The present research is a continuation of another one previously developed about unsafe abortion, associated socio-demographic characteristics and morbidity, and goes further in its analysis of the social determinants of health that influence this occurrence, generating inequities in health. This study compared data of three groups of 51 women (total of 153) submitted to induced abortion, as per situation and site of the procedure: one with “unsafe abortion” (Slum), one with “legal and safe” induced abortion (Public hospital) and a third group with “illegal and safe” induced abortion (Private clinics with appropriate standard of care). Univariate and multiple analyses of multiple multinomial logistic regression analyses were performed for the three categories with Private as reference. In the final model, the variables that proved to have a statistically significant association with induced abortion (CI=95%; p<0.05) were: income, level of schooling, ethnicity/color and place of birth for Slum and, for the Hospital location, the variable ethnicity lost significance. Morbidity, resulting from the outcome, showed a highly significant discrepancy between the first sample (Slum), with 94.12% of women who reported post-abortion complications, and the other two samples (Hospital and Private) in which no case of complication was identified or reported. A critical analysis was also made on the influence of the social determinants of health implied in abortion in all samples, and on the degree of inequity generated in each one (intra-group) and among them. We aimed to better understand social determinants of health concepts in practice. Proposals of action/intervention related to the “entry points” and findings were also suggested.
A presente pesquisa dá continuidade a outra previamente desenvolvida sobre aborto inseguro, características sociodemográficas associadas e morbidade e aprofunda a análise sobre determinantes sociais da saúde que influenciam essa ocorrência e geram iniquidades em saúde. Este estudo comparou três grupos de 51 mulheres, 153 ao todo, com aborto provocado: um grupo com aborto provocado “inseguro” aborto inseguro (Favela), outro com aborto provocado “legal e seguro” (Hospital Público) e um terceiro com aborto provocado “ilegal e seguro” feito em clínicas particulares (Particular). Na análise dos dados, foram efetuadas análises univariadas e múltipla de regressão logística multinomial para as três categorias de aborto provocado, relacionadas por local, tendo como referência o local Particular. No modelo final as variáveis que mostraram associação estatisticamente significativa (p<0,05; IC: 95%) com aborto provocado foram: renda, escolaridade, etnia/cor e origem para o local Favela. Para o local Hospital a variável etnia perdeu a significância. A morbidade resultante dos resultados mostrou uma discrepância altamente significativa entre a primeira amostra (Favela), com 94,12% das mulheres que declararam complicações pós-aborto e as outras duas amostras (Hospital e Particular), nas quais nenhum caso de complicações foi referido ou identificado. Foi efetuada, então, análise crítica sobre a influência dos determinantes sociais da saúde implicados na ocorrência do aborto provocado nas três amostras e o grau de iniquidades por eles gerado em cada uma delas e entre elas. Com isso, pretendemos entender como usar melhor os conceitos de determinantes sociais da saúde na prática. Foram sugeridas também propostas de ação/intervenção relacionadas aos “pontos de entrada” pertinentes aos achados.
The present research is a continuation of another one previously developed about unsafe abortion, associated socio-demographic characteristics (SDC) and morbidity, and goes further in its analysis of the social determinants of health (SDH) that influence this occurrence, generating inequities in health.1
Twenty years after the International Conference on Population and Development (ICPD), Cairo, 1994, the situation of unsafe abortion, considered then as a serious Public Health problem, continues unchanged in Brazil.2
Unsafe abortion may be defined as the “procedure for terminating an unintended pregnancy either by people lacking the necessary professional skills or in an environment lacking the minimal medical standards, or both”.3 Globally, unsafe abortion causes about 70 thousand deaths a year (13% of the total number of maternal deaths). The World Health Organization (WHO) calculates that each year, and between 19 and 22 million abortions occur in the world under conditions that are inadequate or of risk.
Almost all the abortions under conditions of risk, or unsafe, occur in developing countries or in poor countries where abortions are limited by law. In 2003, for example, 97% of all unsafe abortions occurred in developing countries, such as Brazil,4 and unsafe abortion was the primary cause of maternal mortality in Latin America and the Caribbean,5 a region with one of the highest recorded rates of clandestine and unsafe abortions, that is, 31/1000 women.3
Finally, unsafe abortion is a serious Public Health problem recognized by the international scientific community in conferences promoted by the United Nations during the 1990s.6–8 In countries where abortion is clandestine and unsafe, its consequences for the health of women are harmful, especially for women who are young, poor, and with a low schooling level. Hence, its impact on local public health services must be taken into account.2,4,9–11
The Social Determinants of Health (SDH) are understood as the social, economic, cultural, ethnic/racial, psychological, behavioral, and other factors that influence the occurrence of health problems and its risk factors on the population. Despite already having reached a certain consensus on the importance of SDH on the health situation, this consensus was built throughout history centered primarily on the conflict between the influences of the biological and the social factors on the health-disease process.12
After the historic Conference in Alma-Ata, in 1978, and its proposal centered on the strategy of primary care in order to provide “health for all in the year 2000”, a year when the reinforcing debate on Millennium Development Goals occurred, accompanying worldwide and growing interest, on the theme of social determinants and inequities in health, the WHO decided to “take upon itself” this issue in 2005, creating the Commission on Social Determinants of Health (CSDH). One year later, in 2006, by Presidential Decree in Brazil, the National Commission on Social Determinants of Health (CNDSS, acronym in Portuguese) was created.13
In 2011, Fusco noted that the occurrence of unsafe abortion and the main socio-demographic characteristics associated with them are influenced by structural and intermediate SDH, generating health inequities of various proportions among the women with history of abortion.2 Additionally, in the population studied (1), the morbidity rate proved much higher than that reported in higher income populations or those with access to safe abortions.14 The vast majority of women who provoked unsafe abortions reported complications related to the abortion, especially intense hemorrhage, with a confirmed high number of admissions to public hospitals of the region. Since mortality due to abortion is difficult to measure, morbidity, the predisposing condition, constitutes the major representative characteristic of the inequities in healthcare, in its values.1
The objective of this new research project was to compare the data obtained in this population studied (1) with data from new populations of women submitted to (2) legal and safe abortion performed in a public Hospital and resulting from sexual violence, and (3) illegal and unsafe abortion performed in high-standard private clinics – regarding the conditions of the occurrence of abortion, associated socio-demographic characteristics, outcome, and morbidity in these populations. The comparisons were made in light of the SDH involved and inequities due to the great influence generated among the women of these populations. Another objective was to suggest healthcare actions and/or interventions aiming to reduce the degree of inequity.
MethodIn the research on unsafe abortion,2,9 Fusco began with a cross-sectional study in which all women aged 15–54 years (Census) residing in a slum area in the Northern zone of Sao Paulo City (Favela Inajar de Souza) were interviewed in the second semester of 2005 and the first semester of 2006. Out of 382 women living in this area and in this age group, 375 were interviewed and only 7 (1.8%) refused to participate in the study.
Data collection was carried out by means of a direct structured interview by trained female interviewers in the homes of the interviewees. The data collection tool has three elements grouped together into a single one: Family Composition (with household monthly per capita income); Structured and pre-coded questionnaire to collect socio-demographic data; and gestational history (with an appendix on complications relative to the abortion and hospitalizations).
The interviews were performed by three monitors of the community and three undergraduate Human Sciences students, who were trained in workshops, and carried out the interviews by means of home visits to the women of the population at a time appropriate for the interview. This procedure was tested previously in a pilot group and under supervision of a field coordinator during the entire data collection process. The women were encouraged to participate in the research and absolute confidentiality was assured as to the information collected, including the fact that no identification was required from those who answered the questionnaire.
For the statistical analysis, the dependent variable, Abortion, was divided into 3 categories: NA/LB (no abortion or just liveborn), SA (spontaneous abortion/miscarriage), and IA (induced abortion).
The independent variables used in this project were age at first sexual intercourse; marital status at the time of the event; ethnicity/skin color; origin or migration (State of Sao Paulo or from other states); religion; paid job; per capita income; family income; level of schooling; use of contraceptives at the time of the gestation of the event. Also investigated were post-abortion complications (morbidity) and hospitalizations.
Initially, the prevalence of abortion – induced and spontaneous – was calculated among women aged 15–54 years, who lived in the community. For data analysis, chi-squared or Fisher's association tests were used, besides Kruskal–Wallis test (for per capita income) and univariate and multiple multinomial logistic regression analyses, using as reference category the NA/LB variable. The variables that showed associations with p<0.20 were selected to be used in an initial Multiple Multinomial Logistic Regression (MMLR) model using the backward stepwise method for identification of the variables that remained in the final model. In all analyses of the final models the association was considered statistically significant when p<0.05. The statistical analysis of the data was performed by means of the software SPSS 16.0, for Windows.2
This research, in its two phases, was approved by the Ethics and Research Committee of the Universidade Federal de São Paulo – UNIFESP (CEP number 1300/06 and CEP number 0990/10). Signing of the Informed Consent Form (ICF) was waived by the nature of the theme covered.
As to the data collected from the sample at the Hospital Pérola Byington (legal and safe abortion), the database available used had 300 women seen from 2009 to 2012, predominantly from the Public Healthcare System (SUS, acronym in Portuguese). It was very difficult to identify the medical charts before this period. Therefore, one case in every five was drawn of the sequential medical charts from this time interval, until completing a sample of 51 cases. The independent variables compatible with the SDC of the first study were: age, marital status, skin color, level of schooling, family income in minimum wages (MW), place of birth, origin, occupation, age at first sexual intercourse, number of children, religion, and morbidity. These data were available in the files of the hospital and were collected by the professionals of the Sexual Violence and Legal Abortion Service.
The abortion cases of the private clinic selected (safe clandestine induced abortion) were among all the cases of general gynecology. There is no archive or database with specific data on abortion at these clinics. Therefore, the same period of 2009–2012 was used. The cases included for the project were the result of a drawing, based on alternated consultation of the medical charts following their numerical sequence. The medical charts without information on abortion were eliminated, following along with the alternated sequence until obtaining 51 cases. The independent variables chosen were the same as those of the previous sample: age, marital status, skin color, level of schooling, family income in minimum wages, place of birth, origin, occupation, age at first sexual intercourse, number of children, religion, and morbidity.
In the statistical analysis of data of the three pooled samples, the variable Location was used, divided into three categories: Slum (S), Hospital (H), and Private (P). Association measurements and descriptive analyses were done, including frequencies, cross-tabulations, chi-squared test, etc. Next, univariate and multiple multinomial logistic regression analyses were made, as in the previous study.
After the statistical evaluation, a critical analysis was made as to the influence of the SDH implied in the occurrence of abortion and its SDC in all three samples, along with the degree of inequity they generated in each one (intra-group) and among them (inter-group), based on the theoretical body prepared by the CSDH.15
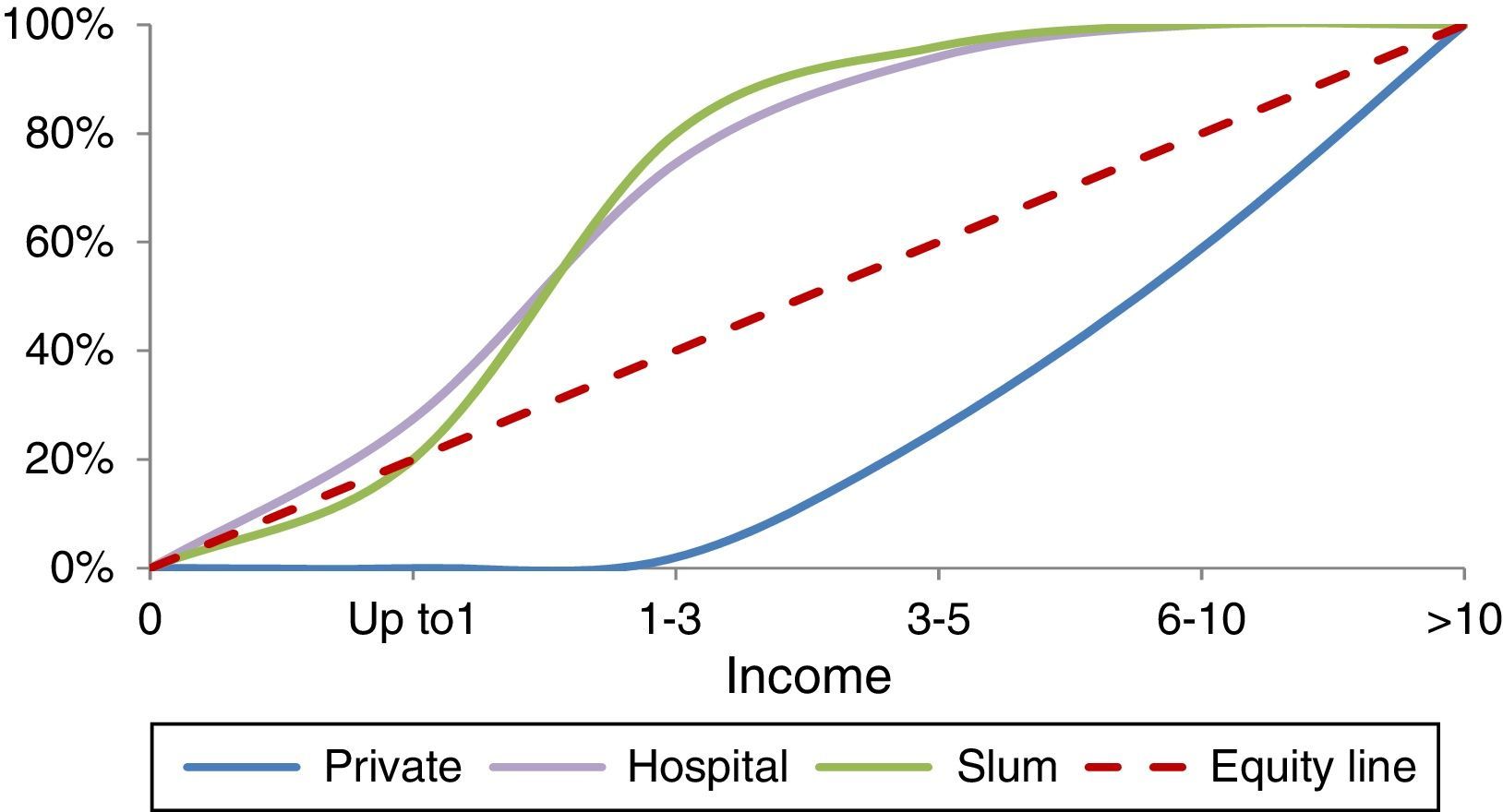
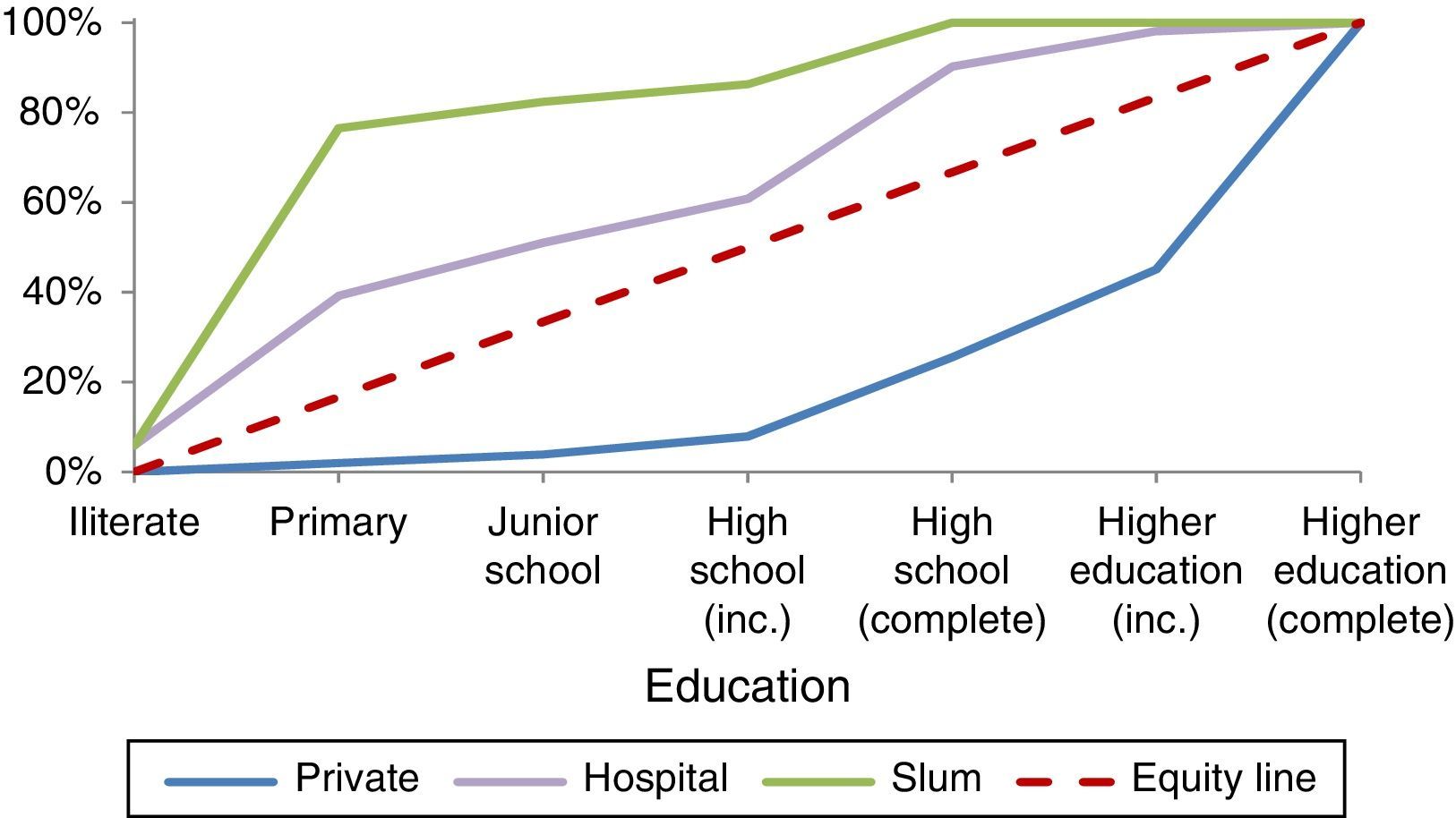
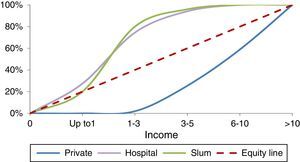
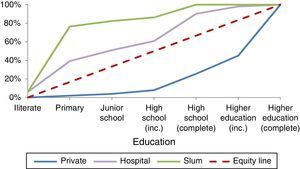
Also prepared were “concentration curves” (quantitative techniques for health equity analysis) for two of the usable variables (income and level of schooling) that remained in the final MMLR model.
(Ethics and Research Committee of the Universidade Federal de São Paulo – UNIFESP, CEP number 250177/13)
ResultsEach sample of 51 women resulting from the three populations analyzed (total of 153 women) referred to a type of induced abortion and a location in Sao Paulo City. The induced abortions (IA) from each sample can be classified as: (1) Slum – unsafe abortions (UA); (2) Public hospital – legal and safe induced abortions; (3) Private – illegal and safe abortions.
Primary descriptive measuresMorbidity, resulting from the outcome, showed a highly significant discrepancy between the first sample (Slum), with 94.12% of women who reported post-abortion complications, and the other two samples (Hospital and Private) in which no case of complication was identified or reported.
The mean age among the three groups showed a statistically significant difference, p<0.001, due to the Private group: Slum=21.6 (minimum=13 years – maximum=37); Hospital=22.3 (minimum=12 years – maximum=38); and Private=28.8 (minimum=16 years – maximum=45).
As to Income, the three groups also proved to be unequal from the statistical point of view (p<0.001), where in the Slum group 80.4% of the women declared a family income of up to 3MW (monthly minimum wages); in the Hospital group, 74.5% had this monthly household total; and in the Private group, only 2%, that is, one woman reported this value as the monthly family income, whereas 41.2% of women in this group, at the other extreme, declared a monthly family income greater than 10MW.
As to Paid Job, 51% of women from the Slum declared paid job; from the Hospital group, 61%, and from the Private group, 98%, with a statistically significant association (p<0.001). As to Level of Schooling, once again there is a noteworthy significant difference (p<0.001) among the groups: Slum – 82% with a level of schooling up to Junior School, with 5.9% illiterate, 70.6% with incomplete or complete Primary School (less than 5 years of studies), 5.9% with complete Junior School, and 17.6% with incomplete or complete High School; Hospital – 5.9% illiterate, 33.3% up to incomplete Junior School, 11.8% with complete Junior School, 9.8% with incomplete High School, 29.4% with complete High School, 7.8% with incomplete higher education, and 2% with complete higher education – in this group, some of the girls are still young and students; and Private – 4% up to complete Junior School and 96% distributed into 21.5% with incomplete or complete High School and 74.5% with Higher Education whether incomplete, ongoing, or complete.
Ethnicity/Skin Color had the following distribution (with p<0.001): Slum – 76.5% non-white (black or brown) and 23.5% white; Hospital – 47.1% non-white and 52.9% white; Private – 9.8% non-white and 90.2% white.
As to Place of Birth or Origin (where the person was born), approximately 60% of women from the Slum come from other states different from Sao Paulo; in the Hospital group, 55% were born out of Sao Paulo State, and 55.8% live in other cities or in peripheral areas of Sao Paulo City; in the Private group, 94.2% of women live in Sao Paulo City and three women in other large cities.
For Age at first sexual intercourse, the descriptive analysis showed: Slum – 76.5% of women had their first sexual intercourse under the age of 16 years; Hospital – 66.7% had their first sexual relation under 16 years of age, and 11 girls (21.6%) had not yet initiated their sexual life at the time of the rape, and Private – 41.2% of women of this group reported having initiated their sexual life at an age under 16 years and 58.8% over 16 years (mean=17.6 years). The association shows a statistically significant difference with p=0.001.
Regarding the number of children born alive, 78.5% of the women residing in the Slum reported having more than two children; in the Hospital group, 21.6% already had two or more children at the time of the event analyzed (IA), and in the Private category, only 11.8% of them declared having two or more children (p<0.001).
As to Religion, more than 50% of the women from the three groups declared they were Catholic. As regards to Marital Status, 55% of women interviewed from the Slum declared being single and/or alone; of the Hospital group, 88.2% of patients reported being single at the time of the event, and 72.5% of the Private group also declared being single as their marital status. The association proved statistically significant with p=0.001.
Multiple multinomial logistic regressionThe variables representative of the socio-demographic characteristics (SDC), that showed association with p<0.20 were selected to be entered into an initial model of Multiple Multinomial Logistic Regression (MMLR) using the backward stepwise method.
In the univariate analyses for two populations (Slum and Hospital) the variables income, level of schooling, skin color, and place of birth remained significant, having as reference the Private category.
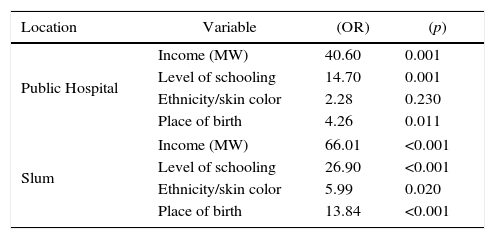
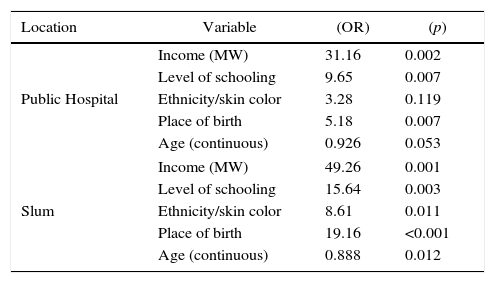
In the multiple analysis, in the final model, the variables that proved to have a statistically significant association were the same for Slum location and, for the Hospital location, the variable skin color lost significance (Table 1).
Multiple analysis of variables (socio-demographic characteristics) associated to induced abortion for the groups: Hospital and Slum.
| Location | Variable | (OR) | (p) |
|---|---|---|---|
| Public Hospital | Income (MW) | 40.60 | 0.001 |
| Level of schooling | 14.70 | 0.001 | |
| Ethnicity/skin color | 2.28 | 0.230 | |
| Place of birth | 4.26 | 0.011 | |
| Slum | Income (MW) | 66.01 | <0.001 |
| Level of schooling | 26.90 | <0.001 | |
| Ethnicity/skin color | 5.99 | 0.020 | |
| Place of birth | 13.84 | <0.001 | |
MW, minimum wage.
Reference category: Private.
These factors had the following distribution and results in the final model adjusted by age (Table 2):
Multiple analysis of variables (socio-demographic characteristics) associated to induced abortion for the groups: Hospital and Slum (adjusted by age).
| Location | Variable | (OR) | (p) |
|---|---|---|---|
| Public Hospital | Income (MW) | 31.16 | 0.002 |
| Level of schooling | 9.65 | 0.007 | |
| Ethnicity/skin color | 3.28 | 0.119 | |
| Place of birth | 5.18 | 0.007 | |
| Age (continuous) | 0.926 | 0.053 | |
| Slum | Income (MW) | 49.26 | 0.001 |
| Level of schooling | 15.64 | 0.003 | |
| Ethnicity/skin color | 8.61 | 0.011 | |
| Place of birth | 19.16 | <0.001 | |
| Age (continuous) | 0.888 | 0.012 | |
MW, minimum wage.
Reference: Private.
The MMLR shows that women living in Slum with a monthly family income of less than 2MW had a 49.2-fold higher chance of causing an unsafe abortion than the women with an income greater than 2MW, using the Private category as reference. On the other hand, in the Hospital group, the women with an income lower than 2MW have a 31.1-fold higher chance than do those with incomes superior to 2MW of undergoing a legal and safe induced abortion after sexual violence.
Likewise, the women with a low level of schooling in the Slum have a 15.6-fold higher chance of inducing an unsafe abortion and in the Hospital group, a 9.6-fold higher chance of provoking a legal and safe abortion after sexual violence than do those of a higher level of schooling (more than complete Junior School).
As to place of birth (if in Sao Paulo or out of Sao Paulo), in the Slum the women who were not from Sao Paulo City had a chance 19.1 greater of inducing an unsafe abortion, and, in the Hospital group, a chance 5.2 times greater of undergoing a legal and safe abortion after sexual violence.
Relative to skin color, in the Slum the women of ethnicity with black and brown skin color have a probability 8.61 times greater of inducing an unsafe abortion when compared to those of white skin. In the Hospital group, despite the fact that in the univariate analysis the OR for skin color was significant, this variable lost significance due to the other variables in the final model.
For the analysis of the MMLR models, a second random sample was collected from the Hospital group with 51 additional cases and the model for age was adjusted in order to increase accuracy. The OR related to the independent variables refer to the outcomes, always using the Private category as reference, and each variable should be seen considering the group of variables that remained in the model.
DiscussionThe structural determinants of health of a population, shaped by the macrosocial determinants, such as social, political, cultural, and economic contexts, are responsible for the unequal distribution of income, differences in education/level of schooling, gender and ethnicity inequalities, among others, resulting in the process of social stratification that this population is subjected to. The intermediate determinants (housing, working conditions, behavioral factors, etc.) in line with this process determine the differences in exposure and vulnerability of this population to a disease or condition.16
The theoretical body of the studies on SDH and on the inequities generated by them facilitates the researchers’ understanding of the results of investigations that involve populations, or population subgroups (even with the impossibility of “study designs” closer to the ideal), as long as the social context of the studied population is known.13,15
Based on the analysis of the social context of the three study populations,17 income is the main structural determinant of the differences among them, and can originate unequal health outcomes and inequities (Fig. 1).
The first two population samples, Slum and Hospital (S and H, respectively), show a certain similarity in income, which on the other hand is exuberantly unequal relative to the third sample, Private (P). This is reflected in the other results. The inequities among the populations generated by the influence of this determinant initially become distinct by their own outcomes and corresponding morbidity when comparing the population with lowest income (S), with only unsafe abortions and an extremely high morbidity rate, and the highest income population of the three (P), which only had safe abortions and no complications or morbidity.
Nevertheless, the second population (H) with income similar to that of S also shows only safe abortions. Considering the process of social stratification, the tendency would be to attribute only to the monthly family income, which represents social inequality among the groups, the inequities in health regarding the outcomes among the populations studied. The relation between poverty and precarious reproductive health, with a high percentage of unintended pregnancies, is already well established. Also, unwanted gestations are positively correlated with risks of unsafe abortions.14 However, in the causal chain of unsafe abortion and its associated morbidity, there is another determinant – the laws of the country that are restrictive to abortion, linked to macrosocial determinants, such as the political system responsible for the laws, which, in turn, is influenced by the dominant culture and religion.
Despite sexual violence, in cases of rape followed by gestation, suffered by the patients of the public hospital, the same law (article 128 of the Criminal Code) that criminalizes abortion allows it in this situation. “Every scientific evidence available indicates sexual violence as a universal phenomenon not associated with social or economic development of a country or a given population, although it is acknowledged that vulnerability may vary for certain specific groups… The difference in Brazil is in the way in which this outcome (abortion) is treated. Socioeconomic classes with greater resources generally do not depend on the Public Healthcare System – SUS – and seek the clandestine system for termination of pregnancy, since they have the financial resources to access a safe form of pregnancy interruption”.18
We also point out that the influence of another structural SDH, i.e., gender inequality, an influence in the three populations studied with different intensities, affording unintended gestations and the option for IA, is stronger in the two populations of lowest income. Remember that “gender violence is a relation of forces that transforms the differences between sexes into inequalities. Men and women end up classified by gender and separated into two categories, one dominant and the other dominated”.19 Note: The debate about gender inequalities and IA will be the subject for another article, since it calls for a lengthy discussion.
The level of schooling, as a structural SDH, in a certain way is representative of income when it cannot be measured – therein lies its importance.2 The countries with the highest rates of income inequalities also have the worst performance at schooling level, which is most marked in the lowest social strata.20 The level of schooling, such as SDC, proved an influential factor in the outcomes of the two low income populations, generating intra- and – especially – inter-group inequities, with the worst outcome – unsafe abortion with associated morbidity – among the women of the first group (S).
The Hospital sample presented with a level of schooling above that of the first sample (Fig. 2), which may have also influenced its representatives to seek help from the Law and physicians. Conversely, the analysis of the level of schooling of the reference sample (P) indicates a very high level of schooling pointing toward voluntary abortion by choice of the patient with a greater sense of autonomy.
Additionally, one should not forget that the use of contraceptives is intimately linked to level of awareness and that vulnerability to unintended gestations is strongly influenced by access and use, or non-use, of effective contraception (intermediate SDH), besides exposure to undesired sex and sexual violence, factors correlated to the level of schooling.14
The place of birth or origin in these samples also speaks of internal migration, which is another structural SDH involved in the social stratification process. The majority of women belonging to the first two samples (S and H) went through this process, which along with its implications may have influenced the outcomes. As to unsafe abortion, this has already been previously verified. “In the slum studied, a large part of the adult population comes from other states, especially the Northeastern region of Brazil, seeking means of survival or better life conditions”… “We note that among the women with a prior gestation, about 60% of those that induced unsafe abortions are not from Sao Paulo State”.2,9 Over the last decade, researchers have directed more attention toward the determinants of poor health within the context of migration.14 There are still few data related to the issue, although internal migration, as well as international migration, continues to grow.
As to the women seen at the hospital (H), most live in the outskirts of the city or even in other cities. The place of residence and the houses are intermediate determinants that influence – along with the process of social stratification – the outcomes and inequities in health. Moreover, as intermediate determinants they are responsible for greater exposure and vulnerability. For example, lack of safety in certain locations increases exposure to non-domestic rape and women who reside there are more vulnerable to this type of occurrence.
Ethnicity/skin color, another structural determinant of health, is interwoven with other structural SDH (e.g., income, education, gender, and migration) as well as with intermediate determinants defined by the socioeconomic position (e.g., place of residence, type of housing, working conditions, habits, etc.), generating exposures harmful to health and increasing vulnerability of susceptible populations. The structural and intermediate determinants mutually influence each other in a perpetuum mobile, promoting iniquities in health, which in the case of the black-skinned population, result in all possible interactions of these determinants.16
Thus, “black (Afro-descendant) women in Brazil have less access to education, worse life and housing conditions, less access to contraceptive methods, and present with greater chances of getting pregnant, even when this is not what they desire”.21
Among the women from the first sample (S) that induced an unsafe abortion, there is a greater proportion of women of black-skinned ethnicity, with low incomes, less than four years of study, and single, which in and of itself, when compared to the white women, demonstrates the inequities in health.2 In the hospital (H) sample, about half of the patients considered themselves to be of black-skinned ethnicity.
The model proposed by the WHO International Commission on SDH, and utilized by Blas in his “case studies”, identified four relevant levels of action or intervention: social stratification, exposure, vulnerability, and different consequences.22 The frame of reference of the Commission adopts these four “entry points” (or access points) and adds a fifth regarding access to the healthcare services.15
Starting with the intermediate determinants that cause greater exposure to unsafe abortions (S) and, in the case of SUS patients (H), to sexual violence followed by gestation and abortion, the action plans focused on these two apparently similar social context populations would be different. Populations residing in small slums, such as that of sample S, classified as belonging to Group 6, that is, of very high social vulnerability according to the Social Vulnerability Index of the State of Sao Paulo – IPVS,23 deserve field interventions that go from information, such as lectures, workshops, and distribution of educational materials, to a program of continuing education seeking to prevent the occurrence (incidence and prevalence) of unsafe abortion and associated morbidity.
The SDH, contraception, and reproductive planning are themes that can be covered in constructivist workshops, with community participation, both as a first step to choose monitors and multiplying agents, and later, to convey the content learned and to discuss the topics with the rest of the residents, making good use of the “capital stock” of this community. With this type of intervention, the exposure and vulnerability of the population can be decreased and consequently, the inequities in health and the different consequences. An intersectoral collaborative action may also be attempted with public health policies allied with third-sector actions, such as NGOs,22 aiming at a more efficient reproductive and family planning.
As to populations that are vulnerable and have greater exposure to sexual violence out of the domestic realm (rape in the streets), besides preexisting legal and medical support in case of gestations resulting from the violence, with safe abortion allowed by law and adequate treatment offered by the hospitals that have services to treat cases of sexual violence, with multidisciplinary teams, and the consequent reduction of inequities – a model of “effective intervention” – should incite the improvement of public safety in locations most likely to be exposed to this crime, with community participation of the populations most vulnerable to it.
These are merely a few ideas (or examples) among many possible actions related to the points of entry conceived by the WHO in approaching SDH, primarily the intermediate determinants.
Due to the difficulty of rapid action on the macrosocial determinants and on the process of social stratification originated by the structural determinants, such as unequal income, level of schooling, gender, migration, and ethnicity, which have an influence in and of themselves and in their interrelations on the occurrence of unsafe and/or clandestine induced abortion, and even on safe abortions and associated SDC, generating inequities, it is up to us to propose actions on the prevention of unsafe abortion and its associated morbidity, since safe abortions are practically devoid of complications. Using as initial reference the differences in outcomes related to morbidity (predisposing condition to mortality), the issue that most draws our attention is what we see repeated as to the current laws that demands changes in the direction of legalization of abortion.
Regardless of theoretical considerations with respect to this serious public health problem, already discussed at length, we think that at least abortion, the process of interruption of an ongoing gestation, should be in the hands of hospitals and physicians with their teams. Enlightened by the concept of sexual violence attributed to rape, the concept of social violence should be attributed to unsafe abortion and its consequences in terms of morbidity and mortality, considering that differences between groups and between populations represent avoidable, unfair and unnecessary inequalities.24
The attention given to cases of sexual violence demonstrates the possibility of reducing maternal morbidity and mortality due to abortion to zero or close to this. Access to healthcare services beyond prevention (but including it) in cases of abortion, with the steps already used at the services that treat sexual violence, warm welcoming environment, medical care, and posterior follow-up of the patient and prevention of resorting to abortion as reproductive planning, may perfectly be transformed into a program for short-term harm reduction, carried out by healthcare teams including those of SUS, even before legalization of abortion.
In conclusion, three different samples were investigated with 51 women each, all with induced abortions, named by the location where the abortion took place (S, H, and P), and that differed as to the subtype and quality of the outcomes. The Private group was the most homogeneous of the groups and served as reference for the statistical analysis of the other two, as it was the group with the greatest income and highest level of schooling, with voluntary abortion, although illegal, and safe without complications, revealing an even greater capacity for choice and autonomy of women. Unsafe abortion followed by morbidity only appears in the S group. Once again the need to legalize abortion is reassured, indicating the relevance of the topic as an ethical public health imperative in Brazil.
The SDH that influence in this occurrence (IA) and in the SDC associated with the abortion generated inequities within the groups (S and H) as well as among the three groups. The primary SDH involved were represented in the final model by the variables income, level of schooling, ethnicity/skin color, and place of birth/origin. The laws and the current political system with influence of other macrosocial factors, such as culture (including religion), provide for induced abortion in cases of sexual violence, allowing the H group to have legal and medical support, which lead to safe abortion with posterior follow-up of the patient. This group of actions can serve as a model for a harm reduction program while the law in reference to abortion is not totally modified. Local actions geared toward the entry points linked to the SDH responsible for greater exposure and greater vulnerability to abortion, in more susceptible populations, such as those with low income, can also be planned and developed for the reduction of inequities in health.
FundingTwenty-four months FAPESP scholarship granted to the author for the development of the project.
Conflicts of interestThe authors declare no conflicts of interest.
Study conducted at the Department of Preventive Medicine, Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.