The importance of clinical communication skills (CCS) teaching and assessment is increasingly recognized in medical education. There is a lack of outcome-based research about CCS teaching and assessment processes in Portuguese medical education. Our goal is to conduct a SWOT analysis of this process in Portugal, Angola and Mozambique in order to contribute to the establishment of an action plan for more effective CCS teaching and assessment in medical curricula.
MethodsBetween 2010 and 2012, semi-structured interviews focused on the state of the art of teaching and assessment of clinical communication skills were conducted with key stakeholders of medical courses in Portugal, Angola and Mozambique. The design corresponds to an exploratory, descriptive and cross-sectional study, with the analysis of the recorded interviews. Interview transcripts were analyzed to identify salient themes/coding template in their discussions of the CCS teaching process. The coding and analysis of the surveys is qualitative.
Results87 interviews were performed at the 8 Portuguese, 1 Angolan and 1 Mozambican medical schools. Results indicate that the teaching and assessment process of CCS is in the beginning stages with these commonalities noted: (i) Variability amongst faculty in the teaching and assessment methods, (ii) disconnection of CCS between basic and clinical cycles, (iii) content and process skills and (iv) faculty development.
ConclusionsCCS training lacks a formal structure with considerable variation of the CCS teaching process in these countries. The interviews promoted a rise in awareness of this situation and how these skills can enhance the quality of curricular change. Some important opportunities for the development and implementation of a framework of an integrated communication skills curriculum such as curricular reforms and well-established cooperation and networks were identified. The acknowledgement of the importance of integrating these skills in ME by key stake-holders and students in institutions and the identification of champions motivated to commit to the effort are strengths that should be considered to integrate and enhance CCS in the medical curricula.
Clinical communication skills (CCS) teaching and assessment is a core component of clinical competence. There is ample evidence that the effective teaching and training1–3 of these skills has a positive impact on physician's communication skills.2,4,5 There is also some consensus on the essential elements of effective CCS courses6–8 and that there is correlation between communication, clinical reasoning, and medical problem solving.9 These studies have been widely acknowledged and motivated gradual integration of CCS training across medical education.10–12
Medical schools are accepting the many challenges involved in developing clinical communication programmes. There is wide variation currently in the methods to teach and assess these competencies.1,4,13 Commonly, CCS are delivered at a pre-clinical stage of medical education and training is much less structured during the clinical and postgraduate phases.7,14–16 Our prior research17 which corroborates previous findings of other studies,18,19 has shown that experiences in CCS training affect attitudes towards the doctor-patient relationship, and content analysis associations suggesting that these perceptions are influenced by context, i.e. faculty and curricula.
In Portugal and in Portuguese speaking African countries there is a lack of research as well as lack of benchmarks on teaching and assessment processes for communication skills in medical schools. This occurs in the background of globalization in medical education and the recognition of CCS as a core competence for education of physicians who share the same language.
This research was conducted with the purpose of examining the current educational practices of CCS teaching and assessment in Portuguese and Portuguese speaking African medical schools to identify needs, potentials for curriculum development and faculty training with the intention of enhancing the necessary skills for a greater humanization of the medical practice as a caring profession.
MethodsThere are presently 8 Medical Schools in Portugal, 3 in the south, 2 in the centre and 3 in the north part of the country. Seven schools have 6 year curriculum and are organized in 2 cycles: (i) Degree in Basic Health Sciences and, (ii) Master Degree in Medicine. One school has a 4 year curriculum orientated for graduated students and is organized according to Problem Based Learning (PBL). The Faculty of Medicine of the University Agostinho Neto (FMAUN) in Luanda, Angola, has a traditional curricula, with 6 year duration and at the University Eduardo Mondlane (FMUEM).
We conducted interviews with the key stakeholders of the medical schools such as course directors, heads of the medical education, and faculty responsible for teaching of specific courses (syllabus). These courses included Medical Psychology, Clinical Semiotics/Propedeutic (course where the physical exam is taught and students have contact with patients in wards for the first time), Communication Workshops, Clinical Interview, Surgery, Medicine, Family/Community Medicine/Public Health, Psychiatry, Paediatrics and Gynaecology/Obstetric. Medical students were invited via e-mail to participate in an in-depth interview study. In Portugal and Mozambique, the interviews were conducted by EL and a research associate. In Angola interviews were conducted by EL.
Utilizing a qualitative approach semi-structures interviews lasting from 15 to 90min were audio-recorded face to face. Ethical approval for this study was obtained from the Ethics Committee of the Faculty of Medicine University of Porto/Hospital of São João, Porto.
The interview questions were developed considering the need to provide a comprehensive assessment of the teaching techniques of communication skills in Portuguese and Portuguese speaking African medical schools. These questions were inspired by a previous and pioneer study by Novak et al.20 Before data collection, interview questions were piloted with senior faculty and students of Faculty of Medicine of the University of Porto (FMUP). Interviews were preferred to surveys because we found that clinical communication skills were not perceived by all in the same manner and therefore interviews would enable a greater clarification and understanding of the process. As we intended to understand what the different medical courses foresee in terms of the teaching and assessment process of CCS as opposed to what is actually done in comparison to how students perceive their experience throughout their medical education, we felt the need to interview course directors, faculty and students. Questions for course directors and/or heads of the medical education approached what is being done, in general terms in that specific medical school, of CCS teaching and assessment (when, where, how it is taught and assessed, and type of remediation, if applicable). Interview questions for faculty responsible for teaching specific courses assessed the following: general knowledge and competencies of the courses, the related specific communication skills s, what teaching methods are used, how are they assessed, and the training of who teaches in CCS). Interview questions for students requested a description of their experience of the teaching and learning process of CCS in the course. The data was collected through open ended and semi-structured questions
All recorded interviews were transcribed verbatim and using a thematic analytic approach guided by phenomenology.21 EL, MAF and two fellow research associates with experience in qualitative analysis methods read through the interview transcripts to identify initial themes which were then compared and finally led to a coding template. All themes and codes were later reviewed by all authors to warrant that all transcripts clearly reflected those themes.
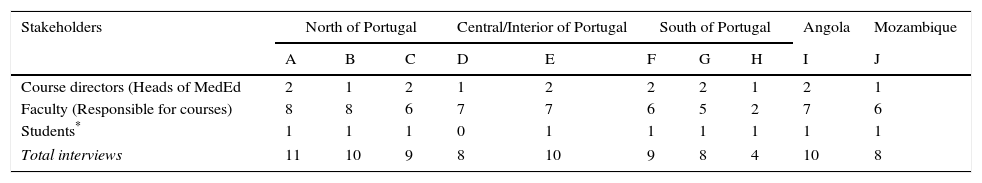
ResultsFrom January 2010 and June 2012, 69, 10 and 8 semi-structured interviews (n=87) were conducted at medical schools in Portugal (n=8), Angola (n=1) and Mozambique (n=1) (Table 1).
Summary of interviews at medical schools in Portugal, Angola and Mozambique.
| Stakeholders | North of Portugal | Central/Interior of Portugal | South of Portugal | Angola | Mozambique | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |
| Course directors (Heads of MedEd | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 1 |
| Faculty (Responsible for courses) | 8 | 8 | 6 | 7 | 7 | 6 | 5 | 2 | 7 | 6 |
| Students* | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total interviews | 11 | 10 | 9 | 8 | 10 | 9 | 8 | 4 | 10 | 8 |
Results have been divided according to the main areas (i) heads of Medical Schools and/or Medical Education departments, in order to find out their perceptions of what is being done in terms of CCS (ii) faculty for specific courses, in order to attain the general learning objectives and what teaching and assessment methods are used, and (iii) students to understand their experience of the teaching and learning process of the CCS throughout their medical training.
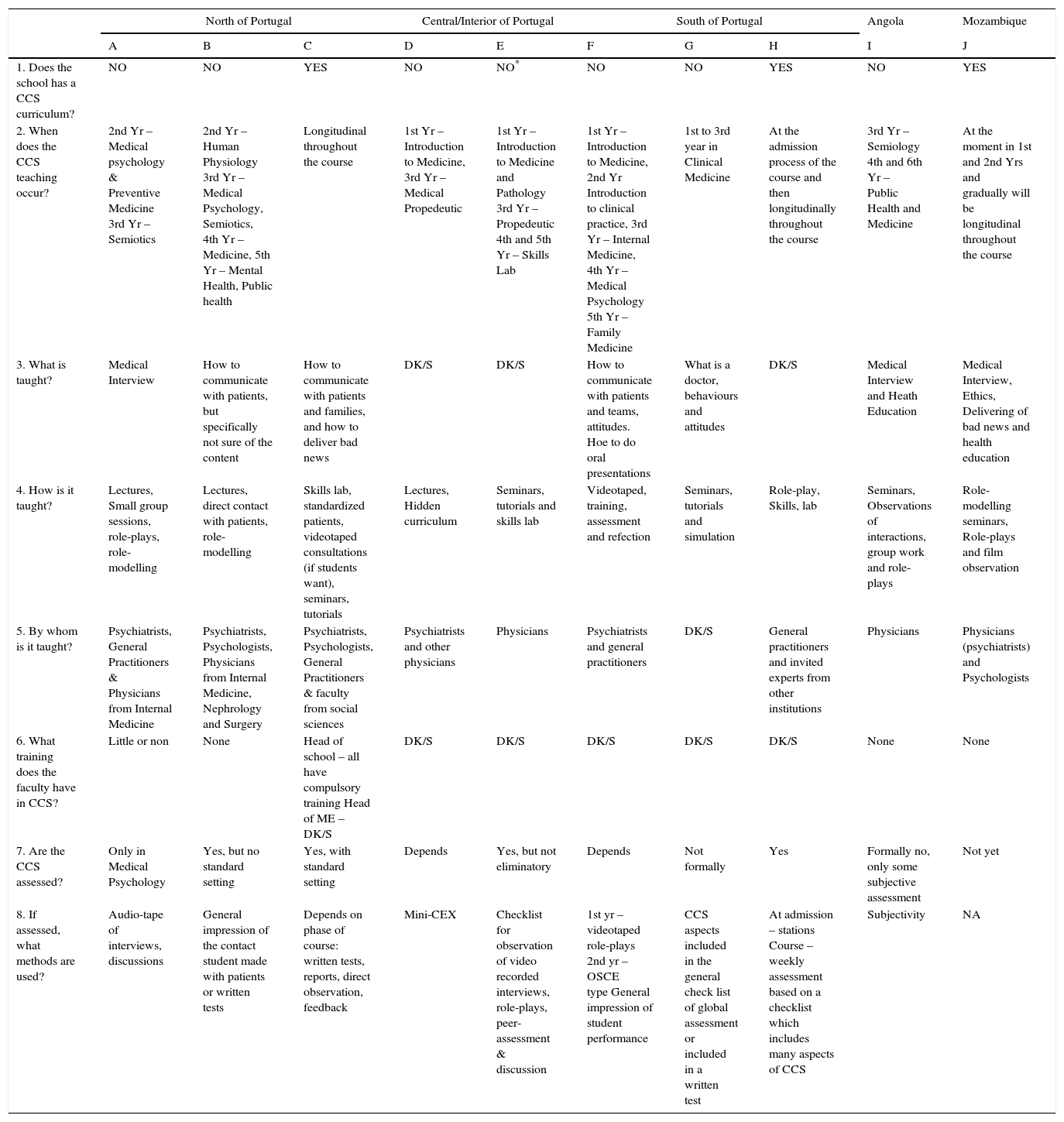
Heads of medical schools or medical education departmentsThe interviews with the heads of the Medical Schools or Medical Education Departments revealed that 6 of the Medical Schools in Portugal and the Angolan school at the time of the study did not have a formal CCS curriculum. Two medical schools in Portugal (one in the north [C] and one in the south [H] of the country – see Appendix A) and the Mozambican medical school have a longitudinal integration of CCS throughout the medical course. The interviews enabled a clear perception of (i) the general CCS content; (ii) the timing and teaching methods used; (iii) who teaches CCS and (iv) the assessment process:
ContentThe heads of these medical schools described Medical Interviewing and the basic behaviours students should learn to interact with patients and families are the main topics covered in the teaching of CCS. Those who confirmed to have a longitudinal integration were not clear on the framework/models of the teaching and learning process used. The heads of the schools in Angola and Mozambique also identified health education (in order to help individuals and populations improve their health, by increasing their knowledge or influencing their attitudes) as a main concern.
Timing and teaching methodsThe main teaching of CCS occurs in the basic cycle years of the courses, i.e. first 3 years of the course, when the contact with patients is very sparse. Lectures, seminars and role-plays are the most common teaching methods of CCS and three schools use their skills laboratories to enhance the teaching of these skills. Tutorials on the wards and role-modelling are common methods.
FacultyPsychiatrists, General Practitioners and Internal Medicine Physicians are the faculty most involved in the teaching of CCS. The specific training faculty have in this scope was not ascertained.
AssessmentIn terms of assessment, two schools [C & H] assess these skills and have checklists and clear standard settings, while the other schools state that that there is some assessment although not formal or objective and lack standardized measure. To illustrate this we may report to a statement from school E – “Assessment has a limitation due to the heterogeneity of the faculty”. The main assessment methods identified are observational checklists, audio/video taped interviews with discussion and some form of feedback, some written tests and overall impression of tutors for students performance.
Overall, according to these heads of medical schools/medical education, there is an increasing recognition of the importance of CCS and that these should be integrated into the courses.
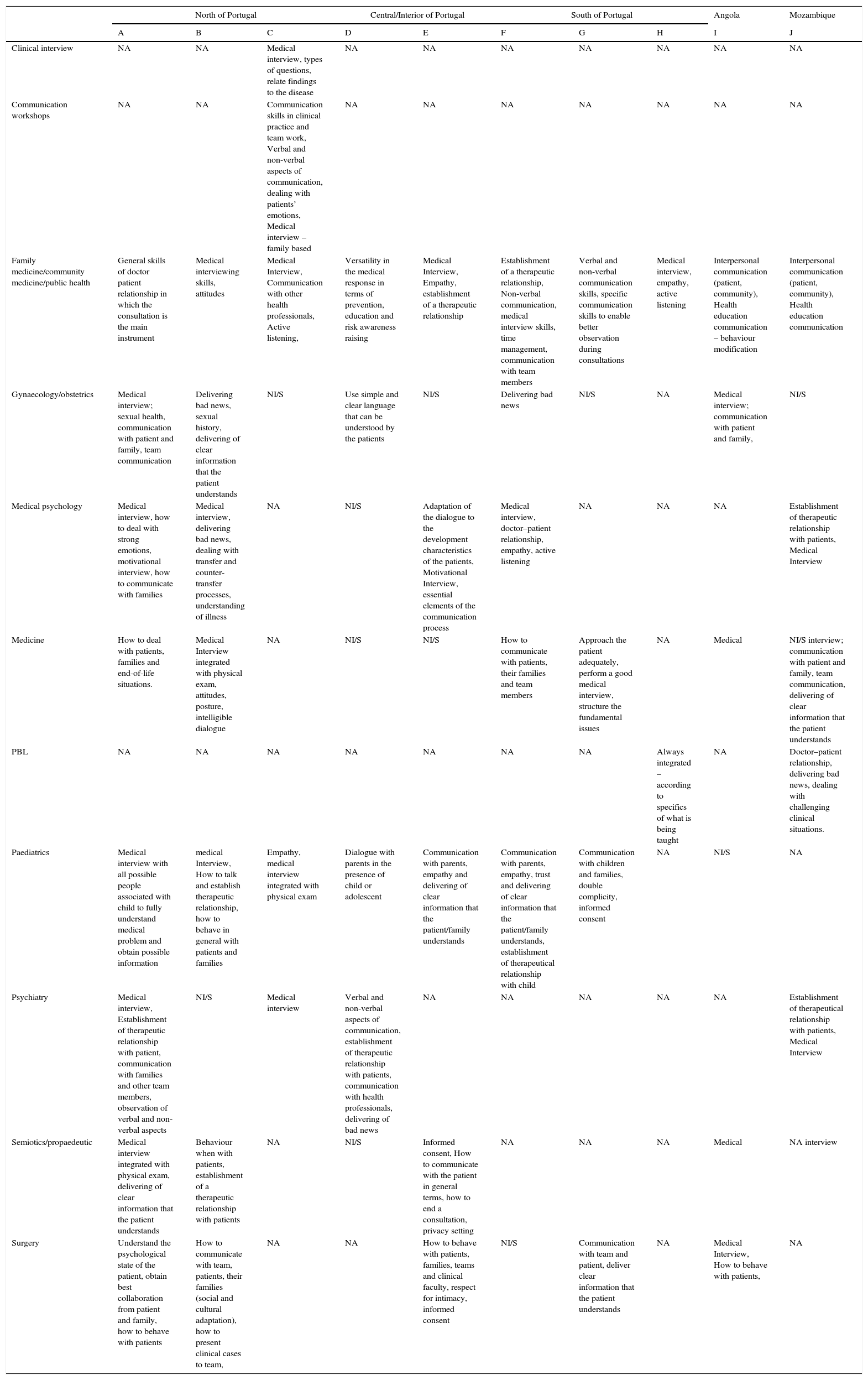
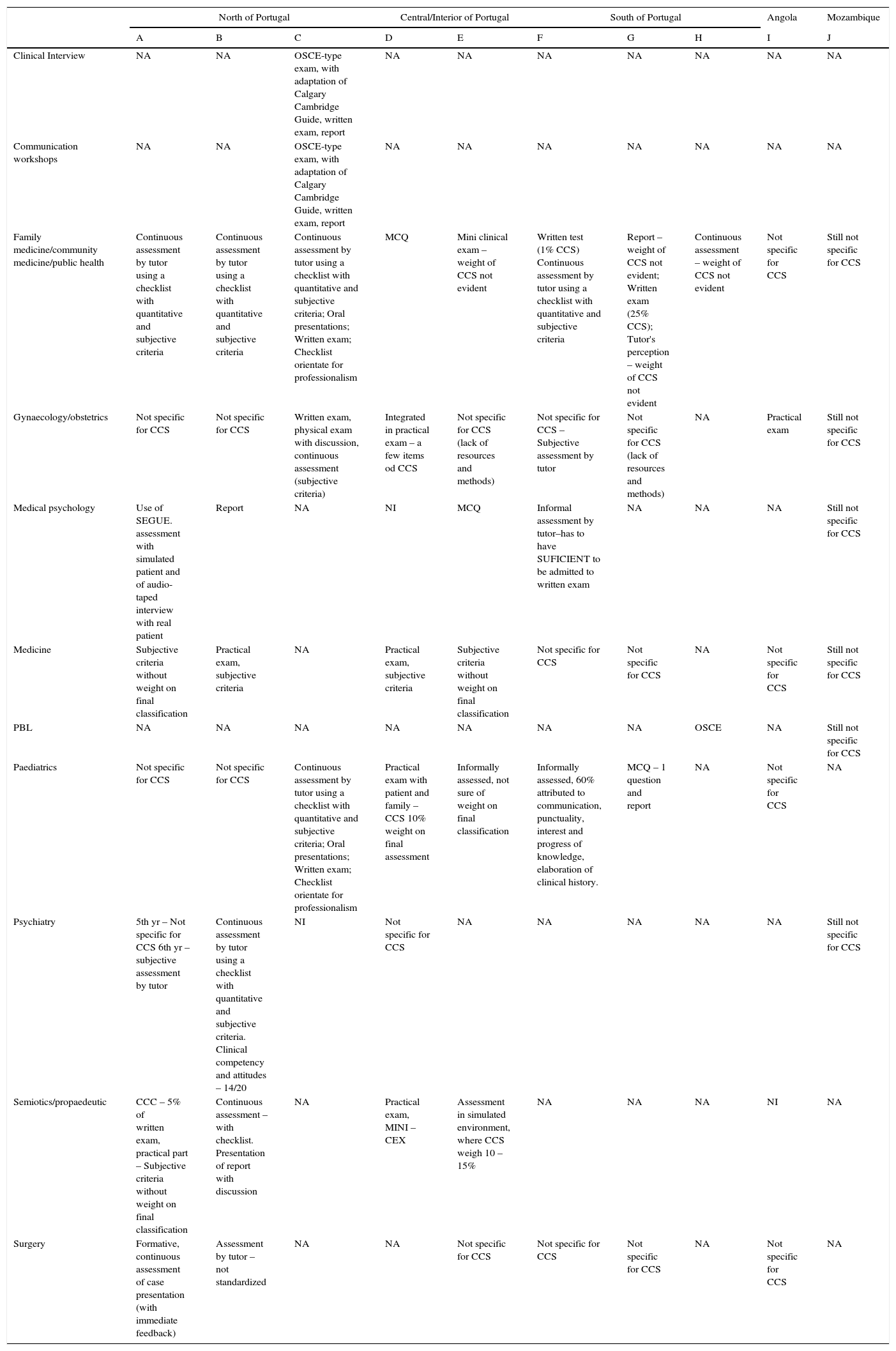
Faculty responsible for specific coursesThe results of the interviews to faculty responsible for teaching of specific courses (n=62) have been summarized in Appendix B.
Link between course objectives and CCSThe questions were related to CCS needed for the specific objectives of each courses. The major issues that have been identified are: (i) medical interview – adapted to the idiosyncrasies each course (ex. paediatrics, psychiatry, gynaecology); (ii) health care team communication; (iii) dealing with challenging situations (ex. delivering of bad news, sexual history, dealing with strong emotions); (iv) establishment of therapeutic relationships, empathy and active listening; (v) motivational interview/health education; (vi) cautions with medical jargon.
The faculty had gaps in CCS teaching and assessment. Some examples are. “I shall need training in this field so that I can answer this question”. “I have no training or expertise in this field”. “I assume that in the first five years of the course this issue was addressed and from then on, depends on the individual sensitivity of faculty and the learners”. “It is important, however, that students be able to transfer the technical objectives to the patients goals, as far as language is concerned, know how this is transmitted”. Others do not find it necessary to dedicate time to teaching these skills as: “it is assumed that CCS have been taught and learnt in the initial years of the course”.
Teaching and assessment methodsWhen questioned about the teaching methods used to convey the CCS in the specific courses in the clinical specialties of Surgery, Medicine, Family/Community Medicine/Public Health, Psychiatry, Paediatrics and Gynaecology/Obstetrics, the methods used are: (i) non-structured role-modelling through the observation students make of their tutors in practice; (ii) Supervised clinical practice with discussions, and (iii) seminars. Again, there are some faculty who do not identify the teaching methods: “I assume that the necessary CCS have been acquired in previous courses, or are innate, so teaching of CCS is purely casuistry and depends on the tutor”. With regards to courses associated with the basic cycle of the specialties of Medical Psychology, Clinical Semiotics/Propaedeutic, Communication Workshops and Clinical Interview, the most common teaching methods are: (i) role-plays, (ii) seminars; training of interviews in simulated settings with discussions; (iii) analysis of taped consultations; (iv) case-based learning. The medical schools with the PBL systems stated that the main teaching methods are seminars and tutorials and training in simulated environment (only school H).
In terms of the assessment methods of the CCS, the main results are summarized in Appendix C. There is no specific assessment process for the assessment of CCS. In some schools, written tests and generalized checklists are used which include aspects of communication. Students have a high pass rate and there are currently no formal remediation programs.
Another aspect highlighted was that the lack of teaching and assessment tools to integrate CCS. “…when we go to the doctor there is a 95% probability that he will ask us if we smoke and how much, but less than 10% about our sexual activity or sexuality. Why does this happen? Due to many reasons, but probably because it takes time but essentially because the doctor is not confident enough about this type of communication. Teaching tools are needed to help doctors gain more confidence and knowledge of how to approach these topics”.
Faculty developmentThe analysis of the interviews identified the need to have faculty specifically trained in CCS. For example, “….we notice many failures in the way doctors approach patients and communicate with them, therefore I consider there is a need for more intense training in this scope so as to reduce the deficiencies that the faculty themselves have” “…we need to be aware that students may be taught about CCS but then they might observe different things on the wards….they see many doctors and tutors who do not communicate well with patients… medical schools need to be careful or guarantee faculty development in these areas, for example”.
The analysis also identified the variability of teaching and assessment of CCS. “There is a problem that we need to resolve and that has to do with the great number of faculty we have for each course and therefore a great deal of variability in teaching and assessment, which can be deleterious in the basic training of students”.
Faculty further consider the number of students, which very high and limits the teaching and assessment of these skills: “If we had less students I would be able to assess the communications skills of our students….with 300 it is impossible”.
Students perspectiveThe interviews with medical students enabled a discussion about their experiences learning CCS during their medical education. Major themes common to these students from different medical schools arose, including: (i) Variability in teaching and role-models, (ii) Hiatus between basic and clinical cycles; (iii) Content vs process; (iv) Assessment and (v) Importance of training of CCS. Representative comments for each theme are included within each communality.
Variability in teaching and role-modelsStudents point out that there is a great variability of teaching methods within the same specialties, and depending on the tutor, some students get training in CCS and others not at all. Students many times do not feel reinforced by what they observe as opposed to what they are taught about in the scope of CCS. A - “….it depends on the tutor….in the 1st semester we had a tutor that would discuss with us how we communicated with the patient, this semester, the tutor doesn’t even observe us” B - “The CCS teaching is dependent on the tutor you get ….it is not an organized thing” E - “….and then everything is done by imitating tutors. At the hospital we become medicalized, we imitate what we see and, sometimes the examples are not good”
Students underline the fact that when CCS teaching occurs it is mostly focused during the basic cycle years when there is little or no contact with patients. They also consider the CCS teaching to be generally informal and empirical. They feel that many faculty members consider CCS to be innate and implicit. F - “….CCS are not taught in a structured manner, a couple of things seem empirical, faculty assume that everyone knows how to communicate and what posture to have (and we don’t)….” C - “Most faculty assume that these skills were taught and acquired in the first years of the course and then in the clinical cycle we just apply”
The students highlighted the fact that they are assessed in terms of what they ask vs process, and that a greater emphasize is given to pathology as opposed to communication skills. They report that they are not observed in many of their interactions with patients and therefore the feedback they may receive when reporting on clinical histories is only on content. They also underline the fact that there are many sensitive issues that should be approached with the patients and are not just because students do not feel comfortable and/or do not know how to do this. A - “…the tutor is rarely present when we take a history, therefore he privileges the content of the history and the way it was taken is not assessed, and I get no feedback on that” F - “….greater value is given to the fact that we do not know how to palpate or to auscultate rather than not knowing how to talk to a patient….in the end, what we miss most in terms of training is what worries us less” B - “…. I can retain from asking about sexual risk behaviors, and since no one is observing me I can write doesn’t have or denied. If someone questions if I asked I say yes. It is not only a matter of knowing what to do, its training to do and training to the point where you feel more comfortable too…”
Students admit to be driven by assessment, which in turn drives learning, therefore it is crucial that CCS be assessed with objective and structured procedures with standard settings. E - “CCS must be assessed with objective criteria and have a greater weight in the final exam”
Overall the students recognize the utmost importance of CCS in Medical Education and that specific CCS teaching and assessment methods should be developed and integrated throughout the specialties and other courses. They believe that including simulation and use of simulated patients in this training would be beneficial and increase the competence (knows how) and performance (shows how) levels proposed by Miller.22 The students from Angola and Mozambique highlight the need to have CCS developed throughout the course and especially for their need to promote behaviour change in patients and community in general in areas of major health concern in these countries.
H - “CCS are very important and are fundamental to help us have more adherence from the patients” B - “Due to the excessive amount of students and the risk of patient saturation standardized patients should be made available so that students all get the same training opportunities” I - “How do we help our population change behaviors and life-styles if we do not know how to reach out to them and get their trust and reliance–this can only be achieved if we have better CCS”
The overall impression is that only 3 schools currently have a formal CCS curriculum in their specialty courses. There is variability in the teaching and assessment process of CCS across medical schools in Portugal, Angola and Mozambique. Interviews with the heads of the medical schools or medical education departments suggest that at this time there is a lack of a structured framework on CCS.
Our study shows a disconnection between the content of the programmes and the difficulty in separating skills from themes and the importance of defining core communication components, how these “are integrated to achieve communication goals”,23 clarifying strategies, skills, and process tasks.
A similar pattern emerges in terms of the timing of the teaching of these skills, which overall seems to be approached in the basic cycle years when the contact with patients is either non-existent or very limited. Van Weel-Baumgarten et al.14 highlighted the importance of integrating, and how students benefit from learning and practicing communication skills at a pre-clinical level. In fact, results of their study, suggested that students perceive that these integrated learning experiences gave them a good background for clinical rotations. Previously, Van Dalen et al.24 had suggested significant higher scores on communication skills in students attending an integrated clinical skills programme with CCS, than students attending preclinical concentrated CCS courses.
It is of note that currently assessment in not well standardized. There are currently medical schools who have adopted CCS teaching and robust assessment models in all of their medical schools.25 In a study on how students perceive medical competences in Portugal and African Portuguese Speaking Countries, i.e. Angola and Mozambique,26 the communication skills domain revealed average scores. For Portuguese medical students, one of the domains with lower scores was communication skills. Mozambican medical students showed higher scores in overall competences than Angolan and Portuguese students. Students may perceive CCS as intrinsic to their future profession and assume they must be acquired.26,27 Researchers also argue that assessment measures26,28 that do not include direct observation of student performance with patients and team members, may cause students to base their perceptions exclusively on final grades.
The study participants also reported the need for faculty development programmes on CCS. The heads of the schools/medical education acknowledge that these skills are fundamental and must be more focused in their speciality courses and all seem to have plans for the new curriculum or restructuring of what is already going on in this field.15
Faculty of specific courses consistent with heads of medical schools or medical education noted that there is difficulty in the definition of specific objectives and identification of content areas that tailor the needs of each specific course. The teaching methods employed by faculty are similar to the methods used in medical schools in UK,25 and corroborating the previous set of interviews to heads of schools. The faculty reveal that assessment procedures are lacking or have little reliability and do not translate the importance of these skills in students’ training. Faculty also identify some concerns, namely, faculty training, variability in teaching and assessment methods, and the high number of students. These concerns are shared among the different schools and previous studies seem to corroborate these issues.20,25
Student interviews enabled a clear understanding of their perceptions of their CCS learning experiences throughout medical education. Specific issues were highlighted by the students, including: variability in teaching/role modelling, CCS teaching focused basically in pre-clinical years, and the lack of assessment. Rosenbaum & Axelson29 similarly discuss the issues of role-modelling, overemphasis on content in detriment to process and how this may lead to students adopting more closed ended questions in their interviews with patients. There are possible consequences of this on establishing rapport, diagnosis and treatment outcomes. In the attempt to examine third year medical students attitudes towards the acquisition of communication skills in a Portuguese medical school, Loureiro et al.17 observed that one of the main reasons for less positive attitudes is the lack of standardized assessment of the communication skills as they are taught in the basic cycle of the course.
According to recent reviews30,31 communication skills are one of the leading components for medical education and yet little attention has been given to doctor–patient relationship and team work in the medical curricula. Martins e Silva31 referring to Portuguese context of Medical Education, highlights the need to have a clear definition of a framework and strategies that will enable the integration of professionalism (and its components, in which communication is stated). The Core Graduates Learning Outcomes for Portuguese Angolan and Mozambican doctors,32–34 foresee interpersonal communication skills, although there are no guidelines or directives on how the skills/tasks listed should be taught or included in the medical curriculum.
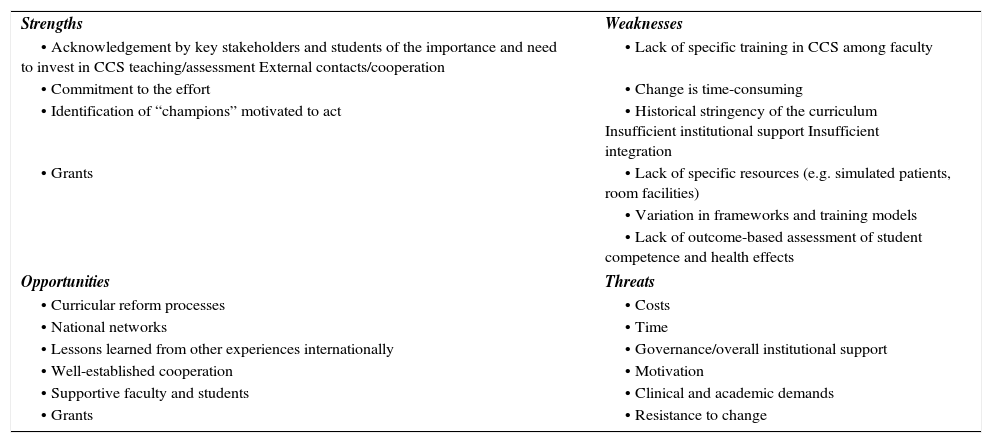
ConclusionThe results of this study enabled us to conduct a SWOT – strengths, weaknesses, opportunities and threats – analysis for the development of a framework of an integrated communication skills curriculum.
| Strengths | Weaknesses |
| • Acknowledgement by key stakeholders and students of the importance and need to invest in CCS teaching/assessment External contacts/cooperation | • Lack of specific training in CCS among faculty |
| • Commitment to the effort | • Change is time-consuming |
| • Identification of “champions” motivated to act | • Historical stringency of the curriculum Insufficient institutional support Insufficient integration |
| • Grants | • Lack of specific resources (e.g. simulated patients, room facilities) |
| • Variation in frameworks and training models | |
| • Lack of outcome-based assessment of student competence and health effects | |
| Opportunities | Threats |
| • Curricular reform processes | • Costs |
| • National networks | • Time |
| • Lessons learned from other experiences internationally | • Governance/overall institutional support |
| • Well-established cooperation | • Motivation |
| • Supportive faculty and students | • Clinical and academic demands |
| • Grants | • Resistance to change |
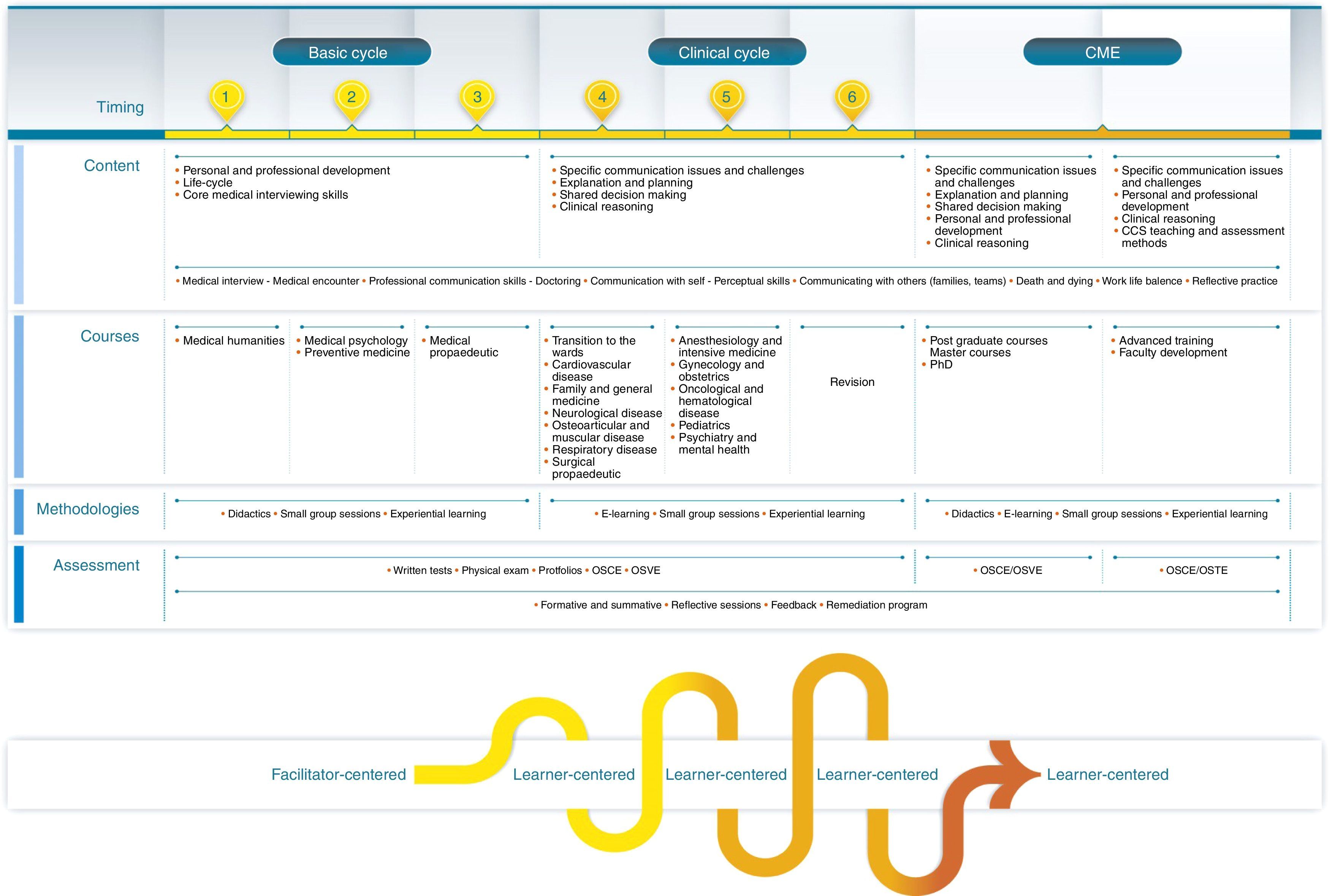
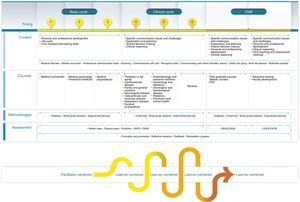
We further conclude that CCS training lacks a formal structure with considerable variation of the teaching process in Portuguese medical education, which evidences a similar scenario as many other countries. Results suggest the need to review timing, content, process and assessment methods of CCS teaching in Medical Education of these countries and those in similar situations, through the development of a framework of an integrated communication skills curriculum at both the undergraduate and postgraduate level. Although at the medical school in Porto, Portugal (FMUP) there already exists a Master Degree course on Clinical Communication, which is pioneer in the Portuguese context35 and considering its effective outcomes,36 we propose that at a post-graduate level of training, further investments on a PhD Course be made and that CCS be integrated as a module in master and PhD courses in biomedical sciences. We therefore suggest the implementation of a Communication Skills Teaching Programme for Medicine, CoSTProMED (Fig. 1), which was previously designed by the authors, and poses a comprehensive communication curriculum with clear learning objectives in coordination with the whole medical course as well as teaching and assessment methodologies to enhance and promote standardization of an educational encounter, to meet the accepted global minimum essential requirements and the general competencies in Medical Education.37,38 Research has demonstrated that longitudinal training of CCS promotes acquisition of more skills and their retention.24 Kaus et al.39 suggested that residents coming from medical schools with an integrated CCS curriculum had more positive interpersonal skills. Therefore, this type of curriculum should be helical as it “needs to provide opportunities for learners to review, refine and build on existing skills while at the same time adding in new skills and increasing complexity”.11
This study has some limitations, it is interview constructed so data is based on descriptions and interpretations. Interviews were not sent to the participants to validate the analysis. Further observational research may be suggested to explore discrepancies between the interviews from the heads of medical schools/medical education and students’ perceptions in terms of CCS. This study does not collect any data for the effectiveness of students’ CCS, which should be considered in new studies as well as monitor student and faculty attitudes towards the teaching and learning process of these skills. Future research should consider (i) the need to focus on the definitions of CCS, as the interviews revealed some inconsistency in the definitions the participants gave to the CCS, has also been raised by Hargie et al.25 and, (ii) the feasibility and performance-based outcomes of the implementation of an integrated curriculum.
In terms of practical implications of this study, we hope that the description of our experience in Portuguese medical schools, encourages other researchers from countries who are at a starting point in the development and integration of CCS in their medical education curricula to do likewise. These interviews enabled the characterization of the state of art of these competencies and most importantly, served to raise awareness among important stakeholders from the medical institutions about communication in medical education, and how these skills can enhance the quality of clinical practice. It is our hope that with these data, medical educators will have the ability to better identify and capitalize on opportunities to integrate and enhance higher academic credit to CCS in the curricula matched to the specific contextual needs of the countries involved, and can, for example, be taken from the Health Professions Core Communication Curriculum.11 This is also the time to leverage the various initiatives that exist for health communication especially in terms of medical education. As such, we recommend the implementation of the CoSTProMED – with a clear assessment of its efficacy and feasibility in future studies, suggest the development of national networks and task forces to optimize resources, know-how, and teaching, so as to try and overcome many of the common barriers identified and enable the “teaching of communication as a mainstream activity in medical schools and post graduate education”11,40,41 and contribute to increasing the quality and humanization of medical education.
Financial contributionsThis research was supported by the Portuguese Foundation for Science and Technology – FCT, through the project CostProMed – PTDC/SAU-SAP/112908/2009
Authors’ contributionsEL and MAF were the principal researchers, MB and SR were the research associates. MA, MF and IM acted as co-researchers. EL, MAF and MB contributed to the design of the study, EL to data collection, EL, MA and SR contributed to data interpretation. All contributed to the drafting of the article and read and approved the final manuscript.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank António Soares (AS), Madalena Abreu (MA) and Rui Encarnação (RE), for their assistance in data collection in Mozambique (RE) and Portugal (AS) and for content analysis of the interviews (AS & MA) respectively. We also thank all faculty and students who participated in this study.
Summary of results of interviews with heads of medical schools/course directors or heads of medical education departments.
| North of Portugal | Central/Interior of Portugal | South of Portugal | Angola | Mozambique | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |
| 1. Does the school has a CCS curriculum? | NO | NO | YES | NO | NO* | NO | NO | YES | NO | YES |
| 2. When does the CCS teaching occur? | 2nd Yr – Medical psychology & Preventive Medicine 3rd Yr – Semiotics | 2nd Yr – Human Physiology 3rd Yr – Medical Psychology, Semiotics, 4th Yr – Medicine, 5th Yr – Mental Health, Public health | Longitudinal throughout the course | 1st Yr – Introduction to Medicine, 3rd Yr – Medical Propedeutic | 1st Yr – Introduction to Medicine and Pathology 3rd Yr – Propedeutic 4th and 5th Yr – Skills Lab | 1st Yr – Introduction to Medicine, 2nd Yr Introduction to clinical practice, 3rd Yr – Internal Medicine, 4th Yr – Medical Psychology 5th Yr – Family Medicine | 1st to 3rd year in Clinical Medicine | At the admission process of the course and then longitudinally throughout the course | 3rd Yr – Semiology 4th and 6th Yr – Public Health and Medicine | At the moment in 1st and 2nd Yrs and gradually will be longitudinal throughout the course |
| 3. What is taught? | Medical Interview | How to communicate with patients, but specifically not sure of the content | How to communicate with patients and families, and how to deliver bad news | DK/S | DK/S | How to communicate with patients and teams, attitudes. Hoe to do oral presentations | What is a doctor, behaviours and attitudes | DK/S | Medical Interview and Heath Education | Medical Interview, Ethics, Delivering of bad news and health education |
| 4. How is it taught? | Lectures, Small group sessions, role-plays, role-modelling | Lectures, direct contact with patients, role-modelling | Skills lab, standardized patients, videotaped consultations (if students want), seminars, tutorials | Lectures, Hidden curriculum | Seminars, tutorials and skills lab | Videotaped, training, assessment and refection | Seminars, tutorials and simulation | Role-play, Skills, lab | Seminars, Observations of interactions, group work and role-plays | Role-modelling seminars, Role-plays and film observation |
| 5. By whom is it taught? | Psychiatrists, General Practitioners & Physicians from Internal Medicine | Psychiatrists, Psychologists, Physicians from Internal Medicine, Nephrology and Surgery | Psychiatrists, Psychologists, General Practitioners & faculty from social sciences | Psychiatrists and other physicians | Physicians | Psychiatrists and general practitioners | DK/S | General practitioners and invited experts from other institutions | Physicians | Physicians (psychiatrists) and Psychologists |
| 6. What training does the faculty have in CCS? | Little or non | None | Head of school – all have compulsory training Head of ME – DK/S | DK/S | DK/S | DK/S | DK/S | DK/S | None | None |
| 7. Are the CCS assessed? | Only in Medical Psychology | Yes, but no standard setting | Yes, with standard setting | Depends | Yes, but not eliminatory | Depends | Not formally | Yes | Formally no, only some subjective assessment | Not yet |
| 8. If assessed, what methods are used? | Audio-tape of interviews, discussions | General impression of the contact student made with patients or written tests | Depends on phase of course: written tests, reports, direct observation, feedback | Mini-CEX | Checklist for observation of video recorded interviews, role-plays, peer-assessment & discussion | 1st yr – videotaped role-plays 2nd yr – OSCE type General impression of student performance | CCS aspects included in the general check list of global assessment or included in a written test | At admission – stations Course – weekly assessment based on a checklist which includes many aspects of CCS | Subjectivity | NA |
DK – does not know/specify; NA – not applicable.
Summary of results of interviews with heads of specific curricular units of the course: what CCS are needed for the specific objectives of the CU.
| North of Portugal | Central/Interior of Portugal | South of Portugal | Angola | Mozambique | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |
| Clinical interview | NA | NA | Medical interview, types of questions, relate findings to the disease | NA | NA | NA | NA | NA | NA | NA |
| Communication workshops | NA | NA | Communication skills in clinical practice and team work, Verbal and non-verbal aspects of communication, dealing with patients’ emotions, Medical interview – family based | NA | NA | NA | NA | NA | NA | NA |
| Family medicine/community medicine/public health | General skills of doctor patient relationship in which the consultation is the main instrument | Medical interviewing skills, attitudes | Medical Interview, Communication with other health professionals, Active listening, | Versatility in the medical response in terms of prevention, education and risk awareness raising | Medical Interview, Empathy, establishment of a therapeutic relationship | Establishment of a therapeutic relationship, Non-verbal communication, medical interview skills, time management, communication with team members | Verbal and non-verbal communication skills, specific communication skills to enable better observation during consultations | Medical interview, empathy, active listening | Interpersonal communication (patient, community), Health education communication – behaviour modification | Interpersonal communication (patient, community), Health education communication |
| Gynaecology/obstetrics | Medical interview; sexual health, communication with patient and family, team communication | Delivering bad news, sexual history, delivering of clear information that the patient understands | NI/S | Use simple and clear language that can be understood by the patients | NI/S | Delivering bad news | NI/S | NA | Medical interview; communication with patient and family, | NI/S |
| Medical psychology | Medical interview, how to deal with strong emotions, motivational interview, how to communicate with families | Medical interview, delivering bad news, dealing with transfer and counter- transfer processes, understanding of illness | NA | NI/S | Adaptation of the dialogue to the development characteristics of the patients, Motivational Interview, essential elements of the communication process | Medical interview, doctor–patient relationship, empathy, active listening | NA | NA | NA | Establishment of therapeutic relationship with patients, Medical Interview |
| Medicine | How to deal with patients, families and end-of-life situations. | Medical Interview integrated with physical exam, attitudes, posture, intelligible dialogue | NA | NI/S | NI/S | How to communicate with patients, their families and team members | Approach the patient adequately, perform a good medical interview, structure the fundamental issues | NA | Medical | NI/S interview; communication with patient and family, team communication, delivering of clear information that the patient understands |
| PBL | NA | NA | NA | NA | NA | NA | NA | Always integrated – according to specifics of what is being taught | NA | Doctor–patient relationship, delivering bad news, dealing with challenging clinical situations. |
| Paediatrics | Medical interview with all possible people associated with child to fully understand medical problem and obtain possible information | medical Interview, How to talk and establish therapeutic relationship, how to behave in general with patients and families | Empathy, medical interview integrated with physical exam | Dialogue with parents in the presence of child or adolescent | Communication with parents, empathy and delivering of clear information that the patient/family understands | Communication with parents, empathy, trust and delivering of clear information that the patient/family understands, establishment of therapeutical relationship with child | Communication with children and families, double complicity, informed consent | NA | NI/S | NA |
| Psychiatry | Medical interview, Establishment of therapeutic relationship with patient, communication with families and other team members, observation of verbal and non-verbal aspects | NI/S | Medical interview | Verbal and non-verbal aspects of communication, establishment of therapeutic relationship with patients, communication with health professionals, delivering of bad news | NA | NA | NA | NA | NA | Establishment of therapeutical relationship with patients, Medical Interview |
| Semiotics/propaedeutic | Medical interview integrated with physical exam, delivering of clear information that the patient understands | Behaviour when with patients, establishment of a therapeutic relationship with patients | NA | NI/S | Informed consent, How to communicate with the patient in general terms, how to end a consultation, privacy setting | NA | NA | NA | Medical | NA interview |
| Surgery | Understand the psychological state of the patient, obtain best collaboration from patient and family, how to behave with patients | How to communicate with team, patients, their families (social and cultural adaptation), how to present clinical cases to team, | NA | NA | How to behave with patients, families, teams and clinical faculty, respect for intimacy, informed consent | NI/S | Communication with team and patient, deliver clear information that the patient understands | NA | Medical Interview, How to behave with patients, | NA |
NA – not applicable; NI – not identified/specified.
Summary of results of interviews with heads of specific curricular units of the course: what assessment methods are used to assess CCS of the CU.
| North of Portugal | Central/Interior of Portugal | South of Portugal | Angola | Mozambique | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |
| Clinical Interview | NA | NA | OSCE-type exam, with adaptation of Calgary Cambridge Guide, written exam, report | NA | NA | NA | NA | NA | NA | NA |
| Communication workshops | NA | NA | OSCE-type exam, with adaptation of Calgary Cambridge Guide, written exam, report | NA | NA | NA | NA | NA | NA | NA |
| Family medicine/community medicine/public health | Continuous assessment by tutor using a checklist with quantitative and subjective criteria | Continuous assessment by tutor using a checklist with quantitative and subjective criteria | Continuous assessment by tutor using a checklist with quantitative and subjective criteria; Oral presentations; Written exam; Checklist orientate for professionalism | MCQ | Mini clinical exam – weight of CCS not evident | Written test (1% CCS) Continuous assessment by tutor using a checklist with quantitative and subjective criteria | Report – weight of CCS not evident; Written exam (25% CCS); Tutor's perception – weight of CCS not evident | Continuous assessment – weight of CCS not evident | Not specific for CCS | Still not specific for CCS |
| Gynaecology/obstetrics | Not specific for CCS | Not specific for CCS | Written exam, physical exam with discussion, continuous assessment (subjective criteria) | Integrated in practical exam – a few items od CCS | Not specific for CCS (lack of resources and methods) | Not specific for CCS – Subjective assessment by tutor | Not specific for CCS (lack of resources and methods) | NA | Practical exam | Still not specific for CCS |
| Medical psychology | Use of SEGUE. assessment with simulated patient and of audio-taped interview with real patient | Report | NA | NI | MCQ | Informal assessment by tutor–has to have SUFICIENT to be admitted to written exam | NA | NA | NA | Still not specific for CCS |
| Medicine | Subjective criteria without weight on final classification | Practical exam, subjective criteria | NA | Practical exam, subjective criteria | Subjective criteria without weight on final classification | Not specific for CCS | Not specific for CCS | NA | Not specific for CCS | Still not specific for CCS |
| PBL | NA | NA | NA | NA | NA | NA | NA | OSCE | NA | Still not specific for CCS |
| Paediatrics | Not specific for CCS | Not specific for CCS | Continuous assessment by tutor using a checklist with quantitative and subjective criteria; Oral presentations; Written exam; Checklist orientate for professionalism | Practical exam with patient and family – CCS 10% weight on final assessment | Informally assessed, not sure of weight on final classification | Informally assessed, 60% attributed to communication, punctuality, interest and progress of knowledge, elaboration of clinical history. | MCQ – 1 question and report | NA | Not specific for CCS | NA |
| Psychiatry | 5th yr – Not specific for CCS 6th yr – subjective assessment by tutor | Continuous assessment by tutor using a checklist with quantitative and subjective criteria. Clinical competency and attitudes – 14/20 | NI | Not specific for CCS | NA | NA | NA | NA | NA | Still not specific for CCS |
| Semiotics/propaedeutic | CCC – 5% of written exam, practical part – Subjective criteria without weight on final classification | Continuous assessment – with checklist. Presentation of report with discussion | NA | Practical exam, MINI – CEX | Assessment in simulated environment, where CCS weigh 10 – 15% | NA | NA | NA | NI | NA |
| Surgery | Formative, continuous assessment of case presentation (with immediate feedback) | Assessment by tutor – not standardized | NA | NA | Not specific for CCS | Not specific for CCS | Not specific for CCS | NA | Not specific for CCS | NA |
NA – not applicable, NI – not indicated.
The research was conducted at the Faculty of Medicine of the University of Porto, Portugal (data was collected at all schools of medicine in Portugal, at the Faculty of Medicine of the University Eduardo Mondlane in Maputo, Mozambique and at the Faculty of Medicine of the University Agostinho Neto in Luanda, Mozambique).