisfaction) to 4 (provides much satisfaction). Higher scores mean higher satisfaction levels.
The validated MMSE for the Portuguese population by Guerreiro, Silva, Botelho, Leitão and Garcia12 is a short test for general cognition assessment. Is composed by 30 questions that assess orientation, attention and calculation, retention, evocation, language and constructive skill. It has a total score of 30 points and schooling is also taken into account for evaluation, with the following cut off points being considered cognitive handicap: Schooling 0 to 2 years – 22 points; Schooling from 3 to 6 years – 24 points and Schooling +7 years – 27 points.
The validated DCS for the Portuguese population by Garrett et al.13 consists of a global evaluation, that calculates the influence of cognitive handicaps in the daily life activities, without presenting cut off values, since the individuals are compared with their own initial performance. This instrument assesses memory, time and space orientation, judgement, problem resolution, social interaction, hobbies and personal care. A score is assigned according to the degree of involvement as follows: 0=Healthy; 0.5=Open to question; 1=light; 2=mild; 3=serious. Only the category “personal care” does not present the score “Open to Question”.
Data analysisFor data analysis, SPSS software 21 (SPSS® Inc., Chicago, IL, USA) application will be applied. For the purpose of family caregivers’ characterisation as well as that of people with dementia, the response to the 5 greater daily needs, MMSE and DCS scores, descriptive statistics will be employed. For result comparison of SCB, CADI and CASI non-parametric statistical analysis will be applied in the three evaluation moments, namely the ANOVA test for repeated tests, due to the reduced size of the sample. For the analysis of differences in the open questions on the strategies used on a daily basis by the caregivers, content analysis will be employed, according to Bardin.14
DiscussionIn view of the prevalence of dementia in the world, and thereafter in Portugal, the development of the present study is paramount. By dint of the increase of the number of people with this syndrome, many families commence living together and feel the need to cope with a set of cognitive and behavioural changes for which they are not qualified. This triggers overload and emotional burnout for the family caregiver.
In Portugal, there are no validated and systematically implemented training programmes for family caregivers of people with dementia living at home. The programme “Living Together with Dementia” seeks thus to fill this gap and become an asset to guide the professionals’ intervention.
We strongly believe that validation and implementation of this programme will prove an asset for the caregivers of the person with dementia themselves, inasmuch as the participants of the experimental group are expected to develop knowledge and skills to provide better care to the person with dementia which brings forward a reduction of the overload and difficulties level as well as greater satisfaction.
The psychoeducational programmes tend to be more efficacious in the caregivers’ training.4,5 The programme “Living together with dementia” features therefore a psycho-educative trait and an individual approach, so that, notwithstanding a core of topics to be covered, it might be adapted to the specific needs of each caregiver.
The major constraints expected throughout the development of the study, are linked to the potential difficulty of commuting of the family caregivers to the hospital due to the lack of means of transport, timetable difficulties and not having any support when it comes to taking care of the person with dementia. To soften these constraints, the programme sessions will be adapted to the caregiver's timetable, which includes weekends and after-work periods if needed.
The results of the pilot-study are expected to allow a future institutional implementation of the programme and the performance of a more robust study of its efficacy. A goal to attain would be the implementation of “Living together with Dementia” in the primary healthcare throughout the country.
LimitationsThe reduced dimension of the sample is the main limitation that has been predicted for the study, since in the present conditions non-parametric statistics will be utilised, which does not allow generalisations. However, since this is a pilot-study, assessing the importance of the programme is feasible, as well as performing adjustments, and in a future, develop a study of greater dimensions.
ConclusionThe construction, validation and implementation of training programmes for family caregivers of people with dementia presents itself as a priority in health in the national context. The programme “Living together with Dementia” arises as a response to this need, as well as a guideline for the professionals’ intervention. The pilot-study illustrated in this protocol has the purpose of verifying the importance of the programme and identifying viable improvements that facilitate its implementation.
Author contributionsEvaluation, intervention with the participants and drafting of the protocol: Lia Sousa. Review/Correction of study design and drafting of the protocol: Carlos Sequeira; Carme Ferré-Grau. Review of protocol: Pedro Neves; Mar Lleixà-Frotuño. Recruitment of participants: Ana Monteiro; Joana Meireles; Madalena Pinto; Tiago Gomes.
FundingNone declared.
Conflict of interestThe authors declare no conflicts of interest.