As postulated by the stress process model, chronically stressed individuals, such as caregivers of people with chronic psychological disorders, have poorer cognitive performance and higher age-related cognitive decline than individuals not exposed to chronic stress. When analysing this topic in caregivers, the majority of research has been conducted in populations in which the care recipient has dementia and/or Alzheimer's disease, while relatively few studies have analysed cognition in caregivers of offspring with autism spectrum disorder (ASD). The main objective of this pilot study was to analyse the effect of a cognitive-behavioural intervention on cognition in caregivers of people with ASD. Specifically, we sought to gather evidence on whether there were clinically significant improvements in speed/attention, memory, and visuospatial, language and executive functions after the intervention. The participants were 17 parents (mean age of 52 years, 59% females) of ASD-diagnosed people who had cared for their offspring for approximately 14 years. The study had a pre-post design. After the cognitive-behavioural intervention, ASD caregivers had better selective attention, short- and long-term memory for words, stories and images, naming, cognitive flexibility and planning skills (p=.01 for all). Nevertheless, no changes were observed in general cognitive status, working memory for digits, verbal fluency, processing speed or inhibitory control (p>.05 for all). These findings underline the relevance of proper support and respite services to help caregivers cope with and reduce stress. A comprehensive neuropsychological assessment together with adjuvant domain-specific procedures and programmes to improve cognitive abilities are required to improve caregivers’ well-being and health.
Según los postulados del modelo del proceso del estrés, los individuos con situación de estrés crónico, tales como los cuidadores de personas con trastornos psicológicos crónicos, tienen un desempeño cognitivo más pobre y un deterioro cognitivo relacionado con la edad más acentuado que los individuos no expuestos al estrés crónico. Al analizar esta cuestión en los cuidadores, la mayoría de los estudios se han realizado en poblaciones en las que los receptores de los cuidados padecen demencia y/o Alzheimer, y pocos estudios han analizado la cognición en los cuidadores de los hijos con trastorno del espectro autista (ASD). El objetivo principal de este estudio piloto fue analizar el efecto de una intervención cognitivo-conductual en los cuidadores de personas con ASD. De manera específica, tratamos de reunir evidencia sobre las posibles mejoras con significación clínica en cuestiones tales como velocidad/atención, memoria y funciones visuoespaciales, del lenguaje y ejecutivas tras la intervención. Los participantes fueron 17 padres (edad media de 52 años, 59% de mujeres) de personas diagnosticadas de ASD que habían cuidado de sus hijos durante aproximadamente 14 años. El estudio tenía un diseño pre-post. Tras la intervención cognitivo-conductual, los cuidadores de las personas con ASD tenían mejor atención selectiva, memoria a corto y largo plazo en relación con las palabras, cuentos e imágenes, es decir, flexibilidad cognitiva y técnicas de planificación (p=0.01 en total). Sin embargo, no se observaron cambios con relación al estado cognitivo general, memoria operativa para cifras, fluidez verbal, velocidad de procesamiento o control inhibitorio (p>0.05 en total). Estos hallazgos subrayan la relevancia de un respaldo adecuado y de unos servicios de relevo que ayuden a los cuidadores a enfrentarse al estrés, y reducir el mismo. Se precisan amplias valoraciones neuropsicológicas y procedimientos y programas adyuvantes, específicos en la materia, para mejorar las capacidades cognitivas, así como el bienestar y la salud, de los cuidadores.
Over the years, the associations between chronic psychological stress and cognitive decline have been investigated in various different populations, including in caregivers of people diagnosed with a long-term psychological disorder (de Vugt et al., 2006; Mackenzie, Smith, Hasher, Leach, & Behl, 2007). The stress process model postulates that chronically stressed individuals have poorer cognitive performance and greater age-related cognitive decline than individuals not exposed to chronic stress (Scott et al., 2015).
The majority of research in caregivers has been conducted in populations in which the care recipient has dementia and/or Alzheimers’ disease, few studies having analysed cognition in caregivers of offspring with autism spectrum disorder (ASD). A number of studies have identified poor performance in processing speed, selective attention, working memory for digits, words and visuospatial information, learning words and long-term memory for words in caregivers of people with dementia, Alzheimers’ disease, stroke survivors, terminally ill family members, individuals with osteoporotic fractures and/or eating disorders compared to control participants (Caswell et al., 2003; Chen & Botticello, 2013; Corrêa et al., 2015; de Vugt et al., 2006; Mackenzie et al., 2007; Mcbean & Schlosnagle, 2016; Romero-Martínez, Ruiz-Robledillo, Moya-Albiol, 2016; Vitaliano, Ustundag, & Borson, 2016). Moreover, longitudinal studies have indicated that chronic stress in caregivers of people with dementia and/or Alzheimers’ disease tends to accelerate age-related cognitive decline in several cognitive domains, including general cognitive status and processing speed (Dassel, Carr, & Vitaliano, 2015; Vitaliano et al., 2009). Nevertheless, some research has produced contradictory or non-significant results in relation to general cognitive status, as well as IQ verbal, abstract reasoning, logical memory, verbal fluency and inhibitory control (Bertrand et al., 2012; Corrêa et al., 2015; de Vugt et al., 2006; Mackenzie et al., 2007; Vitaliano et al., 2009). Hence, it seems that not all the cognitive domains are equally sensitive to the effects of chronic psychological stress in this type of population.
Helping caregivers to cope with stress and burden, as well as develop good communication skills could help to protect against cognitive decline and even improve their cognitive performance. For instance, a previous study with caregivers of people with dementia demonstrated that cognitive behavioural therapy (through a 13-week intervention) resulted in clinically meaningful cognitive improvements. In fact, caregivers who finished the intervention programme experienced an improvement in attention, and in working and long-term memory for verbal and visual information after the intervention. Nevertheless, no improvements were observed in verbal or visual recognition, visual-spatial processing, verbal fluency, abstract reasoning or set-shifting (Mackenzie, Wiprzycka, Khatri, & Cheng, 2013).
Around 50–70 years of age, parents who are caregivers of offspring with disabilities also often experience more physiological dysregulation and chronic health problems than parents of normative children, and this may be linked to functional outcomes and may have an impact on their ability to provide adequate care (Romero-Martínez, González-Bono, Salvador, & Moya-Albiol, 2016). Our previous studies concluded that ASD caregivers (both men and women) had poorer declarative verbal memory, but they outperformed non-caregivers in inhibitory control and visuospatial skills (Romero-Martínez, Ruiz-Robledillo, et al., 2016; Romero-Martínez & Moya-Albiol, 2015). Moreover, this type of caregiver was found to have more retrospective and prospective memory failures (assessed by a questionnaire) in a diary over the course of a week than non-caregivers (Lovell, Elliot, Liu, & Wetherell, 2014; Mcbean & Schlosnagle, 2016). However, there is a gap in the scientific literature analysing whether cognitive-behavioural interventions, to reduce health complaints and stress levels, could be effective in offsetting normal age-related cognitive decline or even improving certain aspects of cognition in this population.
Our previous study with ASD caregivers demonstrated that a cognitive-behavioural intervention, which was adapted to the ASD care context, showed effectiveness to reduce somatic symptoms and level of depression and to improve mood states (Ruiz-Robledillo & Moya-Albiol, 2015). Hence, we considered that it would be interesting to assess whether this cognitive-behavioural intervention improved ASD caregivers’ cognition. In this sense, the main objective of our study was to examine cognitive domains that could be affected in caregivers and to compare the caregivers’ performance before and after the psychological intervention. Based on the results of Mackenzie et al. (2013) study, we hypothesized that ASD caregivers would obtain better scores in attention, working and long-term memory for verbal and visual information, but they would not show no changes in recognition (verbal or visual), visuospatial processing, verbal fluency, abstract reasoning or set-shifting after the intervention.
MethodParticipantsThe sample was composed of 17 parents (10 women and 7 men) of individuals diagnosed with ASD who had cared for their offspring for approximately 14 years. Participants’ mean age was 52.23±7.03 years, and body mass index was 27.88±5.46; most of them were married (76.5%), the others being divorced (11.75%) or widowed (11.75%), and most had a high level of education (61.9%). With regard to the care recipients, 13 were males and 4 females with a mean disability rating of 76% (as measured by the local government). Caregivers were recruited from members of an association for relatives of people with ASD (Asociación Valenciana de Padres de Personas con Autismo, APNAV) in the region of Valencia (Spain).
ProcedureEach participant in the study attended three sessions in the psychology laboratories of the University of Valencia. Firstly, a meeting was conducted with caregivers to explain the aim of the research and the criteria for participation, namely, being the mother or father of an individual with a clinical diagnosis of an ASD; living at home with the care recipient; and having been the primary caregiver (that is, the person with the greatest responsibility for the daily care and rearing of the child) for at least 2 years before the study. In this meeting, parents were told about the content and procedure of the neuropsychological assessment and the intervention programme. After indicating that they wished to participate in the study, selected parents were interviewed to collect demographic data and information about their caregiving status. After arriving at the laboratory, participants were taken to a room where they signed an informed consent form to participate in the study, and data were collected on anthropometric variables. Then, neuropsychological tests were administered, this being before the intervention programme (1 week before). Participants then attended the intervention programme. After the programme, the neuropsychological assessment was repeated (1 week after the end of the intervention), assessing the same neuropsychological variables.
Intervention programmeThe programme consisted of eight 2-hour sessions once a fortnight for 10 weeks. It is fundamentally based on a cognitive-behavioural approach adapted to the ASD care context, taking into account factors that have been shown to be modulators of health status in family caregivers of people with ASD, in order to increase its effectiveness in this population (for more details, see Ruiz-Robledillo & Moya-Albiol, 2015).
Neuropsychological assessmentThe Mini-Mental State Examination (MMSE) assesses cognitive function. Moreover, it is used to detect the progression of cognitive impairment related to neurodegenerative diseases (Crum, Anthony, Bassett & Folstein, 1993). It takes no more than 5–10minutes to administer. The normal MMSE score initially proposed is > 27 (Crum et al., 1993).
AttentionWe employed the Spanish version of the d2 test of attention, which measures the ability to focus on relevant stimuli while ignoring irrelevant stimuli (Brickenkamp & Zillmer, 2002). It consists of 14 test lines with 47 characters in each line, the characters being the letters “d” and “p”. Participants are asked to check the contents of each line from left to right for 20 seconds, marking only d's with two small dashes (both above, both below or one above and one below the letter). Scores used as dependent variables in this study were: total responses (TR); number of correct responses (TCR); omission errors (O); commission errors (C); total performance (TOT=TR−(O+C); concentration index (CON=TCR-C) and VAR, variation index (TR+−TR−).
MemoryMemory was assessed using the Wechsler Memory Scale-III (WMS-III) (Wechsler, 2004). It is a neuropsychological test designed to measure different memory functions. Three WMS-III subtests were used in this study:
Word List. This test includes four learning trials of 12 unrelated words each one, an interference list of 12 new words. Moreover, this test includes a delayed recall trial of the initial 12 words 25–35 minutes later.
Logical Memory. Logical Memory test is made of two brief stories, which are presented orally. Participants should recall each story immediately after it was read and again 25–35 minutes later.
Digit Span. In the first part, participants must repeat sequences of digits of increasing length have to be ed in the same order. In the second part, participants must repeat in reverse order digit sequences.
Rey–Osterrieth Complex Figure Test assesses visuospatial constructional ability and visual memory. Again, we considered all three test conditions: copy, immediate recall and delayed recall. Initially, participants must copy a stimulus card. Afterwards, the card is taken away and they are instructed to draw what they remember of the figure. Finally, participants are asked to draw the same figure again after 30minutes.
Language skills were assessed with the short form of the Boston Naming Test (Mack, Freed, Williams, & Henderson, 1992), which is made of 15 items (figures). Participants must say the names of the objects. The dependent variable employed in our study were the correct answers recorded.
A semantic category test was used, consisting of asking participants to say as many animal names (without repeat names) as they could in 60 seconds. It is scored by assigning 1 point for each correct animal name listed in that time interval, without a maximum score (Benton & Hamster, 1983). In addition, in an F-A-S phonemic verbal fluency test was employed, in which participants were asked produce as many words as possible beginning with each of the three aforementioned test letters in 60seconds (for each letter).
Executive functionsThe revised version of the WCST (Heaton, Chelune, Talley, Kay, & Curtiss, 2009) was used to measure cognitive flexibility. Cards must be sorted until six categories are matched or until all 128 cards are sorted. Cards are matched according to different criteria such as color, form, and number. After 10 consecutive correct cards are sorted, a new criterion is instituted without warning.
The Key search test and Zoo map are part of the Behavioural Assessment of the Dysexecutive Syndrome (BADS) battery, a series of tests that was designed to provide an ecologically valid measure of executive function, given concern about the low validity of other neuropsychological measures (Wilson, Alderman, Burgess, Emslie, & Evans, 1996). The Key search test was used to measure planning and problem-solving abilities. In this test participants are required to search for an imaginary key they have lost on a field (a square on a piece of paper). By drawing their search route, they provide an indication of their ability to plan and develop a search strategy. The time that the individual takes to do the task is also recorded. We employed the Zoo map to obtain a measurement about the ability of participants to elaborate a route that allows them to visit 6 of 12 locations in a section of a zoo.
Trail-Making Test, Parts A and B (TMT), was used to assess set-shifting. The first part (Part A) contains 25 numbered circles randomly arranged. In fact, individuals should draw lines between the circles in increasing sequential order finishing with the circle labelled “End.” The second part (Part B) contains the letters A–L and 13 numbered circles intermixed and randomly arranged. Individuals should connect the circles by drawing lines alternating between numbers and letters in sequential order, finishing with the circle labelled “End.”
The Stroop test (Golden, 1980) is used to assess interference/response inhibition. It consists of three forms, each one contains 100 elements. The first form contains the words “red”, “green,” and “blue”, which are printed in black ink. Moreover, these elements are ordered randomly. The second form consists of several letter “X” printed in red, blue, or green ink. For the second part, participants should name the colour. The third form introduces the condition of interference, and it consists of the words from the first sheet printed in the colours of the second. In this condition, participants have to name the colour of the ink and ignore the word.
Data analysesAfter assessing the normality of the data using the Shapiro–Wilk test (p<05), non-normal data were log10 transformed.
For neuropsychological variables, repeated measures analysis of variance was performed with time (pre and post) as the within-subject factor. Greenhouse–Geisser corrections for degrees of freedom and Bonferroni corrections for multiple comparisons were applied where appropriate. For significant results, partial eta squared (ηp2) is reported as a measure of effect size.
All statistical analyses were performed with IBM SPSS Statistics for Windows, version 22.0 (IBM Corporation, Armonk, NY, USA) with the alpha level set at 0.05 and a confidence level of 95%. The descriptive values are expressed as mean and standard deviation (M and SD, respectively).
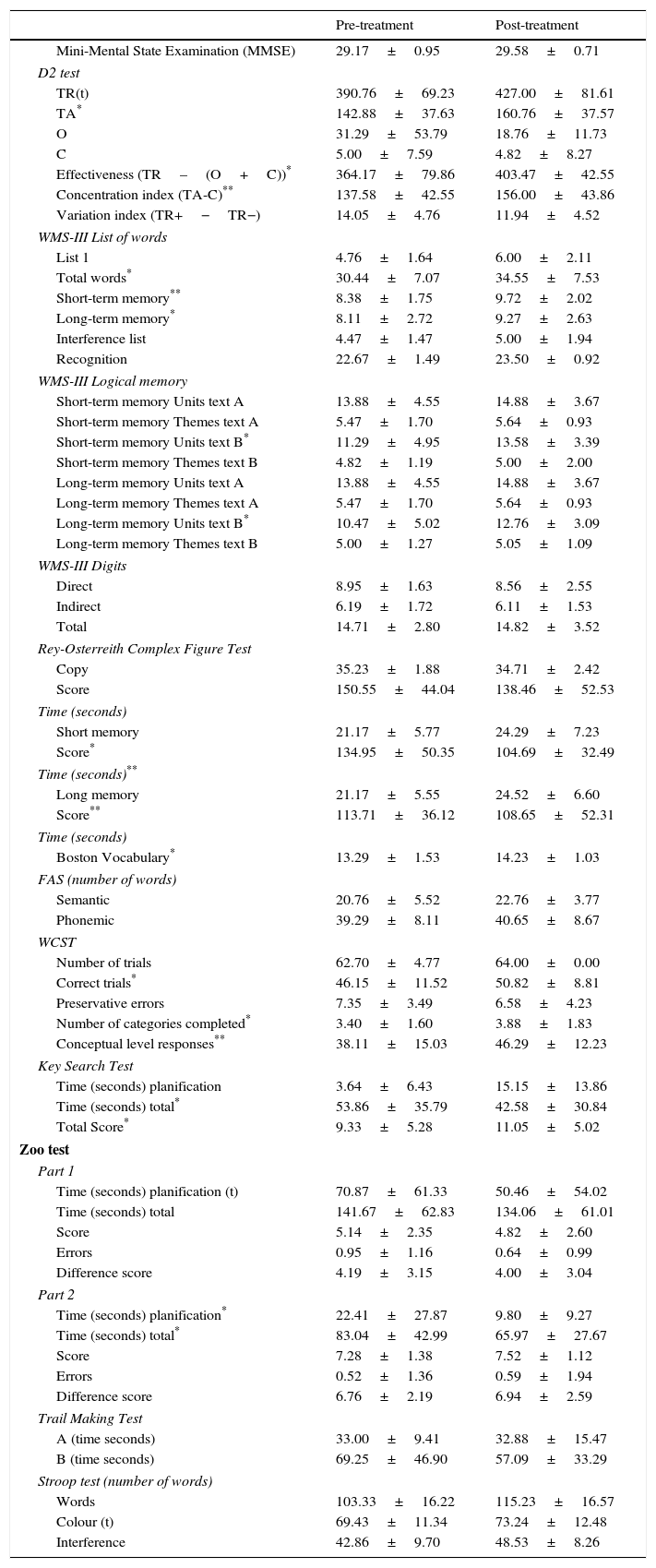
ResultsThe means and standard deviations of scores obtained by caregivers before and after the intervention are shown in Table 1.
Mean±SD of neuropsychological measures for caregivers pre- and post-treatment (without log10 transformation).
| Pre-treatment | Post-treatment | |
|---|---|---|
| Mini-Mental State Examination (MMSE) | 29.17±0.95 | 29.58±0.71 |
| D2 test | ||
| TR(t) | 390.76±69.23 | 427.00±81.61 |
| TA* | 142.88±37.63 | 160.76±37.57 |
| O | 31.29±53.79 | 18.76±11.73 |
| C | 5.00±7.59 | 4.82±8.27 |
| Effectiveness (TR–(O+C))* | 364.17±79.86 | 403.47±42.55 |
| Concentration index (TA-C)** | 137.58±42.55 | 156.00±43.86 |
| Variation index (TR+−TR−) | 14.05±4.76 | 11.94±4.52 |
| WMS-III List of words | ||
| List 1 | 4.76±1.64 | 6.00±2.11 |
| Total words* | 30.44±7.07 | 34.55±7.53 |
| Short-term memory** | 8.38±1.75 | 9.72±2.02 |
| Long-term memory* | 8.11±2.72 | 9.27±2.63 |
| Interference list | 4.47±1.47 | 5.00±1.94 |
| Recognition | 22.67±1.49 | 23.50±0.92 |
| WMS-III Logical memory | ||
| Short-term memory Units text A | 13.88±4.55 | 14.88±3.67 |
| Short-term memory Themes text A | 5.47±1.70 | 5.64±0.93 |
| Short-term memory Units text B* | 11.29±4.95 | 13.58±3.39 |
| Short-term memory Themes text B | 4.82±1.19 | 5.00±2.00 |
| Long-term memory Units text A | 13.88±4.55 | 14.88±3.67 |
| Long-term memory Themes text A | 5.47±1.70 | 5.64±0.93 |
| Long-term memory Units text B* | 10.47±5.02 | 12.76±3.09 |
| Long-term memory Themes text B | 5.00±1.27 | 5.05±1.09 |
| WMS-III Digits | ||
| Direct | 8.95±1.63 | 8.56±2.55 |
| Indirect | 6.19±1.72 | 6.11±1.53 |
| Total | 14.71±2.80 | 14.82±3.52 |
| Rey-Osterreith Complex Figure Test | ||
| Copy | 35.23±1.88 | 34.71±2.42 |
| Score | 150.55±44.04 | 138.46±52.53 |
| Time (seconds) | ||
| Short memory | 21.17±5.77 | 24.29±7.23 |
| Score* | 134.95±50.35 | 104.69±32.49 |
| Time (seconds)** | ||
| Long memory | 21.17±5.55 | 24.52±6.60 |
| Score** | 113.71±36.12 | 108.65±52.31 |
| Time (seconds) | ||
| Boston Vocabulary* | 13.29±1.53 | 14.23±1.03 |
| FAS (number of words) | ||
| Semantic | 20.76±5.52 | 22.76±3.77 |
| Phonemic | 39.29±8.11 | 40.65±8.67 |
| WCST | ||
| Number of trials | 62.70±4.77 | 64.00±0.00 |
| Correct trials* | 46.15±11.52 | 50.82±8.81 |
| Preservative errors | 7.35±3.49 | 6.58±4.23 |
| Number of categories completed* | 3.40±1.60 | 3.88±1.83 |
| Conceptual level responses** | 38.11±15.03 | 46.29±12.23 |
| Key Search Test | ||
| Time (seconds) planification | 3.64±6.43 | 15.15±13.86 |
| Time (seconds) total* | 53.86±35.79 | 42.58±30.84 |
| Total Score* | 9.33±5.28 | 11.05±5.02 |
| Zoo test | ||
| Part 1 | ||
| Time (seconds) planification (t) | 70.87±61.33 | 50.46±54.02 |
| Time (seconds) total | 141.67±62.83 | 134.06±61.01 |
| Score | 5.14±2.35 | 4.82±2.60 |
| Errors | 0.95±1.16 | 0.64±0.99 |
| Difference score | 4.19±3.15 | 4.00±3.04 |
| Part 2 | ||
| Time (seconds) planification* | 22.41±27.87 | 9.80±9.27 |
| Time (seconds) total* | 83.04±42.99 | 65.97±27.67 |
| Score | 7.28±1.38 | 7.52±1.12 |
| Errors | 0.52±1.36 | 0.59±1.94 |
| Difference score | 6.76±2.19 | 6.94±2.59 |
| Trail Making Test | ||
| A (time seconds) | 33.00±9.41 | 32.88±15.47 |
| B (time seconds) | 69.25±46.90 | 57.09±33.29 |
| Stroop test (number of words) | ||
| Words | 103.33±16.22 | 115.23±16.57 |
| Colour (t) | 69.43±11.34 | 73.24±12.48 |
| Interference | 42.86±9.70 | 48.53±8.26 |
In the case of cognitive screening tests, the psychological therapy was not found to be efficient for eliciting changes in MMSE scores.
Selective attentionA significant “time” effect was observed for d2 number of symbols processed, F(1, 16)=3.70, p=.07, ηp2=.19; number of correct responses, F(1, 16)=8.97, p=.009, ηp2=.36; effectiveness, F(1, 16)=5.32, p=.04, ηp2=.25 and concentration performance, F(1, 16)=8.10, p=.01, ηp2=.34, but not for omission errors, commission errors or the variation index. Specifically, it was found that caregivers obtained more correct responses and improved their effectiveness and concentration after the intervention programme.
MemoryWith regards to the WMS-III Word List subtest, the psychological therapy was shown to be efficient for eliciting variations in the number of words remembered in List 1, F(1, 16)=5.19, p=.04, ηp2=.25; total words, F(1, 16)=15.31, p=.001, ηp2=.49; short-term memory, F(1, 16)=22.42, p=.001, ηp2=.58; long-term memory, F(1, 16)=11.53, p=.004, ηp2=.42 and recognition, F(1, 16)=12.18, p=.003, ηp2=.43. In fact, caregivers remembered and recognized more words after the intervention than before. Nevertheless, there was no significant “time” effect for the interference list.
Regarding the Logical Memory subtest, the psychological therapy was shown to be efficient for eliciting variations in the short-term memory of story B units, F(1, 16)=4.42, p=.05, ηp2=.22; total words, F(1, 16)=5.27, p=.04, ηp2=.25 and long-term memory of story B units. Specifically, caregivers remembered more after than before the intervention. However, there were no significant “time” effects for short- or long-term memory of story B thematic unit; or short- or long-term memory of story A units and/or themes.
Regarding the WMS-III Digit Span subtest, there was no significant “time” effect for total score, direct or indirect order. This indicates that caregivers did not improve their ability to remember digits.
With regards to the Rey-Osterreith Complex Figure test, significant “time” effects were found for short-term memory score and time and long-term memory score, F(1, 16)=4.35, p=.05, ηp2=.21; F(1, 16)=8.23, p=.01, ηp2=.34; and F(1, 16)=9.05, p=.01, ηp2=.36, respectively. Specifically, caregivers obtained better scores and they took less time to draw the figure after than before the intervention. However, no differences were found in copy (score or time) or long-term memory time.
LanguageA significant “time” effect was found for the Boston Naming Test, F(1, 16)=6.50, p=0.02, ηp2=.29, with caregivers improving their performance after the intervention programme. Nevertheless, no significant “time” effect was observed for semantic or phonemic fluency. That is, caregivers improved in their ability to name objects, but they did not show an improvement in their verbal fluency.
Executive functionsA significant effect of “time” was found in WCST number of correct responses, number of categories completed and percentage of conceptual level responses, F(1, 16)=6.11, p=.03, ηp2=.28, F(1, 16)=7.09, p=.02, ηp2=.34 and F(1, 16)=9.28, p=.01, ηp2=.37, respectively. It was found that caregivers had more correct answers, more categories completed and higher percentages in conceptual level of responses after the intervention. However, no significant “time” effects were found for WCST number of trials, errors or preservative errors.
Regarding the Key Search test, a significant “time” effect was found for total time and total score, F(1, 16)=7.12, p=0.02, ηp2=.30 and F(1, 16)=4.94, p=0.04, ηp2=.24, but not for time planning, F(1, 16)=2.88, p=0.10, ηp2=.13. After the intervention, caregivers spent less time on the task (planning+execution) and obtained a higher score than at baseline.
With regards to the Zoo Map test, a significant “time” effect was found for time planning for part A, F(1, 16)=4.13, p=0.06, ηp2=.23, and for part B, F(1, 16)=14.59, p=0.002, ηp2=.53; and total time for part B, F(1, 16)=5.09, p=0.04, ηp2=.24, but not for total time for part A or total score for part A or B. Specifically, caregivers spent less time on planning and executing the task after the intervention, but their scores were similar at the two time points.
Regarding the TMT, no “time” effects were found for TMT A or B. This indicates that no improvement in processing speed was observed in the caregivers. Similarly, for the Stroop test, no significant “time” effects were found for words; colour; word-colour or interference. That is, there was no change in caregivers’ inhibition skills associated with the intervention.
DiscussionThe main aim of this pilot study was to gather evidence from caregivers who were willing and able to take part in cognitive-behavioural intervention on whether such an intervention could produce clinically significant improvements in their cognition, considering measures of speed/attention, memory, and visuospatial, language and executive functions. The study has demonstrated that ASD caregivers do have better selective attention, short- and long-term memory for words, stories and images, naming, cognitive flexibility and planning after the intervention. Nevertheless, their scores do not change in general cognitive status, working memory for digits, verbal fluency, processing speed or inhibitory control after this type of cognitive-behavioural intervention.
As neuropsychological tests included have shown a high test-retest reliability and stability over a 1-year period (Gagnon, Awad, Mertens, & Messier, 2003; Jelicic, Henquet, Derix, & Jolles, 2001; Lo, Humphreys, Byrne, & Pachana, 2012), it is highly probable that the changes observed in our study are attributable to the intervention programme, rather than limitations of the tests employed. Therapy seemed to have the strongest effects on selective attention, short- and long-term memory for words and stories, naming, cognitive flexibility and planning. This is in line with the results of Mackenzie et al. (2013), which demonstrated improvements in attention, and in short- and long-term memory for verbal and visual information after an intervention. On the other hand, unlike the study of Mackenzie et al., in our study, improvements were also observed in several other domains, namely, language (naming), set-shifting/cognitive flexibility and planning improved. This could be explained by several methodological factors including differences in the characteristics of participants (different types of caregivers), number of years caring, length of the intervention programme, and neuropsychological tests employed to assess these cognitive domains.
Cognitive-behavioural therapy that combines material oriented to problem-solving strategies and management of dysfunctional thoughts has shown effectiveness to reduce depression, burden and mood disturbances (Ruiz-Robledillo & Moya-Albiol, 2015), and such changes tend to be associated with improvements in attention and memory (Carpenter, Peters, Vastfjall, & Isen, 2013; Hubbard & Blyler, 2016). The changes in sustained attention and memory scores observed may mean that caregivers experience an improvement in their ability to focus on relevant information, switching between stimulus and inhibiting irrelevant information (García-Madruga, Gómez-Veiga, & Vila, 2016). Furthermore, there is a complex and reciprocal relationship between memory, attention and executive functions (McCabe, Roediger, McDaniel, Balota, & Hambrick, 2010). This is consistent with the assumption that cognitive flexibility and planning ability are sustained by properly functioning attention and memory resources (Tirapu-Ustárroz & Muñoz-Céspedes, 2005; Tirapu-Ustárroz, Muñoz-Céspedes, Pelegrín-Valero, & Albéniz-Ferreras, 2005). Thus, an improvement in memory and attention would tend to improve performance in executive functions.
It makes sense that the training in problem-solving strategies provided in our intervention programme would improve executive functions, especially cognitive flexibility and planning, as it has clearly been demonstrated in previous research in different populations (Areán et al., 2010; de Noreña et al., 2010; Kurowski et al., 2014). It has been suggested that specific instructions necessary for solving novel and complex tasks related to the caregiving situation. Hence, the observed improvement in cognitive flexibility (more correct answers after therapy) and planning ability (more time dedicated to planning and improvements in scores) could be explained by slower and controlled processing, step by step.
Lastly, the main limitation of our study is the small sample size; for this reason, the findings should be considered preliminary. Additionally, there was no control group, and comparison with controls would have helped to confirm that the observed changes were caused by the intervention and not by uncontrolled variables. Future studies should therefore assess several more reliable measures and explore these patterns in larger samples with a control group. Nevertheless, our data are novel as no studies have previously analysed the role of cognitive-behavioural therapy on the cognition of caregivers of people with ASD.
In conclusion, this study shows that the intervention programme for caregivers studied improved several types of socio-cognitive skills, these improvements being significant in the case of selective attention, short- and long-term memory, naming, cognitive flexibility and planning ability. These findings should be taken into account for understanding the impact of cognitive impairments on individuals’ ability to provide optimal caregiving. Our findings underline the importance of proper support and respite services to help caregivers cope with and reduce stress. Adjuvant domain-specific procedures and programmes to improve cognitive abilities are required if we want to improve caregivers’ well-being and health.
Conflict of interestThe authors have no conflict of interest to declare.