An iatrogenic pseudoaneurysm of the superficial femoral artery was embolized with ultrasonographically guided thrombin injection. In order to avoid thrombin migration to the limb arteries, during the injection, the aneurysm neck was temporarily occluded, inflating a 5mm balloon. The balloon was deployed endovascularly with a crossover technique. At six months’ follow-up, the pseudoaneurysm remained occluded and the limb arteries were patent.
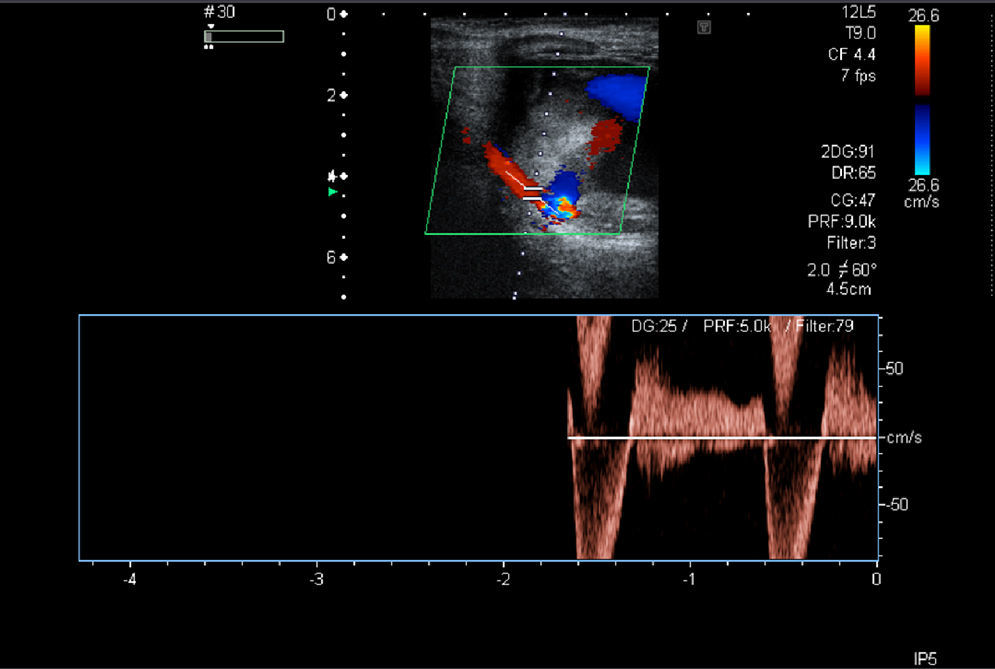
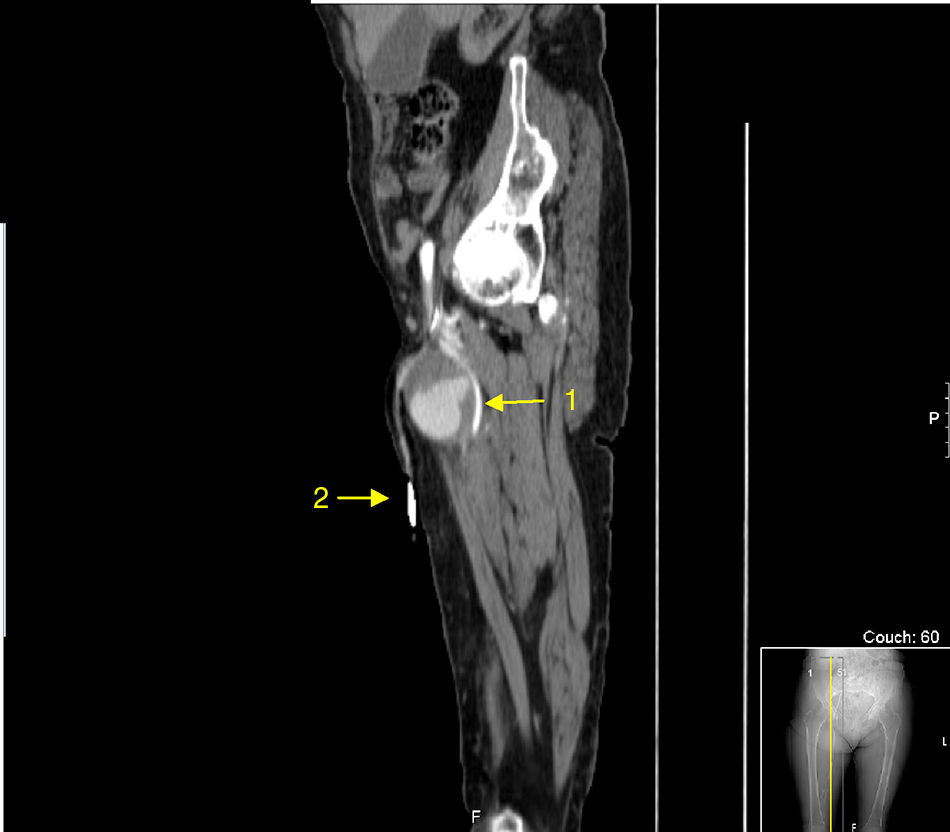
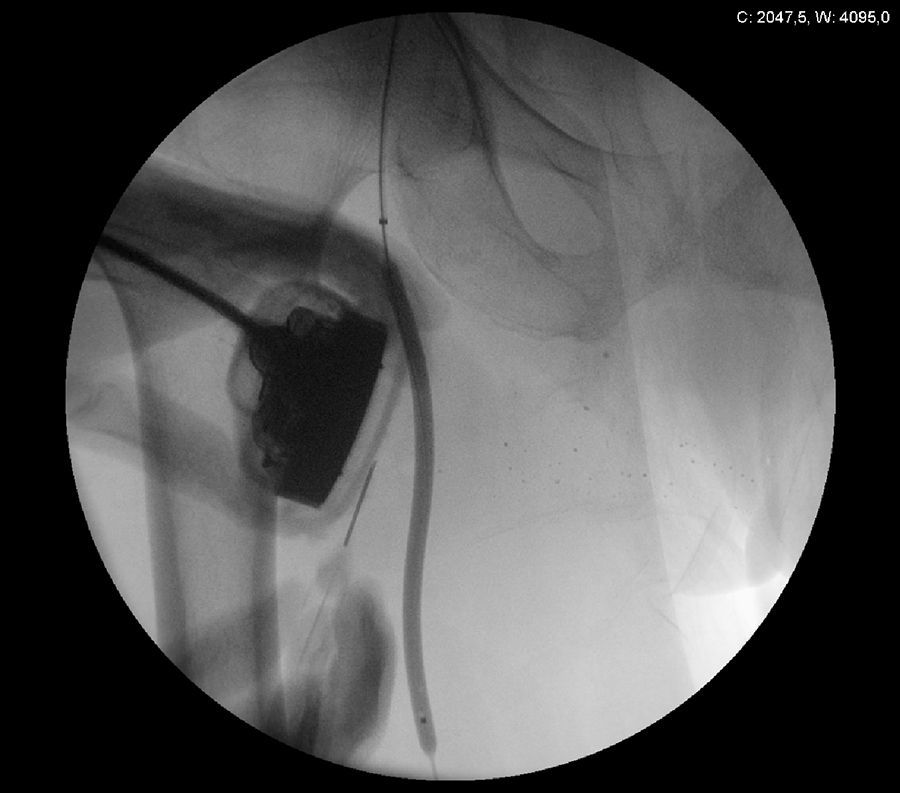
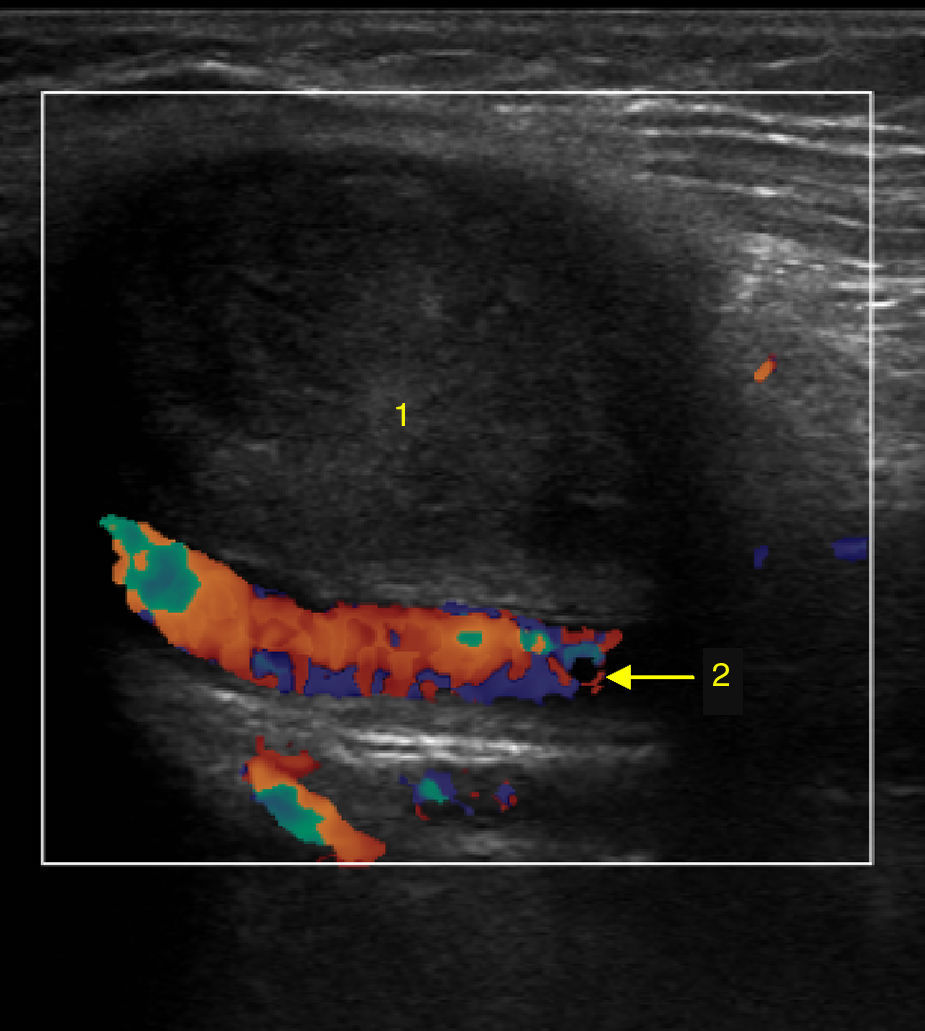
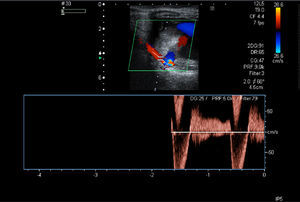
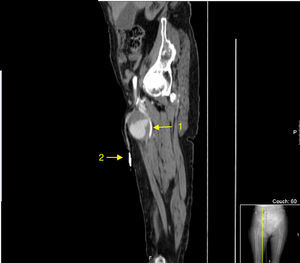
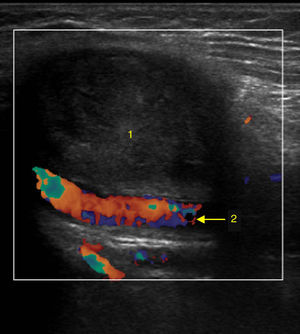
A 79-year-old female was admitted with a pulsating mass in the right thigh. Three months before, a temporary haemodialysis catheter had been inserted in the right common femoral vein. She underwent a Doppler ultrasound which showed a right superficial femoral artery pseudoaneurysm measuring 6cm×5cm with a 5mm×5mm×1mm neck (Fig. 1). In order to plan the pseudoaneurysm correction a CT scan was performed (Fig. 2). We decided to correct the aneurysm with thrombin injection, while the aneurysm neck was occluded with a balloon. The left common femoral artery was punctured. Using a crossover technique, a 5mm balloon was displaced at the right superficial femoral artery, near to the pseudoaneurysm neck. Percutaneous ultrasonographically guided thrombin injection was performed under real time color Doppler ultrasound monitoring. During the thrombin injection the balloon was inflated to occlude the aneurysm neck (20min in each thrombin injection) (Fig. 3). Injection was performed as far away as possible from the pseudoaneurysm neck. There were no complications and the pseudoaneurysm was excluded. Doppler ultrasound performed six months after the treatment, showed no blood flow in the aneurysm sac and the superficial femoral artery was patent (Fig. 4). The distal right limb pulses were present.
Pseudoaneurysms are frequently iatrogenic. The pseudoaneurysms can cause skin necrosis, neuropathy, deep venous thrombosis and can rupture.1 They should be excluded to avoid these complications. They can be treated with ultrasound-guided compression, surgical intervention, stent implantation or with percutaneous thrombin injection.2,3 Due to its minimally invasiveness, percutaneous thrombin is an appealing option.2 However, in pseudoaneurysm with short and large neck there is a risk of thrombin embolization to the nearby artery.3 In the case report described, thrombin embolization could cause acute limb ischemia. To minimize this risk, during the thrombin injection, the pseudoaneurysm neck was temporarily occluded with a balloon. In the case reported this was a valuable option.
Conflicts of interestThe authors declare no conflicts of interest.