This article reviews the main results and conclusions of published studies concerning the influence of the knowledge and attitudes of health professionals in detecting and reporting elder abuse. Fifty-seven articles published in English or Spanish between 2000 and 2014 were analysed. The main findings and conclusions are presented around four themes: (1) the influence of definitions used by professionals in the detection and reporting of abuse; (2) the ability of knowledge and attitudes of professionals to act as barriers or facilitators of abuse detection and reporting; (3) the influence of the knowledge and attitudes of professionals in strategies for action taken in response to suspected abuse; and (4) training as a means to improve the competence of professionals to detect and report abuse. Results show the influence of knowledge and attitudes, but testing the theoretical models that integrate the relationship of these variables to other factors that affect decision processes and actions of health professionals is needed. Findings from such tests will facilitate the design of intervention strategies to increase the likelihood that health professionals will detect and report abuse.
Este artículo presenta una revisión de los principales resultados y conclusiones de los estudios sobre la influencia de los conocimientos y las actitudes de los profesionales de la salud en la detección y la notificación del maltrato a las personas mayores. Se analizaron 57 artículos publicados en inglés o en español entre los años 2000 y 2014. Los principales resultados y conclusiones encontrados se exponen en torno a 4 líneas temáticas: 1) la influencia de las definiciones utilizadas por los profesionales en la detección y la notificación; 2) el papel de los conocimientos y las actitudes de los profesionales como barreras o facilitadores de la detección y la notificación; 3) la influencia de los conocimientos y las actitudes de los profesionales en las estrategias de actuación ante la sospecha de maltrato, y 4) la formación como medio para mejorar la competencia de los profesionales para detectar y notificar. Los resultados de las investigaciones muestran la influencia de los conocimientos y las actitudes, pero sería necesario probar modelos teóricos que integrasen la relación de estas variables con otras que han demostrado influir en el proceso de decisión y en las actuaciones de los profesionales. Sus resultados facilitarían el diseño de estrategias de intervención para aumentar el número de casos detectados y notificados por los profesionales.
Elder abuse is a single or repeated act or lack of appropriate action that causes an older person harm or distress within any relationship where there is an expectation of trust (World Health Organization, 2002). Elder abuse represents a significant public health and social problem. Maltreatment of the elderly can produce serious consequences for their health and wellbeing, including reduced quality of life, psychological distress, loss of property and security, and increased morbidity and mortality. As the size of the aged population grows, the number of elder abuse cases is also likely to increase. In Europe, the proportion of people 65 years of age and older is predicted to grow from 14% in 2010 to 25% in 2050 (World Health Organization, 2011). The prevalence of elder abuse varies widely. A recent systematic review showed that in North and South America, the prevalence of elder abuse ranged from 10% in cognitively intact older adults to 47.3% in older adults with dementia (Dong, 2015). Meanwhile, the European Report on Preventing Elder Maltreatment (World Health Organization, 2011) showed that the prevalence of maltreatment in community-dwelling elders was high (about 3%) and might be higher (25%) for older people with high support needs. According to this report, older people receiving formal care either at home or in care settings were more vulnerable to maltreatment, with an average rate of 11% in the European Union (World Health Organization, 2011).
There is a general agreement that health professionals, especially doctors and nurses, have an important role in detecting and reporting abuse due to the nature of their contacts and relationships with the older people. Physicians and nurses are best placed to recognise these cases since most elderly people trust them (Almogue, Weiss, Marcus, & Beloosesky, 2010). These professionals are usually the first contacts of abuse victims may have with a medical or social service organisations or agencies and their ability to recognise the signs and symptoms of elder abuse is of utmost importance (Rinker, 2009). Because victims of elder abuse tend to be isolated, their interactions with physicians present critically important opportunities to recognise elder abuse and to intervene or refer the victims to appropriate providers (Lachs & Pillemer, 2015). However, professionals have difficulty recognizing suspected cases of elder abuse, and the percentage of reported cases is very low even when professionals suspect abuse (Yaffe, Wolfson, & Lithwick, 2009). Some studies have suggested that for every case of elder abuse reported, 23 go undetected (American Psychological Association, 2012). Despite mandated reporting laws that require health professionals to report elder abuse, health professionals have low rates of reporting.
Elder abuse has only recently been addressed in the medical literature (Kennedy, 2005). Little is known of how much the health professionals know and understand the problem (McCreadie, Bennett, Gilthorpe, Houghton, & Tinker, 2000), and reasons for lack of reporting are understudied. Underreporting appears to be related to the fact that the perpetrators of abuse are usually family members or carers, and of equal importance is a general community lack of understanding and health professionals’ lack of education in recognition of aged abuse (Joubert & Posenelli, 2009). Professionals report that lack of confidence and knowledge regarding defining, diagnosing, and reporting abuse are important barriers to managing abuse effectively (Cooper, Selwood, & Livingston, 2009). Professionals’ knowledge and skills have been considered a clear deficit in detection, and the education of medical staff has been identified as the most effective way of improving the recognition of cases of abuse (Joubert & Posenelli, 2009). Professionals’ attitudes also seem to influence their decision to report. Reluctance to report abuse unless certain that it had occurred, empathy with the abuser (if another professional), fear of the consequences of reporting, dissatisfaction with the authorities’ response to the reported abuse cases, and the lack of confidence in identifying or reporting geriatric victims of abuse or neglect have emerged as factors that can reduce reporting (Clark-Daniels, Daniels, & Baumhover, 1990; Jones, Veenstra, Seamon, & Krohmer, 1997).
We hypothesised that the knowledge and attitudes of health professionals regarding abuse could be factors that influence their ability to detect and report elder abuse, as well as their decisions and actions in response to suspected abuse. The final decision could be the result of an overall assessment of the case that includes very different factors. Knowing the most relevant knowledge and attitudes in the decision-making process and how they interact with other variables may provide guidance to implement interventions that medical staff could take to improve abuse detection and reporting. For these reasons, we decided to conduct an exploratory review on this issue.
The purpose of this exploratory review was to develop an overview of the main results and conclusions of published studies concerning the influence of the knowledge and attitudes of health professionals in detecting and reporting elder abuse. The main question that guided this review was: What are the main findings and conclusions of articles published between 2000 and 2014 on the relationship between the attitudes, knowledge, and actions of health professionals in detecting and reporting cases of domestic and institutional elder abuse? In our literature search, two systematic reviews were found that analysed studies on the influence of the knowledge of professionals in detecting and reporting abuse cases and the factors that influence decision making (Cooper et al., 2009; Killick & Taylor, 2009).
Cooper et al. (2009) conducted a systematic review to analyse health and social care professionals’ knowledge of elder abuse, their ability to detect it, and their willingness to report it. They also examined characteristics of staff and organisations that were associated with more abuse being reported and any interventions designed to increase these outcomes. This review included original research articles reporting quantitative data, and the search was made in PubMed and Web of Science databases in November 2008.
The review conducted by Killick and Taylor (2009) sought to identify research material relating to older people living in the community who were subjected to abuse by an informal caregiver. Their purpose was to analyse the factors that influence professional decision making at the point of first referral. Eight databases were used in the search process: Ageinfo, ASSIA, CINAHL, Google Scholar, Medline, Psychinfo, Social Care Online, SSA, and SSCI. Inclusion criteria referred to English language, 1995–2006 inclusive, and empirical research design.
The purpose of the review presented here is different from the aims set by the previous two reviews. Although the three reviews analyse variables that influence the detection and reporting of situations of abuse, this review focuses specifically on the influence of attitudes and knowledge of health professionals. The range of material that was considered was also different. This review included more recent publications and covered databases listing publications in English or Spanish. It incorporated data from both qualitative and quantitative studies within the same review, as well as theoretical essays. Studies about people living in hospitals or nursing homes and abuse by paid staff or caregivers were not excluded.
The results of this exploratory review may complement and extend the results of the previous two reviews. They can provide valuable information to design research and interventions that increase rates of detecting and reporting elder abuse, a prevalent and growing social problem with significant consequences on victims’ health and wellbeing.
MethodThis exploratory review was conducted according to the described phases for conducting exploratory reviews, with the exception of an optional consultation (Arksey & O’Malley, 2005; Armstrong, Hall, Doyle, & Waters, 2011). The search was conducted in the following databases: PubMed, CINAHL, Cochrane Library Plus, Latin American and Caribbean Literature in Health Sciences (LILACS), Abstracts in Social Gerontology, PsycINFO, PsycARTICLES, Violence & Abuse Abstracts, Family Studies Abstracts, Academic Search Premier, E-Journals, Spanish Medical Index (IME)-Biomedicina, Spanish Bibliographic Index in Health Sciences (IBECS), and ISOC-Social Science and Humanities. The English search terms used were the following: elder abuse, health personnel, health staff, health workers, perception, beliefs, attitudes, perspective, knowledge, practice. In Spanish, the following terms were applied: violencia, maltrato, malos tratos, mayor, anciano, tercera edad, viejo, vejez, profesional sanitario, salud, enfermera, médico, atención, práctica, intervención, conocimientos, creencias, actitudes, percepciones, perspectiva. Many of these terms were truncated and combined using Boolean operators. The searches were conducted following the parameters of each database, in the title, in the abstract, and in the descriptors.
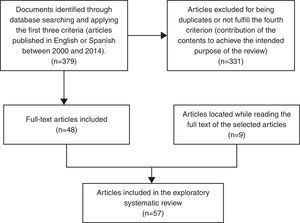
The inclusion/exclusion criteria were the following: (1) type of publication: articles; (2) publication period: from 2000 to 2014; (3) language of publication: English or Spanish; and (4) contribution of the contents to achieve the intended purpose of the review. Study quality was not used as an exclusion criterion in the selection. Unlike systematic reviews, exploratory reviews often do not make exclusions based on quality (Armstrong et al., 2011), because the priority is the contribution made in the review synthesis.
Fig. 1 shows the article selection process. Using the search terms previously stated and applying the first three criteria, 379 articles were obtained. After removing duplicate articles and those that did not meet the fourth criterion, 48 papers were selected for further analysis. While reading the full text of the selected articles, nine other publications were identified that met the inclusion criteria and were also incorporated in the review. Therefore, the total number of articles reviewed in this study was 57.
ResultsTable 1 provides information about the articles assessed in this review.
Selected articles for review.
| Authors and publication date | Country | Type of study | Sample | Information gathering techniques | Analysed variables | Main results |
|---|---|---|---|---|---|---|
| Ahern and McDonald (2002) | Australia | Descriptive | Registered nurses (n=95) | Questionnaire | Beliefs related to whistleblowing, patient advocacy and traditional roles of nursing | Whistleblowers supported the beliefs inherent in patient advocacy; nonwhistleblowers retained a belief in the traditional role of nursing |
| All (1994) | Theoretical essay | |||||
| Almogue et al. (2010) | Israel | Descriptive | Physicians and nurses working in the internal and geriatric services of a hospital and long-term facilities (n=157) | Questionnaire | Level of general knowledge of elder abuse; level of knowledge of protocols and laws; attitudes towards elder abuse; willingness to report suspected cases | Participants had a low level of knowledge of elder abuse issues, the relevant laws and regulations. No significant differences relating to the knowledge of elder abuse were found between nurses and physicians, nor between general and geriatric hospital employees. Both physicians and nurses tended to have neutral attitudes. Employees of geriatric hospitals had better attitudes than general hospital workers. The unwillingness to get legally involved had been the main reason of not reporting suspected cases |
| Bomba (2006) | Theoretical essay | |||||
| Bond (2004) | Theoretical essay | |||||
| Bover et al. (2003) | Theoretical essay | |||||
| Bužgová and Ivanová (2009) | Czech Republic | Descriptive | Residents and employees of residential homes, and managers (n=48); complaints about elder abuse (n=11) | Interview and analysis of complaints about employees | Employees’ and residents’ lived experiences of elder abuse | Two main dimensions of the examined phenomenon were identified: forms of elder abuse (rights violation, financial abuse, psychological abuse, physical abuse and neglect) and causes of elder abuse (institution, employee and client characteristics) |
| Caciula et al. (2010) | Romania | Descriptive | Care workers and clients of a non-government home care organisation (n=114) | Questionnaire | Identification of elder abuse and detection of elder abuse at work | Of the professionals, 11.4% had encountered a case of elder abuse, 5.7% in the last year. No staff and only one older person correctly identified all abusive strategies. Staff with more professional caregiving experience recognised fewer abusive strategies |
| Cohen and Shinan-Altman (2011) | Israel | Descriptive | Nursing aides from nursing homes (n=188) | Questionnaire | Work stressors, burnout (emotional exhaustion and depersonalization), attitudes to elder abuse, demographic and work-related variables | New immigrant nursing aides reported a higher tendency to condone abusive behaviours than did veteran nursing aides. Twenty-three per cent of the variance in attitudes was explained by group, demographics, work stressors and burnout. Greater condoning of elder abuse was associated with belonging to the new immigrant group, being unmarried and reporting higher work stressors. An interaction effect of work stressors×group was found. Burnout was correlated with greater condoning of elder abuse, but this association was not significant when the other variables were controlled |
| Coma et al., 2007 | Spain | Descriptive | Primary care doctors and nurses (n=27) | Focus groups | Definition, detection, risk factors, and management of elder abuse | The most frequent types of abuse were psychological and financial. Dysfunctional families, stressed and under-trained caregivers, and elder hostility were important risk factors. The profile of the abuser was associated with mental disorders, drug addiction and prior family violence in physical and financial abuse, but no clear profile was identified for neglect and abandonment. Detection was fruitless because social and health resources were insufficient and limited intervention. Education, monitoring and counselling of health professionals were needed to intervene effectively |
| Conry (2009) | Theoretical essay | |||||
| Cooper et al. (2013) | United Kingdom | Descriptive | Care workers from care homes (n=36) | Focus groups | Witnessed or perpetrated abuse | Participants reported that situations with potentially abusive consequences were a common occurrence, but deliberate abuse was rare. Behaviours witnessed could mostly be divided into three categories: (1) situations which the care workers thought were due to insufficient resources or competing demands; (2) instances when staff acted in potentially abusive ways, which they judged better for residents than alternatives; (3) situations related to institutional practices. The likelihood of abusive situations was determined by factors related to the institutions, the care workers, and the residents |
| Cooper et al. (2012) | United Kingdom | Descriptive | Trainee psychiatrists (n=40) | Questionnaire | The effectiveness of an educational elder abuse intervention over three months and its impact on professionals’ knowledge and practice regarding identification and management of potentially abusive situations | Compared with baseline, participants scored higher and identified more definitely abusive and possibly abusive situations immediately post-intervention. At three-month follow-up, participants reported higher confidence in managing abuse and considered it more frequently, but did not ask older people and their carers about abuse more frequently. Two participants detected abuse in the three months before the intervention, compared with 2 in the same period afterward |
| Cooper et al. (2009) | Systematic review | Professionals’ knowledge, detection, reporting, and intervention of elder abuse | Thirty-two articles were reviewed that included 21 surveys (of 5325 professionals), nine analyses of elder abuse reports to statutory bodies, and two intervention studies. Compatible results were pooled in a meta-analysis. Professionals underestimated prevalence of elder abuse and only a quarter of physicians knew the American Medical Association elder abuse guidelines. Of health care professionals, 33.7% had detected a case of elder abuse in the last year, and half of the detected abuse cases were reported. There was an association between recalling training in abuse and higher reporting rates. Face-to-face training was effective in increasing knowledge, although no intervention studies had investigated whether detection and reporting of abuse could also be increased through education. Current evidence would support the development and testing of interventions to increase professionals’ detection and reporting of abuse | |||
| Daly and Coffey (2010) | Ireland | Descriptive | Nurses and care assistants working in long-term care settings (n=114) | Questionnaire | Perceptions of elder abuse, level of education, how knowledge was gained on elder abuse, confidence about recognising elder abuse and desire to obtain further education on elder abuse | There was a high level of uncertainty about what constituted elder abuse |
| Daly and Jogerst (2005) | USA | Descriptive | Adult protective service caseworkers (n=302) | Delphi panel | Types of elder mistreatment, indicators of elder mistreatment per type, and demographic variables | The different types of abuse (emotional abuse, exploitation of finances and/or property, neglect, physical abuse, and sexual abuse) had some similar and some extremely different indicators that singly and together expanded their definition |
| Daly et al. (2012) | USA | Descriptive | Critical care nurses (n=10) | Interview | Types, suspicions, reporting, barriers to reporting elder abuse, legislation, and improvement in practice | Nurses reported the kinds of abuse they may encounter as emotional abuse, financial exploitation, neglect, and physical abuse. They reported being suspicious of elder abuse if the patient (1) depicted being malnourished and unkempt; (2) had bruising or other marks on the body with no reasonable explanation, (3) had burn marks in places where the patient could not reach, (4) could not provide a clear explanation/reluctance to answer questions, or (5) if a family member hovered or appeared uncomfortable with health care professionals present. In most instances, the nurses reported suspected abuse to the patient's physician or the unit's social worker and they did not know what happens after the allegation was reported. Reasons provided why patients were reluctant to report included: being scared, feeling they deserve the abuse, it may get worse when they get home, fear of being relocated to a nursing home or different institution, fear of abandonment, they did not want to get their children in trouble, dependence. Suggestions for improving the practice: conduct health history in private, ask safety questions on admission assessment, readdress the issue of elder abuse at discharge from the unit, establish the reporting of elder abuse as a priority for the unit, and offer elder abuse education in addition to that required by law |
| Davis and Konishi (2007) | Japan | Descriptive | Master's students and clinical teachers with BSN degrees at a nursing college (n=24) | Questionnaire | The meaning of and the experiences with whistleblowing | Fourteen nurses answered the hypothetical question of whether they would report another colleague saying they would report a nurse and six said they would not, but 17 said they would report a physician and only one said she would not report. Some nurses had already reported report a nurse or a physician in their work setting. Many thought that reporting nurses or physicians would result in someone taking action to change the situation, and that their nurse colleagues and their senior nurse would support them. When asked if physicians would support them if they reported a nurse, 10 said yes, but only six said yes if this involved reporting a physician. All the nurses who responded said they would whistleblow depending on the situation; this was especially true when considering reporting a physician. Reasons given for reporting were: the results of first going directly to the person whom they thought to be the wrongdoer; concerns about the effects of wrongdoing on the patient; and the belief that the head nurse should receive such information because she has overall responsibility for the hospital unit |
| Dow et al. (2013) | Australia | Descriptive | Health professionals from metropolitan health services and university health care students (n=247) | Questionnaire | Identification of elder abuse, demographic variables, been taught about identifying elder abuse or what to do in case of suspected elder abuse | Significantly more students than health professionals identified locking someone in the house alone all day and restraining someone in a chair as abusive. Tests found no statistically significant associations between demographic variables and identifying strategies categorised as abusive. |
| Dyer et al. (2005) | USA | Descriptive | Adult protective service workers (n=24) | Interview | Indicators, definitions and criteria of caregiver neglect and self-neglect, and demographic variables | The participants cited environmental filth, poor personal hygiene and health related factors as the three most common indicators. The definition of self-neglect was best generalised as an inability or unwillingness to provide for care for oneself. Neglect was defined as the failure of a caregiver to provide necessary goods and services to a client. When asked to distinguish between self-neglect and caregiver neglect, 44% of the respondents noted that the presence of a caregiver indicated caregiver neglect. Participants were generally comfortable validating self-neglect, but were concerned about falsely identifying a caregiver as neglectful |
| Ellis et al. (2014) | Theoretical essay | |||||
| Erlingsson et al. (2012) | Sweden and Japan | Descriptive | Community-based nurses and public health nurses (n=205) | Questionnaire | Nurses’ response patterns | Nurses’ response patterns in the aggregated data were similar across all three hypothetical cases. However, there were also differences between Swedish and Japanese responses. Swedish responses were generally practical, action oriented and involved increased levels of suspicion and personal intervention to achieve increased control. Japanese responses concerned better understanding that involved the family members and their situation, focusing on interventions grounded in collaboration |
| Gironda et al. (2010) | Theoretical essay | |||||
| Granville (2001) | USA | Descriptive | Registered nurses (n=372) | Questionnaire | The likelihood of reporting an intentional versus an unintentional wrongdoing | Perceived intentionality was related to questionable behaviour. The severity of the wrongdoing performed a significant role in determining whether or not an incident should be reported. Nurses indicated they would confront the wrongdoer about the unintentional incidents instead of reporting it to an immediate supervisor |
| Halphen et al. (2009) | Theoretical essay | |||||
| Hempton et al. (2010) | Australia | Descriptive | Health professionals from metropolitan hospitals, older volunteers and carers of older people with dementia (n=570) | Questionnaire | Perceptions of elder abuse | Significantly more health professionals than older people identified locking someone in the house alone all day, restraining someone in a chair and hiding medication in food as abusive. There were no significant differences between older volunteers and carers in their perceptions of elder abuse. A significant minority (40.8%) of health professionals and over 50% of carers did not identify locking the care recipient alone in the house all day as abusive |
| Hirst (2002) | Canada | Descriptive | Registered nurses working in urban long-term care institutions (n=10) | Interview and focus groups | Perceptions of resident abuse | Five categories of resident abuse characteristics emerged: perception of hurt felt by older residents, acts of omission or commission, context of care, intentional or unintentional, and behavioural clusters |
| Joubert and Posenelli (2009) | Australia | Descriptive | Hospital staff (n phase 1=166), (n phase 2=11), (n phase 3=11) | Questionnaire, interview and focus group | Hospital staff's response to aged abuse | Seventy-three per cent of participants were familiar with the concept of aged abuse; 14% had received any education or training on how to detect or manage this group of patients; 32% indicated that they had a good understanding while 54% said that they had a fair to poor understanding of aged abused; 47% had never suspected abuse in any of their elderly patients within the previous twelve months. Staff suspicion was aroused during their observation of the patient and their family or carer (22%), during routine assessment (46%) or when the elderly person was referred to them by another member of the staff (32%). The highest frequency of abuse suspected was ascribed to an adult child (39%) with the same frequencies reported for the spouse, carer, and residential care facility (10%). Information from interviews focused on three topics: staff perception of satisfaction with the care offered; ethical dilemmas faced by interviewees, and staff attitudes towards mandatory reporting. Four main themes emerged from the focus group: issues around the patient, issues around the carer, issues around the patient, issues around health care professionals and service provision, and issues around types of abuse |
| Kennedy (2005) | USA | Descriptive | Family physicians and general internists (n=392) | Questionnaire | Experience, knowledge and attitudes towards elder mistreatment | Nearly 72% reported no exposure or only minimal exposure to elder mistreatment. More than half of the participants reported that they had never identified a case of elder mistreatment. Participants estimated its prevalence as roughly less than 25% of the prevalence documented in the medical literature, and they were reluctant to accept the problem as universal. More than 60% reported that they had never asked their elderly patients about abuse. Family physicians tended to have a better knowledge of elder mistreatment and were more aware of management options |
| Kennelly et al. (2007) | Ireland | Descriptive | Non-consultant hospital doctors working in internal medicine and medical social workers (n=39) | Questionnaire | Understanding of the term elder abuse, its perceived prevalence, attitudes, identification of potential risk factors, training received, awareness of the existing government policy, the frequency of exposure to cases and their management | Forty-five per cent had never heard the term “elder abuse”, and 30% had read any literature at any stage on the topic. No doctors had ever received any formal training, and only one doctor had heard of guidelines for its management. Eighty-five per cent felt elder abuse was common, and all felt it was under-reported. Eighty-five per cent of doctors had treated at least one suspected case of elder abuse in the last year. All MSWs had read literature or had received formal training on the topic, 58% were aware of management guidelines, however only 10% were able to name them. Both groups said they sought the advice of senior colleagues when managing suspected cases of abuse and 46% of the participants would feel uncomfortable using the label of “elder abuse” |
| Killick and Taylor (2009) | Systematic review | Factors influencing professional decision making at the point of first referral | Nineteen articles were reviewed. The factors identified by the research were classified into three categories: case factors, professional factors and agency factors. The studies identified case factors relating to the victim, the caregiver, and the wider social and economic situation. The frequency and severity of abuse received little attention. The majority of included studies focused primarily on practitioner factors. The influence of agency factors was addressed by only two of the included studies | |||
| Ko and Koh (2012) | South Korea | Descriptive | Hospital nurses (n=365) | Questionnaire | Willingness to report suspected elder abuse and its related factors | Of the participants, 18.6% were not willing to report suspected elder abuse. Fewer years in clinical work, a higher level of knowledge on elder abuse law, and the perception of more severe abuse were found to be significant predictors of willingness to report elder abuse |
| Leddy et al. (2014) | USA | Descriptive | Obstetricians and gynaecologists (n=122) | Questionnaire | Knowledge, attitudes, and practice regarding elder abuse | Eighty-one per cent had never reported a case of abuse. Younger males reported different clinical practice patterns than other groups. Generally, participants were knowledgeable about risk factors and issues about elder abuse, but several knowledge gaps were identified. Most considered that elder abuse screening was within their professional purview. Half of the respondents cited time constraints as a barrier to screening |
| Liao et al. (2009) | USA | Descriptive | Hospice and palliative care professionals and adult protective service workers (n=96) | Questionnaire | Differences in elder mistreatment reporting threshold, and factors for not reporting elder mistreatment | Significant differences were found in the threshold of reporting between APS and HPC professionals in all the mistreatment cases but the most severe. APS was more likely to accept reports of elder mistreatment. HPC professionals had reported a mean of 2.52 (±2.79, SD) cases in the last 5 years, 33.3% had not reported a single case in the last 5 years, 24.1% had not suspected any cases of mistreatment in the last 5 years, and 29.6% had suspected cases that they did not report. The median difference between the total number of suspected and reported cases was 2 (±4.6, SD). Eleven per cent had ethical concerns about reporting and 63% were concerned about practical consequences of reporting. Thirty-seven per cent correctly identified the reporting agencies that have jurisdiction over abuse that occurs in long-term care. Correct identification of long-term care reporting agencies correlated with whether the HPC professional had training in elder mistreatment (r=0.35, p=0.009). Ninety-six per cent would report physical abuse that they witnessed, and sixty-three would report abuse verbalised by the patient |
| Malmedal et al. (2009) | Norway | Descriptive | Nursing staff in nursing homes (n=616) | Questionnaire | Attitudes on reporting acts of inadequate care, age, education, and length of experience of working in the healthcare services | Participants held a positive attitude towards reporting acts of inadequate care committed by their colleagues. There were significant differences between the age groups and between educational levels regarding the attitudes of staff towards reporting. Compared with younger staff, the older staff seemed to be more reluctant to report colleagues, to feel less brave, to be more afraid of what would happen to them if they reported, and to agree that it is best to deal with such matters internally. Regarding education, it seemed that a higher educational level was related with a more positive attitude towards a willingness to report and less fear of negative sanctions. There were significant differences between groups with varying lengths of experience in respect of two statements: “It is no use reporting anything; nothing will happen anyway” (p=0.009) and “It is best to deal with such matters internally” (p=0.003) |
| Mandiracioglu et al. (2006) | Turkey | Descriptive | Emergency health care providers teams (n=125) | Questionnaire | Knowledge, attitudes, and beliefs towards the identification and management of abused older people | Of the respondents, 13.6% had never identified an abused older person. The health care personnel working at university emergency department had a better knowledge than state hospital personnel about elder abuse. There was a significant difference on the “willingness to report abuse” scores between physicians and nurses. Most of the participants felt uncomfortable in asking questions about older people abuse. A majority of them believed that it is the older person's responsibility to report their symptoms related abuse. Most of the participants perceived elder abuse to be uncommon in Turkey and 24% reported they had not received formal training on older people abuse |
| McCool et al. (2009) | USA | Descriptive | Employees of nursing facilities (n questionnaire=49) (n interview=22) | Questionnaire and interview | Demographic data, personal experiences with suspected elder abuse and reporting, legislation, facility protocols, and opinions on mandatory reporting | Fifty-three per cent of the respondents reported that they have suspected a case of elder abuse; 35% of those respondents indicated that they did not report all the cases of abuse they have suspected. Most of the respondents answered correctly the questions about reporting abuse and consent. Four themes emerged from the interviews: the need for more staff education/training; difficulty in making judgments about whether the situation needs to be reported; barriers to reporting, and a sense that some abuse situations may occur because the staff is overworked, inexperienced, and/or frustrated from dealing with difficult residents |
| McCreadie et al. (2000) | United Kingdom | Descriptive | General practitioners (n=291) | Questionnaire | Demographic characteristics, practice characteristics, home visiting, education, training, and diagnosis of abuse | Forty-five per cent had diagnosed elder abuse in the previous year. The strongest factor predicting diagnosis of abuse was knowledge of five or more risk situations |
| Meeks-Sjostrom (2013) | USA | Descriptive | Registered nurses (n=84) | Questionnaire | Applied knowledge (assessment cues) of elder abuse, use of intuition in nursing, years of experience as a RN, clinical level of practice status, and the clinical decision outcomes (interventions) | RNs applied knowledge (assessment cues) and years worked as a RN significantly predicted clinical decision outcomes (interventions), There were no differences in applied knowledge (assessment cues) of elder abuse, intuition use in nursing, years working as a RN, clinical level of practice status, and clinical decision outcomes (interventions) between RNs who received elder abuse education at orientation and those who did not receive the education |
| Pillemer et al. (2011) | USA | Descriptive | Academic research experts and practitioner experts | Research-to-practice consensus workshops | Recommendations from expert practitioners and researchers regarding future directions for research on elder abuse prevention | Ten key recommendations for future research were proposed. The recommendations included the following priority areas: defining elder abuse, providing researchers with access to victims and abusers, determining the best approaches in treating abusers, exploiting existing data sets, identifying risk factors, understanding the impact of cultural factors, improving programme evaluation, establishing how cognitive impairment affects legal investigations, promoting studies of financial and medical forensics, and improving professional reporting and training |
| Richardson et al. (2002) | United Kingdom | Randomised controlled trial | Nurses, care assistants and social workers (n=64) | Questionnaire | Type of training (attending an educational course vs. printed educational material) knowledge and management of abuse, attitude towards people with dementia, and burnout | There was a lack of knowledge of good management in dealing with elder abuse. Those who attended an educational course improved their knowledge after the intervention. There was a ceiling effect with those who knew more learning less. Attending and educational course and low baseline knowledge predicted learning. Positive attitude towards people with dementia correlated with baseline knowledge, but did not predict knowledge |
| Rinker (2009) | USA | Descriptive | Emergency medical services and hospital care providers (n=400) | Questionnaire | Perception, knowledge and ability to identify patients that were potential victims of elder abuse and/or neglect | During the past 12 months, 51.3% of those surveyed did not have reason to suspect abuse or neglect, participants (83.5%) believed a decubital ulcer was a positive indicator of abuse/neglect and 92.8% indicated that the elderly could suffer from injuries similar to “shaken-baby syndrome”. Sixty-nine per cent identified skin bruises as a possible indicator of abuse, and 71% indicated that burns are not common in the elderly and could be another sign of elder abuse. One-in-three providers indicated they would suspect other reasons (dementia, depression, etc.) for the report of a sexual assault in an elderly patient. The majority (89.0%) of respondents knew that they were obligated to report cases of (suspected) elder abuse or neglect to law enforcement or social services personnel. Sixty-six per cent of the respondents felt that elder abuse was a medical problem, whereas 20.3% felt it was a social problem. Over 95% of the participants suspected the existence of abuse, neglect and domestic violence among the elderly were not rare events |
| Rodriguez et al. (2006) | USA | Descriptive | Primary care physicians (n=20) | Interview | Physician's perspectives on mandated reporting of elder abuse | Paradoxes emerged from analyses of interview transcripts related to 3 topical areas: physician–patient relationship; increase and decrease in patient quality of life; and presence and loss of physician control. All 20 physicians referred to these paradoxes. These paradoxes appeared to be primarily hidden or unconscious, yet they influenced the conscious decision process of whether to report |
| Sandmoe and Kirkevold (2013) | Norway | Descriptive | Nurse managers and department managers (n=52) | Interview | Identification and handling of abused older clients | Half of the participants had identified cases during the previous year, but the interviews indicated that abuse was discovered more often than the participants stated. The role of the participants in identifying abuse cases was not clear. Identification and handling of abused older clients was based on clinical experience and less on knowledge through professional training and education. The participants emphasised the importance of individualising interventions, taking appropriate action depending on the severity of a situation and finding a solution that was satisfactory to both the victim and abuser. All participants stated that interdisciplinary collaboration was primarily limited to discussion and counselling. Several participants found that few people were willing to play an active role in case management. In general, the participants believed that handling neglect cases was appropriate, whereas strategies for handling financial abuse were described as insufficient and very difficult to access |
| Sandmoe et al. (2011) | Norway and Australia | Descriptive | Nurses, auxiliary nurses and care workers (n=20) | Interview | Handling of abused older clients | The similarity of the information obtained in the two countries was very high. The nature of the interventions differed based on the type and seriousness of the abuse and the participants’ considerations of the client's cognitive capacity. The participants experienced the intervention as a long-lasting process with changing goals and problem-solving activities that displayed phases of improvement and aggravation; however, some cases also called for immediate action. The clients’ and caregivers’ attributes, relationships and life contexts were important factors and constituted the premises for the participants’ intervention. Financial abuse was a more prominent issue in Australia than in Norway. The managers’ support and the elder protective services were of great importance to the nurses |
| Schmeidel et al. (2012) | USA | Descriptive | Nurses, physicians, and social workers (n=23) | Interview | Professionals’ perspectives on elder abuse | All professions reported emotional, financial, mental, neglect, physical, psychological, spousal, and verbal abuse as the kinds of abuse they may encounter. In addition, physicians reported isolation and sexual abuse. Social workers also mentioned self-neglect. Analysis of participants’ statements about barriers to detecting and reporting revealed five major categories: professional orientation, assessment, interpretation, systems, and knowledge and education |
| Shefet et al. (2007) | Israel | Descriptive | Physicians, residents and specialists in relevant primary care fields, from both outpatient and inpatient settings (n=150) | Questionnaire | Self-perception of knowledge and skills, reported case management, and perceived intervention barriers | Perception of knowledge and skills, routine screening frequency and reported case management all demonstrated significant improvement between baseline and follow-up. A clear trend to elevation in detection, evaluation and referral rates was found. Ranking of intervention barriers was compared with baseline values and lack of knowledge, lack of skills and psychological difficulties diminished significantly, which indicated an improvement in the physicians’ attitudes regarding these barriers |
| Shinan-Altman and Cohen (2009) | Israel | Descriptive | Nursing aides from nursing home (n=208) | Questionnaire | Demographic variables, work stressors, burnout, perceived control, and attitudes condoning elder abuse | The mean score of attitudes condoning elder abuse of 3.24 (SD=0.59) on a 1–4 scale indicated a relatively high tendency to condone abusive behaviours. Condoning abusive behaviours were closely associated with higher levels of work stressors, burnout, and low income. Multiple regression analyses showed that demographic variables, work stressors, burnout, and perceived control explained 16% of the variance of attitudes condoning elder abuse. Burnout was a partial mediator in the relationship between the work stressors variable and the attitudes condoning elder abuse |
| Sociedad Española de Geriatría y Gerontología (2004) | Spain | Descriptive | Health and social professionals (n=7 groups) | Focus groups | Professionals’ perspectives on elder abuse | Three concepts emerged from the group discussion: neglect, abuse and maltreatment. Participants indicated the factors influencing the occurrence of negligence (socioeconomic context characteristics, the older person's social and personal characteristics, type of care, and the geographical context) and the causes of neglect, abuse and mistreatment (factors related to the professionals, the profession, and institutional factors). The groups analysed the relationship between risk group, profession and undesirable behaviour. The proposed solutions to prevent neglect and abuse were professionals’ solutions, solutions from the professions, and institutional solutions |
| Starr (2010) | Theoretical essay | |||||
| Strümpel and Hackl (2011) | Austria, Belgium, Bulgaria, Germany, Portugal and Slovenia | Descriptive | Professionals who working in community health and social services (n interviews=59) (n questionnaires=141) | Questionnaire and interview | Professionals’ perspectives on violence against older women | In all countries, staff of community health and care services reported that they had experienced different types of abuse against older women. Very little attention was paid to specific gender related issues. Barriers to detecting and reporting violence against older women were analysed. In the majority of countries, most organisations considered they were prepared to deal with abuse against older people and specifically older women to an average extent. It became evident through the “Breaking the Taboo 1” project that further awareness raising as well as longer training courses for staff members in health and care services for older people at home were necessary. A total of 14 trial workshops were carried out. Preliminary results of the trial workshops were: 1. Workshop participants perceived the topic as very relevant to their work, but it raised anxiety among some workshop members; 2. The most worthwhile learning experiences could be found through participants sharing their own experiences and “practical” case studies; 3. Organisational procedures dealing with abuse of older women had to be clarified before running the workshop; 4. To be able to plan the training course flexibly according to the target group and their roles, the time available and the size of the group attending the workshop; 5. The combination two areas of expertise (social services and violence against women) proved to be a very important factor in the success of the workshops; 6. Training volunteers as well as staff members; 7. Workshops with participants from different professional groups were seen as being very valuable and also rewarding |
| Sugita and Garrett (2012) | USA | Descriptive | Oral health care providers (n=103) | Questionnaire | Level of knowledge and the self-reported likelihood to report elder abuse | The analysis revealed that there was a significant increase in the number of respondents who felt that they had suspected elder abuse at least once in their career after the intervention. There was a significant improvement in self-reported levels of knowledge. Similarly, knowledge of the reporting process for elder abuse and neglect was improved after the intervention. The self-perceived likelihood to report an incidence of elder abuse showed increased numbers of respondents who would probably or definitely report. Increases were noted in comfort levels with recognizing signs and symptoms of elder abuse and neglect |
| Taylor et al. (2006) | USA | Descriptive | Primary care physicians (n=95) | Questionnaire | Knowledge deficits and perceived barriers to physician reporting | The majority of respondents recognised that physicians were not routinely screening for abuse, abuse was overlooked and that physicians were not familiar with signs of family violence. Regarding the impact of abuse, most participants expressed an understanding of the significance of the problem. With respect to an assessment of barriers to physician reporting, the lack of understanding about reporting procedures was deemed the most significant obstacle. There was strong agreement regarding the need for added education of clinicians. A majority of the responding physicians did not have a correct understanding of either prevalence or risk |
| Teresi et al. (2013) | USA | Randomised controlled trial | Residents and professionals of nursing home units (n=1405) | Questionnaire, interview and sheet report | Knowledge, recognition and reporting of resident-to-resident elder mistreatment (R-REM) | There was a significant gain in staff knowledge after training. Higher levels of recognition and documentation of R-REM were observed in the experimental as contrasted with the control group. The results showed that over time the experimental group reported significantly more R-REM events than did the control group |
| Yaffe et al. (2007) | Canada | Descriptive | Elderly individuals (n=858) | Questionnaire | Gender and suspicion of elder abuse | While the prevalence of elder abuse is estimated to range from 12.0% to 13.3%, the specific prevalence was found for females to be 13.6–15.2% and for males 9.1–9.7% |
| Yaffe et al. (2009) | Canada | Descriptive | Family physicians, nurses and social workers (n=31) | Focus groups | Professionals’ perspectives on elder abuse detection | Individuals from all three disciplines tended to focus on seniors who were 80 or older and often frail, frequently omitting consideration of younger, more active seniors. All three professions spoke of the desirability of minimising length of questions, but the reasons for this differed. The social workers’ approach appeared based on need to advocate for clients. Nurses’ viewpoints seemed influenced by utilitarian concerns for practicality and directness, desire to respect doctors’ time constraints, and discomfort that some physicians’ questioning might impose on nursing fields of interest. Physicians’ concerns tended to be holistic, tempered by practicality and time management issues. The social workers felt risk factors must be included in questionnaire items, however physicians did not. When participants were asked to rank the top five questions they considered best overall to meet the goals of an elder abuse suspicion index, the same five were chosen by all participants and all professions (though not necessarily in the same rank order) |
| Zanza et al. (2004) | Spain | Descriptive | Nurses (n=47) | Questionnaire | Use of physical restrictions | The use of physical restraints in geriatric centres appeared to be a fairly common practice, but it was not identified by professionals as being a possible abusive action. The infrastructure and resources of the institutions, dementia, and the unawareness of the problem among professionals were considered important risk factors |
As shown in Table 2, most of the reviewed articles consisted of primary investigations, two of which (Richardson, Kitchen, & Livingston, 2002; Teresi et al., 2013) used randomised trials to test the effects of training programmes. Two articles analysed systematic reviews (Cooper et al., 2009; Killick & Taylor, 2009). One (Cooper et al., 2009) incorporated a meta-analysis. The other documents were theoretical essays. Most of the investigations collected information through questionnaires. Interviews and focus groups were approaches that were also widely used. Several studies combined one or more of these techniques. Countries with a higher percentage of investigations were the United States, Australia, Israel, and the United Kingdom.
Characteristics of the studies reviewed (relative frequency).
| Type of study | |
| Theoretical essays | 15.79% |
| Systematic reviews | 3.51% |
| Primary investigations | 80.70% |
| Descriptive | 77.19% |
| Randomised controlled trial | 3.51% |
| Country | |
| United States of America | 16% |
| Australia/Israel/United Kingdom | 8.69% |
| Spain/Canada | 6.52% |
| Norway/Ireland | 4.35% |
| Czech Republic/Romania/Japan/South Korea/Turkey | 2.17% |
| Sweden and Japan/Norway and Australia | 2.17% |
| Austria, Belgium, Bulgaria, Germany, Portugal and Slovenia | 2.17% |
| Information gathering techniques | |
| Questionnaire | 60.87% |
| Interview | 13.04% |
| Focus groups | 8.69% |
| Other techniquesa | 6.52% |
| More than one techniqueb | 10.875 |
The main findings and conclusions of the analysed articles were classified around four themes: (1) the influence of definitions used by professionals for detecting and reporting elder abuse cases; (2) the ability of knowledge and attitudes of professionals to act as barriers or facilitators of detecting and reporting of abuse; (3) the influence of the knowledge and attitudes of professionals in strategies for action taken in response to suspected abuse; and (4) training as a means to improve the competence of professionals to detect and report elder abuse. The first thematic section focuses on the analysis of abuse definitions and the type of information on which professionals base their decisions. The second section presents the results of studies on factors that can facilitate or obstruct abuse detection and reporting, with knowledge and attitudes of health professionals being among the most studied factors. The third thematic section considers results of research on how knowledge and attitudes of professionals can influence the strategies of action to respond to suspected abuse. The fourth main theme focuses on the importance of training programmes to promote abuse detection and reporting to improve the knowledge and the attitudes of professionals towards abuse.
The influence of definitions used by professionals in the detection and reporting of casesAlthough clinicians often recognise elder abuse, a large percentage reported not having been in contact with a possible victim in the last 12 months (Rinker, 2009). A first aspect that reviewed publications highlight is the need to improve the definitions and classifications of abuse used by professionals (Pillemer et al., 2011). Our review included studies that evaluated the definitions and indicators used by adult protective services professionals (Daly & Jogerst, 2005), and studies concerning abuse detection by primary care professionals (Coma et al., 2007; Kennedy, 2005; Schmeidel, Daly, Rosenbaum, Schmuch, & Jogerst, 2012; Taylor, Bachuwa, Evans, & Jackson-Johnson, 2006). To promote the detection and reporting of possible cases of domestic abuse, practitioners must agree on and use operational definitions to guide their interpretations of available information. Furthermore, some studies (Dyer et al., 2005) showed that the type of professional activity or established relationship with the elder affected the access to information on which professionals could base their decisions. Thus, collaboration between professionals is also crucial to compile a more reliable and comprehensive list of possible indicators. Besides, differences were found between what seniors, family caregivers, and health professionals considered to be abuse (Hempton et al., 2010).
The definitions of institutional abuse and their types have also been studied. The use of physical restraints in geriatric centres appears to be a fairly common practice, according to one of the analysed studies (Zanza et al., 2004), but was not identified by professionals as being a possible abusive action, despite the frequency with which it occurs (Cooper, Dow, Hay, Livingston, & Livingston, 2013). The term “institutional abuse” can be used to refer to contexts involved in the abuse, and, in most cases, actions or omissions on the part of professionals or family members involved with the patient. Publications that considered abuse among residents in elder care institutions were less frequent (Ellis et al., 2014; Teresi et al., 2013). This type of abuse is often ignored by nurses, and can remain undetected to the extent that it can even be considered normal.
One of the studies reviewed (Bužgová & Ivanová, 2009) found that employees of residential homes and residents reported all types of abuse identified by WHO, except for sexual abuse, but more often they perceived violations of a patient's rights. Other studies analysed how professionals themselves defined abuse (Hirst, 2002; Sociedad Española de Geriatría y Gerontología, 2004). These studies showed that when social and health professionals were asked to define abuse, their views could be different from that reflected in definitions not generated by the professionals themselves. These results have important implications for the detection and reporting of abuse, and question the usefulness of the statutory definitions if they differ from those used by professionals. The results of other studies also suggest that definitions are influenced by cultural factors, and by job stressors that increase the probability that the abuse is rationalised (Cohen & Shinan-Altman, 2011; Shinan-Altman & Cohen, 2009).
The ability of knowledge and attitudes of professionals to act as barriers or facilitators of detection and reportingMost of the reviewed articles addressed the barriers and difficulties for professionals to detect and report abuse cases. The following barriers were found: lack of confidence in defining, identifying, and reporting abuse; reluctance to report abuse unless there is certainty that abuse had occurred; concern for the therapeutic relationship; potential consequences for the victim; the risk of a long judicial process; empathy with the abuser; a lack of screening procedures; not having clear definitions of abuse; shortages of available interventions for the abused and abusers; perceptions regarding the intent of the perpetrator; a lack of training; a lack of time; the victim's health; inability or unwillingness of victims to report their situation; absence of clear legislation; ignorance of laws concerning abuse; not knowing where or how to report; a lack of protocols; ethical dilemmas and paradoxes posed by reporting; the belief that abuse is a private family matter; and insecurity about whether the informant will be protected (All, 1994; Almogue et al., 2010; Bover, Moreno, Mota, & Taltavull, 2003; Cooper et al., 2009; Daly & Coffey, 2010; Daly, Schmeidel, & Jogerst, 2012; Joubert & Posenelli, 2009; Kennelly, Sweeney, & O’Neill, 2007; Kennedy, 2005; Killick & Taylor, 2009; Ko & Koh, 2012; Leddy, Farrow, & Schulkin, 2014; Liao, Jayawardena, Bufalini, & Wiglesworth, 2009; Mandiracioglu, Govsa, Celikli, & Yildirim, 2006; Rodriguez, Wallace, Woolf, & Mangione, 2006; Schmeidel et al., 2012; Strümpel & Hackl, 2011; Taylor et al., 2006). Two of the studies reviewed (Schmeidel et al., 2012; Yaffe et al., 2009) showed how perceptions of such barriers to detecting and reporting can vary depending on the professional profile and that health and social services professionals could have different attitudes, beliefs, values, and behaviours towards abuse. For example, compared to the more pragmatic approaches of doctors and nurses to abuse detection, the traditions of social work might encourage an approach based more on abuse defence.
The results regarding the role of professional experience seem to be a source of controversy. The results of some studies showed that health professionals recognised fewer abusive situations than did students in training (Dow et al., 2013); that lower degrees of professional experience predicted greater recognition of abuse (Caciula, Livingston, Caciula, & Cooper, 2010) and willingness to report abuse (Ko & Koh, 2012). These findings suggest that, over time, professionals can change their perceptions of what action strategies are acceptable in difficult situations in which there are few available alternatives and then adjust their views according to their level of experience. These results could also be due to the possibility that professionals with more years of work experience find reporting not to be useful. Alternatively, these results could indicate that better training of young professionals increased the likelihood of recognizing abuse. However, we also found other studies indicating that years of professional experience and knowledge regarding the assessment of abuse indicators were predictors of appropriate measures being taken to address cases of suspected abuse, since experience could influence the decision-making process (Meeks-Sjostrom, 2013).
There were other variables that increased the likelihood that abuse could be detected and reported: asking people about abuse; having a reporting protocol; working in a rural community; training to provide information about screening instruments, legislation, and available resources for elder abuse victims; the use of simple detection and reporting mechanisms; and the existence of a single entity that addresses reports of suspected abuse (Cooper et al., 2009; Leddy et al., 2014).
Along with research that focused on analysing the barriers to and facilitators of detecting and reporting abuse, other studies focused on factors that can influence whether professionals diagnose abuse and diagnostic decision making (Killick & Taylor, 2009; McCreadie et al., 2000; Yaffe, Weiss, Wolfson, & Lithwick, 2007). The data provided by McCreadie et al. (2000) supported the proposal that the knowledge of risk and, therefore, a greater understanding of the psychosocial circumstances of patients, facilitated the diagnosis of abuse among general practitioners. The systematic review conducted by Killick and Taylor (2009) aimed to identify research on how the decision making of professionals was involved in detecting elder abuse and to extract the key messages that guide their practices. As in other studies, the factors identified in this research were grouped into three categories: (1) case factors related to the client, the caregiver, or context; (2) professional factors related to the professionals or their roles; and (3) institutional factors such as services provided and relevant policies. The results indicated that factors relating to the case, particularly levels of risk and vulnerability, had a major impact on decisions about abuse detection and reporting. Patient age, gender, and health status were considered to be key indicators of vulnerability, while risk components were not clearly identified. Surprisingly, the type and severity of abuse, although important, were discussed in very few studies.
A barrier that seems particularly relevant for reporting institutional abuse was discussed in several of the studies reviewed (Ahern & McDonald, 2002; Davis & Konishi, 2007; Granville, 2001; Malmedal, Hammervold, & Britt-Inger, 2009) and concerns attitudes towards reporting on actions committed by other professionals. Although ethical codes for nurses establish their roles as defenders of patients and force nurses to act when the rights or safety of patients are at risk, reporting wrongdoing or incompetence can place nurses in direct conflict with their fellow professionals, which poses an ethical dilemma. In addition, fear of retaliation by colleagues or supervisors of nurses can present a major barrier to reporting (McCool, Jogerst, Daly, & Xu, 2009). However, the severity of the damage caused by abuse, the intent, and the belief that reporting is useful, all encourage the reporting of malpractice involving abuse. Also, the belief systems of professionals appear to influence behaviour.
The influence of knowledge and attitudes of professionals in strategies of action to respond to suspected abuseOne of the reviewed articles (Bomba, 2006) described the use of the Principles of Assessment and Management of Elder Abuse Tool. Such a tool can help maintain an index of suspicion for professionals, which is an essential attitude for detecting cases of suspected abuse. Four publications (Erlingsson, Ono, Sasaki, & Saveman, 2012; Sandmoe & Kirkevold, 2013; Sandmoe, Kirkevold, & Ballantyne, 2011; Strümpel & Hackl, 2011) considered the strategies of professionals who are faced with a possible case of abuse and found that knowledge and attitudes can affect the way in which they approach situations of suspected abuse.
Strümpel and Hackl (2011) outlined strategies that emerged from interviews with professionals from several European countries on how they addressed domestic violence against older women. Not all organisations have established standard operating procedures, leaving many frontline workers unsure about how to behave and what to do in situations in which abuse might be occurring. Regarding the education of staff and the organisational policy, most social service organisations did not feel adequately prepared.
Erlingsson et al. (2012) compared the actions proposed by Swedish and Japanese nurses regarding hypothetical cases of abuse. Community nurses in Sweden in these situations felt alone, with few resources and with an expectation of competition with other professionals. These nurses felt that their responsibility was to identify and describe the facts, and they expected the doctor to write a report. Meanwhile, Japanese nurses highlighted the need for a collaborative approach that involved the family, other professionals, and the community. They worked on multiple levels, including substantial social networking that fostered interactions not only with family members but also with community and government agencies. Moreover, the nurses felt that they should be present throughout the investigation process. Despite these cultural differences, this study identified common elements and emphasised the possibility of developing generalised instruments and interventions for detecting abuse.
Other research found many similarities in abuse-related difficulties reported by nurses in Australia and Norway and in the actions they performed in response to suspected abuse (Sandmoe et al., 2011). Their performance was influenced by several factors, but the most important were the gravity of the case and the cognitive ability of the victim. The main difficulties reported by nurses were that interventions should be individualised, and they had conflicting feelings about being both responsible for coordinating the activities of victim support and being involved in activities that the client could not fully understand, and the need to establish the boundary between respecting the will of the client and abandonment when a client rejected an intervention These results are consistent with another study analysing the perspectives of nursing team supervisors (Sandmoe & Kirkevold, 2013). In both studies, the need of frontline professionals for support and guidance from their superiors within the organisation was emphasised, as was the necessity for the organisation to receive the support of other organisations that specialise in intervention services programmes to protect against abuse.
Training as a means to improve the competence of professionals to detect and report elder abuseMost of the articles included in this review indicated the importance of training for professionals to promote the detection and reporting of elder abuse, and such training can influence the knowledge and attitudes of professionals. This training should be a part of the curriculum for undergraduate, graduate, and continuing education programmes (Starr, 2010). Some papers provided information to identify, prevent, and report abuse (Conry, 2009; Halphen, Varas, & Sadowsky, 2009). Others (Pillemer et al., 2011) emphasised the need to develop evidence-based training methods and to assess whether such training improves the effectiveness of professionals in identifying abuse, assisting victims, and improving case investigations. One of the systematic reviews included in this review (Cooper et al., 2009) concluded that no study has investigated how rates of detection and reporting could be increased, but did suggest a relationship between whether professionals received training and a higher likelihood of reporting suspected abuse. The analysis of the existing evidence (Bond, 2004; Cooper, Huzzey, & Livingston, 2012; Dow et al., 2013; Gironda et al., 2010; Shefet et al., 2007; Strümpel & Hackl, 2011; Sugita & Garrett, 2012) indicates some features that training programmes on detection and reporting of elder abuse should include: clear procedures regarding how to act and how to report abuse are in place before training courses are conducted; to include information about the ageing process to allow contextualisation of abuse cases; adaptation of content to existing regulations; training tailored to the characteristics and needs of the participants; the consideration of the importance of cultural aspects; flexible planning that suits the schedules of the participants and offers a number of appropriate training times to achieve the desired level of learning; the inclusion of different professional profiles, as well as volunteers, to enhance the training experience and provide a foundation for networking between individuals from different professions; the discussion of cases encountered in daily work to facilitate learning; to favour professionals asking seniors about abuse and addressing professionals’ concerns about the impact of reporting abuse on their therapeutic relationship with victims and the legal consequences for informants; and the use of standardised patients as the one methodology that can facilitate acquisition of relevant skills.
Three of the reviewed articles described programmes that focused on evaluating the effectiveness of training professionals to address institutional abuse. The most notable results include that professionals increased their knowledge but did not change their attitudes towards older people with dementia; the presence of a ceiling effect in the training, wherein professionals who began the training with a higher level of knowledge learned less (Richardson et al., 2002); the importance of adopting a people-centred perspective; and to conform interventions to the characteristics of each residential centre (Ellis et al., 2014; Teresi et al., 2013).
DiscussionThe results of the studies included in this review indicate the importance of the knowledge and attitudes of health workers as they relate to detection and reporting of abusive situations. The quality of abuse definitions, the accuracy of health professionals’ knowledge, and their expectations about the consequences of reporting or how they define their professional role can all influence the actions of health professionals and represent barriers or facilitators to detecting and reporting possible abuse cases. However, other factors can influence the decisions and actions taken by health professionals who encounter elder abuse. Thus, variables related to potential abuse victims and the organisational environment must be considered. Regarding organisational structures, studies included in this review emphasise the importance of having clear procedures to respond to suspected abuse and collaboration between professionals and between organisations or community services. The creation of action guidelines must allow an individualised approach for any case of suspected abuse (Sandmoe et al., 2011; Sandmoe & Kirkevold, 2013). Such guidance and direction should serve to enhance the activities of frontline professionals and organisations, as well as to encourage interdisciplinary assessment and design of responses to cases of abuse.
Most studies in this review point to training as a means to enhance health professionals’ knowledge of abuse detection and reporting rules and procedures. Although most studies found positive effects of training on the knowledge and attitudes of health professionals, there is still little available empirical evidence on the effectiveness of such training in terms of increasing the likelihood that cases will be detected and reported (Pillemer et al., 2011). Moreover, training should not only serve to increase the knowledge of professionals about abuse, but also change their attitudes towards the reporting of suspected cases. Even when they are provided with knowledge and appropriate procedures, professionals can choose not to report a case if they are unsure about whether reporting will benefit families or would cause professional harm. In the absence of such reassurance, only the most serious cases are likely to be reported based on the availability of definitive evidence, while suspected cases may go unreported. Therefore, the effectiveness of training to change attitudes to favour intervention in cases of abuse will be conditioned by other variables such as the type of resources available to assist families and to support health professionals who submit reports. The ethical dilemmas faced by professionals who decide to report cases of suspected domestic or institutional abuse are relevant, and experience can cause some professionals to think that such reporting is not worthwhile.
These concerns highlight the need for continued study of decision-making processes and strategies of professionals who encounter elder abuse. Most of the articles reviewed here collected results and conclusions from studies that explored the attitudes, beliefs, and knowledge of professionals and their relationships with the decisions and actions taken in response to suspected abuse. These investigations should be used as a foundation for pilot studies of theoretical models about the decision-making process involved in detection and reporting. Such models should also include the different variables that were previously shown to influence abuse detection and reporting.
There are two limitations to this review. The first relates to the fact that the studies analysed were found in the selected databases and met the inclusion and exclusion criteria employed. Therefore, studies in other databases, articles written in languages other than English and Spanish, and other types of publications (e.g., books and dissertations) may have been omitted from the analysis. The second limitation relates to the impossibility of accomplishing all the methodological recommendations proposed by some authors (Levac, Colquhoun, & O’Brien, 2010).
Conflict of interestThe authors have no conflict of interest to declare.