Inspiratory muscle fatigue may inhibit healthy athletes to achieve maximum performance, compromising blood flow and perfusion on locomotor muscles. Recent studies have showed irregular influence of inspiratory muscle training (IMT) on resting lung function. It was hypothesized that a 4-week IMT protocol would improve pulmonary function of basketball players. Twenty-one female basketball players were randomly assigned to an experimental group (EG) (n=11) or a control group (CG) (n=10). Pre- and post-forced expiratory volume in first second (FEV1), forced vital capacity (FVC) and peak expiratory flow (PEF) were assessed with spirometry in the beginning of the sport's season, at the first day of protocol and four weeks after. The EG (22.00±5.00 years) was submitted to IMT using a threshold, 5 times a week, for a 4-week protocol (30 maximal repetitions (RM) against a pressure threshold load equivalent to 50% of maximal inspiratory pressure), while the CG (18.50±5.75 years) was not subjected to any intervention during the same period. Baseline sociodemographic and anthropometric characteristics were not significantly different with the exception of age (p=0.036). No significant differences were found in baseline pulmonary volumes (0.173≤p≤0.848) neither in predicted pulmonary variables (0.223≤p≤0.654). Significant increase on FEV1, FVC and PEF was found in the EG post-protocol (p<0.001). In the CG, an improvement of PEF was found (p=0.042). This type of specific inspiratory training appears to improve pulmonary function. Results suggest that the applied IMT protocol is effective. Further research is needed to assess the sustainability of the findings and to conclude the short and long term effects of IMT on basketball players.
Basketball is a team sport that requires a well-developed relation between strength, power, agility and speed.1 Many authors have suggested that it combines both aerobic and anaerobic pathways, despite the high-intensity activity intervals.2,3 During a game of basketball, upper limb muscles and trunk are engaged, either directly, to throw or pass the ball, or indirectly, to stabilize the core muscles along with the diaphragm, resulting in an increase in respiratory work and breathing perception.4 Inspiratory muscle fatigue inhibits healthy athletes to achieve maximum performance, impairing blood flow and blood perfusion on locomotor muscles, reducing maximal inspiratory pressure (MIP)4–6 and also resulting in a faster activation of the respiratory metaboreflex, originated in inspiratory muscles.7
Hence the importance of inspiratory muscle training (IMT), which has shown positive results in enhancing pulmonary O2 uptake during severe- and maximal-intensity exercise, leading to an increase in athletes’ tolerance to high-intensity exercise (30 maximal repetitions (RM) against a pressure threshold of 50% MIP, twice daily)8 as well as in the performance of wheelchair players9 and in pulmonary function of swimmers (30RM against a pressure threshold of 50% MIP, twice daily).10 The majority of IMT's positive outcomes appear between the fourth and sixth week of protocol, for example significant hypertrophy of the diaphragm.11
Little is yet know about the influence of IMT on high-intensity activity sports, particularly in basketball players, given this, it was hypothesized that a 4-week IMT would improve static lung volumes of these. This study aimed to investigate the influence of IMT in basketball players’ pulmonary function.
MethodsStudy designThis was a randomized controlled trial. Athletes were randomly assigned to the experimental group (EG) or control group (CG). For the allocation of groups the researcher resorted to sealed envelopes. Athletes were aware of the existence of two different groups, with different procedures.
The study was approved by the Research Ethics Committee of Fernando Pessoa University. All procedures were conducted in accordance with the Declaration of Helsinki prior to study commencement. After a detailed explanation of the aims, benefits and risks involved in this investigation, all participants provided informed consent. Participants were told that they could withdraw at any moment. The trial was reported according to CONSORT guidelines.12
ParticipantsParticipants were recruited from two basketball clubs from the main female basketball Portuguese league. These were included if they were professional basketball players able to provide informed consent. Exclusion criteria consisted of smoker athletes, athletes with any severe musculoskeletal, respiratory, cardiac and/or neurological pathology and athletes who did not complete 80% of the exercise sessions.
InterventionAthletes underwent 4 weeks of protocol in the beginning of the basketball season, between September and November 2015. They had the same work intensity, similar training protocols and returned to physical activity simultaneously. During this protocol, they were advised to maintain the training regimen and normal diet.
Participants’ characteristicsSociodemographic and anthropometric data were collected using a structured questionnaire, which included age, body mass index (BMI), occupation, and an inquiry about smoking, training habits and possible severe musculoskeletal, respiratory, cardiac and/or neurological pathologies.
Resting pulmonary functionThe following lung volumes were measured in all participants: forced expiratory volume in first second (FEV1), forced vital capacity (FVC) and peak expiratory flow (PEF) were assessed at baseline. Outcomes values were measured at the last day of protocol. These were recorded using a handheld spirometer (Microloop, Carefusion, Kent, San Diego, CA, EUA). The test begun by instructing the subject about the maneuver, demonstrating the appropriate technique and an inquiry about smoking, recent illness and medication use. For all maneuvers performed the subject was using a mouthpiece and a nose clip. Enthusiastic coaching of the subject was used throughout all maneuvers. FEV1 and FVC were recorded with the close circuit method, in a correct posture with the head slightly elevated, which should start in a maximal inspiration followed by a “blast” of expiration and a complete exhalation. PEF maneuver included a maximal inspiration followed by a blow, without any delay, while the athletes’ neck was in a neutral position.13 These variables were measured from a series of three, free from artifact, maneuvers with a resting period of 1min between repetitions. Data was examined from the largest curve performed or value obtained.
Inspiratory muscle trainingTraining begun by instructing the athletes on the usage of the inspiratory pressure threshold device for IMT (POWERBreathe IronMan Plus®, Warwickshire, UK). The training load used in this study is equivalent to 50% of MIP. In order to calculate the load, the threshold was placed at a minimum of resistance for the first session and increased at day two of protocol, only allowing athletes to perform 30 inspiratory efforts (30RM – 50% MIP).6 The training was performed in a standing position. Athletes were instructed to initiate every breath from residual volume in a powerful manner.4 The protocol consisted of 30 breathing efforts, 5 times a week during 4 weeks.11,14 For training progression, the inspiratory load would be increased by 10–15cm H2O once the subject had adapted (i.e., the subject was able to complete 30 maneuvers without any break).6 All IMT training sessions were applied by physiotherapists with knowledge in this subject as well as in the techniques and threshold used. Training load was recorded in a diary, with each sessions’ progress.
Statistical analysisData are presented as median±interquartile range (median±IQR). Due to the sample size comparisons between the two groups were performed with nonparametric tests, Wilcoxon test for paired samples was used to detect any statistically significant difference between the initial and final intervention in pulmonary function of these two groups.
Significance was set at p≤0.05. All these calculations were made using IBM Statistic Package for Social Science (IBM, Armonk, NY, USA, version 22).
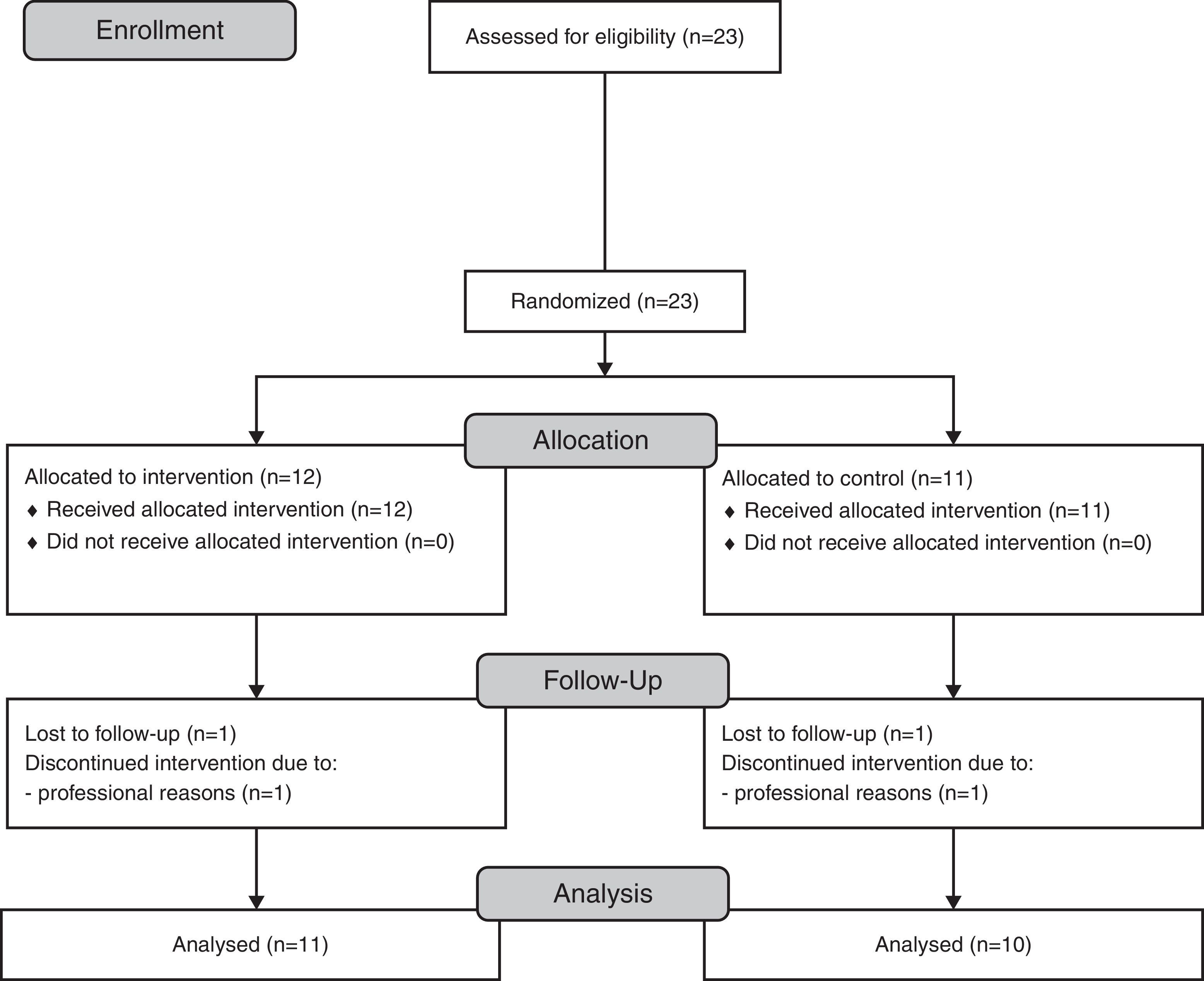
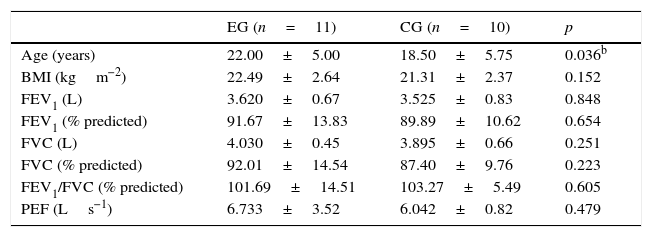
ResultsParticipantsTwenty-three competitive female players were screened (n=23) and allocated to the EG (n=12) or the CG (n=11). Two athletes were lost in follow-up in both study groups (n=1) due to professional reasons (Fig. 1). Final participants from the EG (n=11) had a mean age of 22.00±5.00 years and athletes from the CG (n=10) had a mean age of 18.50±5.75 years. Baseline sociodemographic and anthropometric characteristics were not significantly different between groups, with the exception of age (p=0.036) (Table 1). No significant differences were found in baseline pulmonary volumes (0.173≤p≤0.848, Table 1) neither in predicted pulmonary volumes (0.223≤p≤0.654, Table 1).15
Characteristics of participants from both study groups (n=21).a
| EG (n=11) | CG (n=10) | p | |
|---|---|---|---|
| Age (years) | 22.00±5.00 | 18.50±5.75 | 0.036b |
| BMI (kgm−2) | 22.49±2.64 | 21.31±2.37 | 0.152 |
| FEV1 (L) | 3.620±0.67 | 3.525±0.83 | 0.848 |
| FEV1 (% predicted) | 91.67±13.83 | 89.89±10.62 | 0.654 |
| FVC (L) | 4.030±0.45 | 3.895±0.66 | 0.251 |
| FVC (% predicted) | 92.01±14.54 | 87.40±9.76 | 0.223 |
| FEV1/FVC (% predicted) | 101.69±14.51 | 103.27±5.49 | 0.605 |
| PEF (Ls−1) | 6.733±3.52 | 6.042±0.82 | 0.479 |
BMI, body mass index; CG, control group; EG, experimental group; FEV1, forced expiratory volume in first second; FVC, forced vital capacity; PEF, peak expiratory flow.
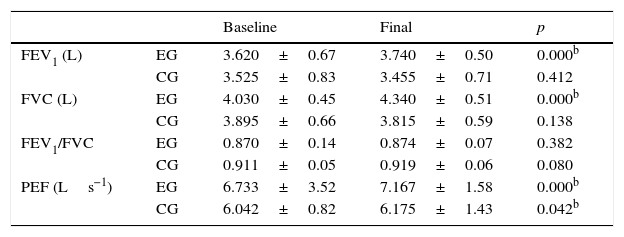
Table 2 shows the main findings. Protocol showed an increase in pulmonary function volumes FEV1 (p<0.001), FVC (p<0.001) and PEF (p<0.001) in the EG. An increase on PEF was observed in the CG (p<0.042) (Table 2).
Pulmonary function volumes comparison between baseline and final intervention in the EG (n=11) and in the CG (n=10).a
| Baseline | Final | p | ||
|---|---|---|---|---|
| FEV1 (L) | EG | 3.620±0.67 | 3.740±0.50 | 0.000b |
| CG | 3.525±0.83 | 3.455±0.71 | 0.412 | |
| FVC (L) | EG | 4.030±0.45 | 4.340±0.51 | 0.000b |
| CG | 3.895±0.66 | 3.815±0.59 | 0.138 | |
| FEV1/FVC | EG | 0.870±0.14 | 0.874±0.07 | 0.382 |
| CG | 0.911±0.05 | 0.919±0.06 | 0.080 | |
| PEF (Ls−1) | EG | 6.733±3.52 | 7.167±1.58 | 0.000b |
| CG | 6.042±0.82 | 6.175±1.43 | 0.042b |
CG, control group; EG, experimental group; FEV1, forced expiratory volume in first second; FVC, forced vital capacity; PEF, peak expiratory flow.
No correlations were found between normal range BMI and any lung volume in the EG (0.067≤p≤0.880) and CG (0.734≤p≤0.181).
DiscussionThis was the first randomized controlled trial that evaluated the impact of IMT on basketball players’ lung function. Furthermore, this was the first study to assess the effectiveness of IMT on female athletes’ lung function. Until this moment little was known about IMT's influence on resting lung function volumes, therefore the main aim of this study was to investigate the influence of IMT regarding those volumes. The main finding of this study was an increase of resting pulmonary volumes in the EG, particularly on pulmonary function (FEV1, FVC and PEF), confirming the original research hypothesis.
Previous studies based on IMT, showed a positive effect on FEV1, as demonstrated in this study, particularly a systematic review with meta-analyses that included 21 randomized controlled trials (p=0.02).5 Nevertheless, aerobic protocols may have a positive influence on FEV1 and FVC, as demonstrated in a study where healthy students were submitted to a 30min aerobic protocol per day, five days a week, over eight weeks (p=0.001),16 although all studied athletes had less than eight weeks of training practice.
A recent study where IMT was applied in 19 males for 8 weeks (60 RM against a fixed pressure threshold of 85% MIP) showed a positive evolution on MIP, maximal expiratory pressure (MEP) and PEF, but not in spirometric values such as FVC or in the Tiffeneau index. When that intervention was implemented MIP, MEP and PEF evolution was observed after 4 weeks of the 8-week protocol.17 The same result was reported here in the EG, however FVC showed a positive evolution in the current study. One possible explanation is that the 8-week protocol had a fixed MIP, instead of a moving MIP, allowing training maximization and a greater adaptation by the subject.6
A PEF improvement in the CG may be a result of regular aerobic exercise, since a 16-week protocol of five 20min sessions of running each week may lead to an improvement on PEF (p=0.07).18
Pulmonary function results may be explained by a decrease of the upper airway resistance for high volumes19 and a hypertrophy of the diaphragm.11
The increase in thickness was found after a 4-week IMT protocol (30RM – 50% MIP, twice daily).11 As it was expected the increase in thickness was accompanied by improvements in MIP (24%). Interestingly, the same magnitude of this change was observed after 4 and 8 weeks of training, yet changes in improvement in MIP differed. This indicates that diaphragm thickness is not the only source of change in MIP, which can also result of improvements in accessory muscles function as well as neural adaptations.6
This results could have a great practical implication because the costs related with this type of training are relatively small, therefore this intervention could be implemented in different basketball clubs, with the objective of improving each players’ pulmonary function.
LimitationsContrary results are presented by various authors that used similar protocols. This was a small-scale trial, therefore, generalizability of the results to clinical practice is limited.
Despite these limitations, the results presented show a positive tendency of IMT's influence on pulmonary volumes, thus a verification of the long-term effects using a larger sample size and a longer follow-up period should be considered for further studies. It is also necessary to verify the influence of pulmonary volumes on athletes’ performance. Finally, it is important to consider a sample from both sexes and different professional teams.
ConclusionsA 4-week IMT protocol leads to a positive evolution of basketball players’ pulmonary function. Further research with larger sample size and longer follow-up assessment period is needed to support these preliminary findings and assess the short- and long-term effects of this type of training on basketball players.
Conflicts of interestThe authors declare no conflicts of interest.
This work was supported in part by the Portuguese Foundation for Science and Technology (FCT – Fundação para a Ciência e a Tecnologia), through CIDMA – Center for Research and Development in Mathematics and Applications, within project UID/MAT/04106/2013.