Family practice is the specialty with the highest number of doctors and covers all of Portugal. Therefore, the attitude of these doctors may have a high impact on patients.
ObjectiveTo explore the opinion and difficulties of Portuguese family doctors on dealing with communication with patients with life threatening diseases.
MethodsA questionnaire was sent to about 10% of family doctors of Northern Portugal. The questionnaire included questions about the disclosure of information, if they feel they need training courses and what they would want if they had a life-threatening disease.
ResultsA questionnaire was given to 196 doctors and 159 (81%) participated in this study. The median age was 43 years (26–64) and 108 (68%) were females. One hundred thirty-five (85%) consider that breaking bad news is a difficult task. One hundred twenty-four (78%) feel they need training in breaking bad news. For many doctors, the disclosure of diagnoses and prognoses has a detrimental psychological effect and affects patients’ hope, but gives patients’ control of the situation. Given a situation where the doctors themselves had a life-threatening disease, the vast majority would want to know the diagnosis and the prognosis and to participate in treatment decisions.
ConclusionsBreaking bad news is still a difficult task. Their attitude to this duty is different from what they would wish if they themselves had a life-threatening disease. One important conclusion is the need of specific training in communication for family physicians that should begin in the training phase of their specialty.
The disclosure of information about the diagnosis and prognosis of life-threatening diseases is still a controversial matter. It is well known that in some countries, such as Anglo-Saxon countries,1 Canada,2 the United States,3,4 and Northern European countries5 the most usual attitude is to convey the information that patients want to hear. In contrast, in other countries such as those in Southern Europe,6–8 Eastern Europe,9 the Middle East,10 South America2 and Asia11 patients are traditionally “protected” from the distress that would result if the information were disclosed. Those differences are usually attributed to cultural issues, but the most usual practice in a country is not static, it may evolve with time. For example, in 1961 in the United States 90% of physicians indicated a preference for not telling a cancer patient the diagnosis, but at the end of the 1970s, 97% of the physicians preferred to disclose the diagnosis.12
In the year 2000 we carried out a study on the views of doctors on the disclosure of cancer diagnoses in the Porto Center of the Portuguese Institute of Oncology.13 We have also conducted a survey, in 2002 and 2003, on the experiences and preferences of cancer patients about information disclosure.14 This survey was carried out in the first contact with patients under palliative care at that hospital. However, no studies have been carried out in Portugal on the attitudes and practices of doctors in other specialties, as far as we know.
The Portuguese health care system is based on a public National Health System, which includes the network of health centers with the family physicians and hospitals all over the country. There is also private medicine with private hospitals and other facilities whose services are paid directly by patients or through insurance companies. Civil servants have also a kind of public insurance that reimburses them partially if they choose to be treated in the private medicine facilities. There are others smaller subsystems for particular professions.
Family practitioners come into contact with patients with a wide range of different diseases, some of them life-threatening, such as cancer, neurological diseases and organ failure. Family practice is the specialty with the highest number of doctors and covers all of Portugal. Family physicians are often the first contact patients have with the National Health Services, playing a gatekeeper role and providing health care continuously throughout their lives. Therefore, the attitude of these doctors can have a high impact on patients. That is why we decided to explore this issue, carrying out a survey on those physicians. This may add useful information on family doctors’ practice concerning this important aspect of care.
MethodsThe population of the northern region of Portugal is about 3000000, and there are about 1800 family physicians. A questionnaire was specifically developed for this survey, based on the questionnaire used in the study carried out with the oncologists, mentioned before. It was assessed by ten physicians and modified according to the relevant suggestions. Then the questionnaire was circulated by all the researchers involved in this survey and once again some details were modified. The validation of the questionnaire was only facial, that is, all researchers agreed that the questionnaire seems to be adequate to assess what it is supposed to assess, without any further validity, such as construct or criterion validity.
Most family medicine trainees in Northern Portugal do a one-month internship in our palliative care department. Doctors that were in the internship during 2012 were invited to participate in the study, one per family practice center, and were the researchers responsible for conducting the study in their center. Therefore, all centers were located in Northern Portugal. When the different parts of that region were reasonably covered the inclusion of researchers was terminated.
The questionnaire included a total of 66 questions and it took about 15min to be completed. The part of the questionnaire used for this study, whose focus was mainly personal opinions and difficulties of doctors on breaking bad news, included questions about demographic data, on informing patients and their families of diagnoses and prognoses for life-threatening diseases, such as cancer, and involvement in treatment decisions. The personal questions were about how doctors see the disclosure of relevant information to patients and their families: how difficult it is, how ready they feel for it, how ready their colleagues are, if the time available is a problem, if they feel they need to attend training courses, if they have actually participated in these courses and, if so, how many and how many hours, if their communication practice changed as time went by and to what extent the training influenced their practice; the last 3 questions were about the hypothetical situation of the doctors themselves having a life-threatening disease and if he/she would like to be informed of the diagnosis and the prognosis and to participate in treatment decisions. This article focuses mainly on these personal questions. Most questions were answered using a verbal rating scale (always, often, sometimes, rarely, never; ex. “do you feel prepared to break bad news to your patients?”), except answers about the number of training courses and the number of hours spent on attending them and the 3 last questions. In those 3 question the verbal rating scale was different (yes, no, no opinion; ex. “if you had a life-threatening disease, such as cancer, would you wish to be informed on the prognosis?”).
The study was carried out in January 2013. The questionnaire was sent to 20 family health centers all over Northern Portugal. The questionnaire was delivered to 196 doctors, who were all family doctors allowed to deal with patients autonomously and willing to participate. All doctors who participated in the study signed a written informed consent.
The protocol was approved by the Ethics Committee of the Northern Portuguese Health Authority and authorized by the medical directors at each center.
Statistical analysisThe variables were analyzed by proportions and means. To evaluate the existence or not of associations between categorical variables, the chi-square test was used. The IBM SPSS Statics version 24.0 statistical software was used to analyze the data. Missing data were omitted, an approach usually called listwise deletion or complete case analysis.
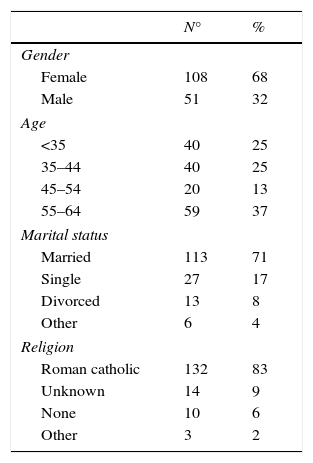
ResultsFrom the 196 doctors contacted, 159 (81%) participated in this study, with a range of participation in each center between 56% and 100%. The median age was 43 years (26–64) and 108 (68%) of them were female. One hundred thirteen (71%) were married and 132 (83%) were Roman Catholic (Table 1). Their time of practice was: ≤10 year – 53 (33%) doctors; 10–25 – 34 (21%); >25 – 71 (45%). One hundred (63%) doctors followed less than 10 patients with life threatening diseases, such as cancer, per year, and only 10 (6%) followed 30 or more.
Demographic data.
| N° | % | |
|---|---|---|
| Gender | ||
| Female | 108 | 68 |
| Male | 51 | 32 |
| Age | ||
| <35 | 40 | 25 |
| 35–44 | 40 | 25 |
| 45–54 | 20 | 13 |
| 55–64 | 59 | 37 |
| Marital status | ||
| Married | 113 | 71 |
| Single | 27 | 17 |
| Divorced | 13 | 8 |
| Other | 6 | 4 |
| Religion | ||
| Roman catholic | 132 | 83 |
| Unknown | 14 | 9 |
| None | 10 | 6 |
| Other | 3 | 2 |
Demographic data of the family physicians participating in this study.
Comparing the doctors included in this study with the total of family doctors in Portugal we verified that the proportion of females was higher in this study and marginally significant (p=0.049). Regarding that proportion inside the age groups we found a significant difference between women and men relatively to the total only in the 35–44 years age group (p=0.01); in the group<35, p=0.09, in the 45–54, p=0.43, and in the 55–64, p=0.54.
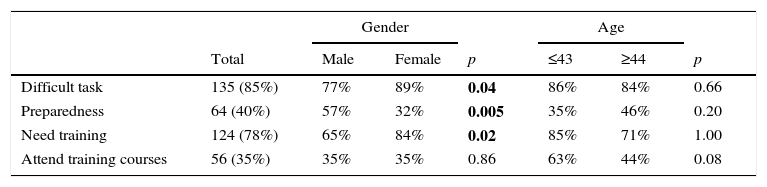
Physicians’ personal issuesOne hundred thirty-five (85%) doctors considered that breaking bad news was a difficult task. Only 64 (40%) doctors felt they were prepared for it, with a significant difference between genders (Table 4). Doctors considered their colleagues even less prepared than themselves, as only 38 (24%) believed that their colleagues were prepared to carry out that duty. Only 31 (20%) doctors answered that lack of time is a barrier to breaking bad news.
One hundred twenty-four (78%) physicians feel they need training in breaking bad news. Dividing the doctors age by the median, there was a significant difference between the younger and the older doctors concerning the need for training: 68 out of 80 (85%) of the younger ones vs. 56 out of 79 (71%). However, only 56 (35%) actually attended training courses, without specifying the course type (Table 4). The number of these courses varied from 1 to 3; most of them (67%) attended 1 course. The number of hours spent attending these training courses varied from 1 to 60 with a median of 6h. Of the doctors who attended these courses, 42 (75%) doctors think that the training courses had a positive influence on how they break bad news.
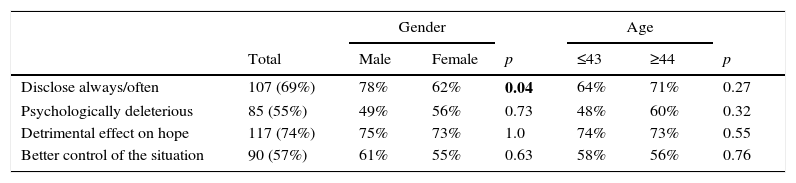
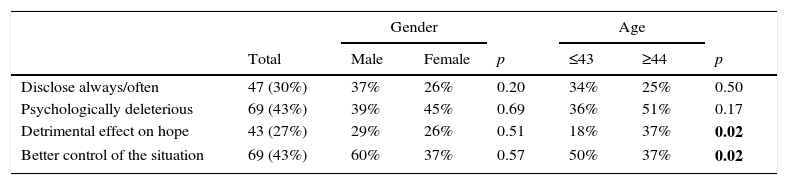
Most physicians disclosed the diagnosis of a life-threatening disease always to often with a significant difference between genders (Table 2). But with regard to prognosis, the situation is different (Table 3). For some doctors the disclosure of the diagnosis and of the prognosis are psychologically deleterious and has a detrimental effect on patients’ hope. On the other hand, many think that the disclosure gives patients control of the situation. Those opinions differ between older and younger doctors (Table 3).
Family physician's practice and views on diagnosis disclosure.
| Gender | Age | ||||||
|---|---|---|---|---|---|---|---|
| Total | Male | Female | p | ≤43 | ≥44 | p | |
| Disclose always/often | 107 (69%) | 78% | 62% | 0.04 | 64% | 71% | 0.27 |
| Psychologically deleterious | 85 (55%) | 49% | 56% | 0.73 | 48% | 60% | 0.32 |
| Detrimental effect on hope | 117 (74%) | 75% | 73% | 1.0 | 74% | 73% | 0.55 |
| Better control of the situation | 90 (57%) | 61% | 55% | 0.63 | 58% | 56% | 0.76 |
Significant associations in bold.
Family physician's practice and views on prognosis disclosure.
| Gender | Age | ||||||
|---|---|---|---|---|---|---|---|
| Total | Male | Female | p | ≤43 | ≥44 | p | |
| Disclose always/often | 47 (30%) | 37% | 26% | 0.20 | 34% | 25% | 0.50 |
| Psychologically deleterious | 69 (43%) | 39% | 45% | 0.69 | 36% | 51% | 0.17 |
| Detrimental effect on hope | 43 (27%) | 29% | 26% | 0.51 | 18% | 37% | 0.02 |
| Better control of the situation | 69 (43%) | 60% | 37% | 0.57 | 50% | 37% | 0.02 |
Significant associations in bold.
Family physician's difficulties on breaking bad news.
| Gender | Age | ||||||
|---|---|---|---|---|---|---|---|
| Total | Male | Female | p | ≤43 | ≥44 | p | |
| Difficult task | 135 (85%) | 77% | 89% | 0.04 | 86% | 84% | 0.66 |
| Preparedness | 64 (40%) | 57% | 32% | 0.005 | 35% | 46% | 0.20 |
| Need training | 124 (78%) | 65% | 84% | 0.02 | 85% | 71% | 1.00 |
| Attend training courses | 56 (35%) | 35% | 35% | 0.86 | 63% | 44% | 0.08 |
Significant associations in bold.
When questioned about what they would want if they had a life-threatening disease, such as cancer: 144 (93%) said they would want to know the diagnosis, 10 (6%) had no opinion and only 1 said she would not want to know; as to prognosis, 129 (83%) would want to know, 11 (7%) would not and 15 (10%) had no opinion; 138 (87%) would want to participate in treatment decisions, 4 (3%) would not and 12 (8%) had no opinion.
DiscussionThe sample of doctors included in this study did not differ much in gender and age from the whole population of Portuguese family physicians. Therefore, the sample can represent that population and the conclusions of this study show which are the opinions and difficulties of Portuguese family doctors on breaking bad news.
Almost all family physicians in this study deemed breaking bad news to be a difficult task. In fact, there is a general consensus on that difficulty and, in the literature, statements like “breaking bad news is one of a physician's most difficult duties”15 are not rare. One study shows that a number of oncologists want to give up oncology practice because of the burden of communicating the discontinuation of treatment to their patients.16
Many doctors feel they are not prepared to break bad news and feel they need training, women more often than men, and the reason for that difference is not clear as female doctors are in general deemed better communicators with patients than male doctors. The same comment applies to the fact that male doctors disclosed diagnosis significantly more often than female doctors. Studies show that female doctors usually engage in more partnership building, emotional support, positive talk, and psychosocial discussion than male physicians.17–19
However, only a minority tried to solve this problem by attending training courses. Most of these courses were effective, but not all of them, according to the doctors’ opinions. The feeling of unpreparedness seems to be a general problem, even in countries where the usual practice is deemed to be disclosure.4
This study deals with family physicians’ approach to breaking bad news. In a study previously carried out by us, we found, unsurprisingly, that the disclosure of information to cancer patients was made more frequently by hospital doctors, but patients would prefer it to be made by family doctors.14 In another study, most patients stated that family physicians communicate, in general, more empathically than hospital oncologists and that family physicians give more opportunities to ask important questions. However, most prefer to discuss cancer therapies with the oncologist,20 concluding that the communication between hospital-based specialists and family physicians is important. Therefore, oncologists should involve family physicians in information disclosure.20
A negative impact that the disclosure of bad news could have at psychological level and on hope was an opinion shared by most family physicians. Older doctors shared the opinion on hope significantly more often than the younger ones, but as only 27% of the whole group thinks that the disclosure affects hope, the impact of this finding is uncertain. Other studies show doctors’ reluctance to convey bad news, mainly prognoses, even in countries where the communication of bad news is the norm.1,4,21 However, several studies suggest that patients can discuss prognoses without necessarily increasing anxiety, and that avoiding the discussion may have adverse outcomes.1 For example, knowing the prognosis is very important for helping patients with decisions about treatment. One study showed that patients who believe that their survival will be at least 6 months tend to prefer life-extending therapy while patients believing they have a shorter time to live tend to prefer comfort care.22 It should be noted, however, that one Turkish study found that knowledge of the diagnosis may be associated with higher psychiatric morbidity23; cultural influences are probably implicated in those results.
In the present study, only a minority of the physicians think that lack of time is a reason for non-disclosure, but this was indicated as a barrier to disclosure in other studies.1,16
The vast majority of family physicians would want to be informed of the diagnosis and prognosis if they had a life-threatening disease. They would also want to participate in treatment decisions. This means that there are doctors who would themselves want something they are not prepared to give to their patients. Other studies show similar results.2,4,9
This survey has some limitations. One of them is the fact that the family health centers were not selected in a systematic way. However, the 20 heath centers were located all over the Northern Portugal and age and gender of doctors were similar to those of the whole population of Portuguese family practitioners, probably representing what really happens. Another weakness of this survey is to be limited to the Northern Portugal. However, Portugal is a small country, nowadays without significant cultural differences among the different regions, so results similar to these probably would be found in any other region of this country. The number of doctors is reasonable for forming an idea of the practice and difficulties of family physicians concerning communication of bad news, however, the relatively small number of doctors at each center does not permit analyze the possible differences among those centers.
ConclusionBreaking bad news is still a difficult task for family physicians. Their attitude to this duty is different from what they would wish if they themselves had an advanced life-threatening disease. Many recognize they need training, but only a minority has attended training courses. Therefore, one important conclusion is the need of more specific training in communication which should begin at the undergraduate level, because this aspect is crucial for all clinicians, and also obligatorily in the training of all clinical specialties.
FundingThis work was supported in part by the Northern Branch of the Portuguese League Against Cancer.
Conflicts of interestThe authors declare no conflicts of interest.