Chorioangiomas are the most common benign placental tumors, with an estimated prevalence of 1%. Whilst small chorioangiomas usually remain asymptomatic and are of no clinical significance, larger tumors (>4cm) can be associated with a variety of complications, ranging from fetal anemia to in-utero demise in up to 40% of cases. Despite size being a major determinant for the risk of complications, the degree of the chorioangioma's vascularity also seems to play a role. In fact, in selected cases, occluding the tumors vessels (e.g. with alcoholic instillation) appears to improve the prognosis due to the subsequent tumor ischemia. We present the case of a 40-year-old woman who at 29 weeks was found to have a large placental hypervascular mass (93mm×66mm) and polyhydramnios, with an elevated peak systolic volume in the middle cerebral artery. She was given corticosteroids for fetal lung maturation, and throughout her admission both the volume of amniotic fluid stabilized and the peak systolic volume in the middle cerebral artery normalized, with changing of the ultrasonographic characteristics of the chorioangioma, with apparent progressive necrosis. At 34 weeks, a large subchorionic hematoma was found and, due to the risk of impending placental abruption, we opted to deliver by cesarean section, with a favorable outcome.
Corioangiomas são os tumores placentários benignos mais comuns, com uma prevalência estimada de 1%. Embora pequenos corioangiomas geralmente permaneçam assintomáticos e não tenham significância clínica, tumores maiores (> 4cm) podem estar associados a diversas complicações, que variam de anemia fetal até a morte intraútero em até 40% dos casos. Ainda que o tamanho do tumor seja um determinante principal para o risco de complicações, o grau da vascularidade do corioangioma também parece desempenhar um papel importante. De fato, em casos selecionados, a oclusão dos vasos tumorais (por exemplo, através de instilação de álcool) parece melhorar o prognóstico devido à subsequente isquemia tumoral. Apresentamos o caso de uma mulher de 40 anos a qual, com 29 semanas de gestação, apresentava grande massa hipervascular placentária (93×66mm) e poli-hidrâmnio, com elevação do peak systolic volume in the middle cerebral artery. Ela recebeu corticosteroides para a estimulação da maturação pulmonar fetal e durante a sua internação o volume de líquido amniótico foi estabilizado e o peak systolic volume in the middle cerebral artery normalizado, com mudança nas características ultrassonográficas do corioangioma, com necrose progressiva aparente. Com 34 semanas de gestação, observou-se a presença de hematoma subcoriônico de grande porte e, devido ao risco de descolamento prematuro da placenta, optou-se por parto cesariano, com desfecho favorável.
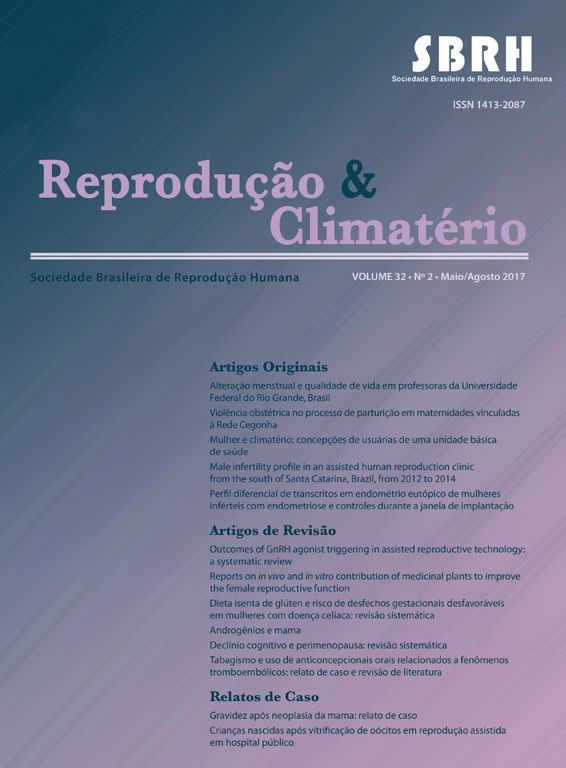
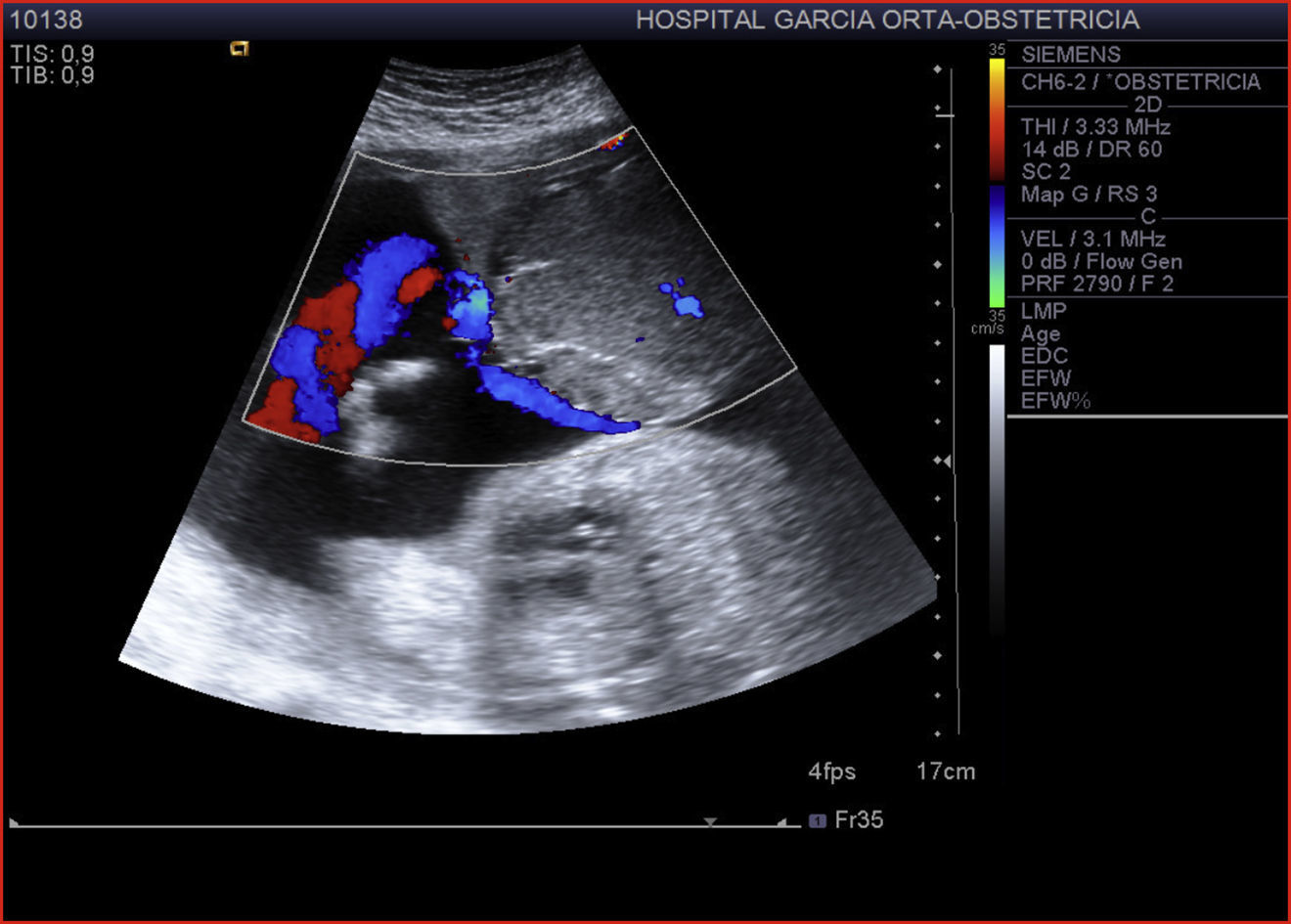
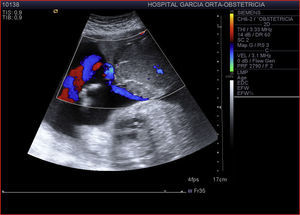
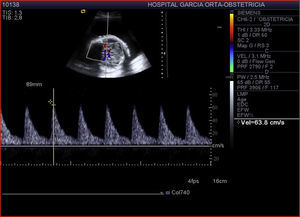
A 40-year-old woman, gravida 3 para 2, was referred to our tertiary-care hospital due to a history of primary hypertension. She was submitted to amniocentesis due to maternal age, with a normal 46,XX karyotype reported. Ultrasounds at 12 and 20 weeks demonstrated normal fetal biometry, with no abnormalities detected. Her pregnancy was uneventful up until 29 weeks, when a routine ultrasound revealed polyhydramnios (amniotic fluid index of 34cm) and a large well-circumscribed hypervascular placental mass (93mm×66mm), highly suggestive of chorioangioma with an adjacent cord insertion (Fig. 1). Fetal growth was normal, as was fetal anatomy. Pulsed Doppler study of the peak systolic volume (PSV) of the middle cerebral artery (MCA) suggested fetal anemia (1.67 MoM) (Fig. 2).
The patient was admitted to the high-risk obstetric unit, undergoing fetal lung maturation with corticosteroids, and being submitted to daily ultrasound and cardiotocographic assessments. Throughout her admission we observed normalization of the peak systolic volume in the middle cerebral artery (PSV-ACM) values, stabilization of the amniotic fluid volume and no signs of fetal hemodynamic instability. This, together with the fact that the tumor lied in close proximity to the umbilical cord insertion, made us decide not to intervene with in-utero therapy.
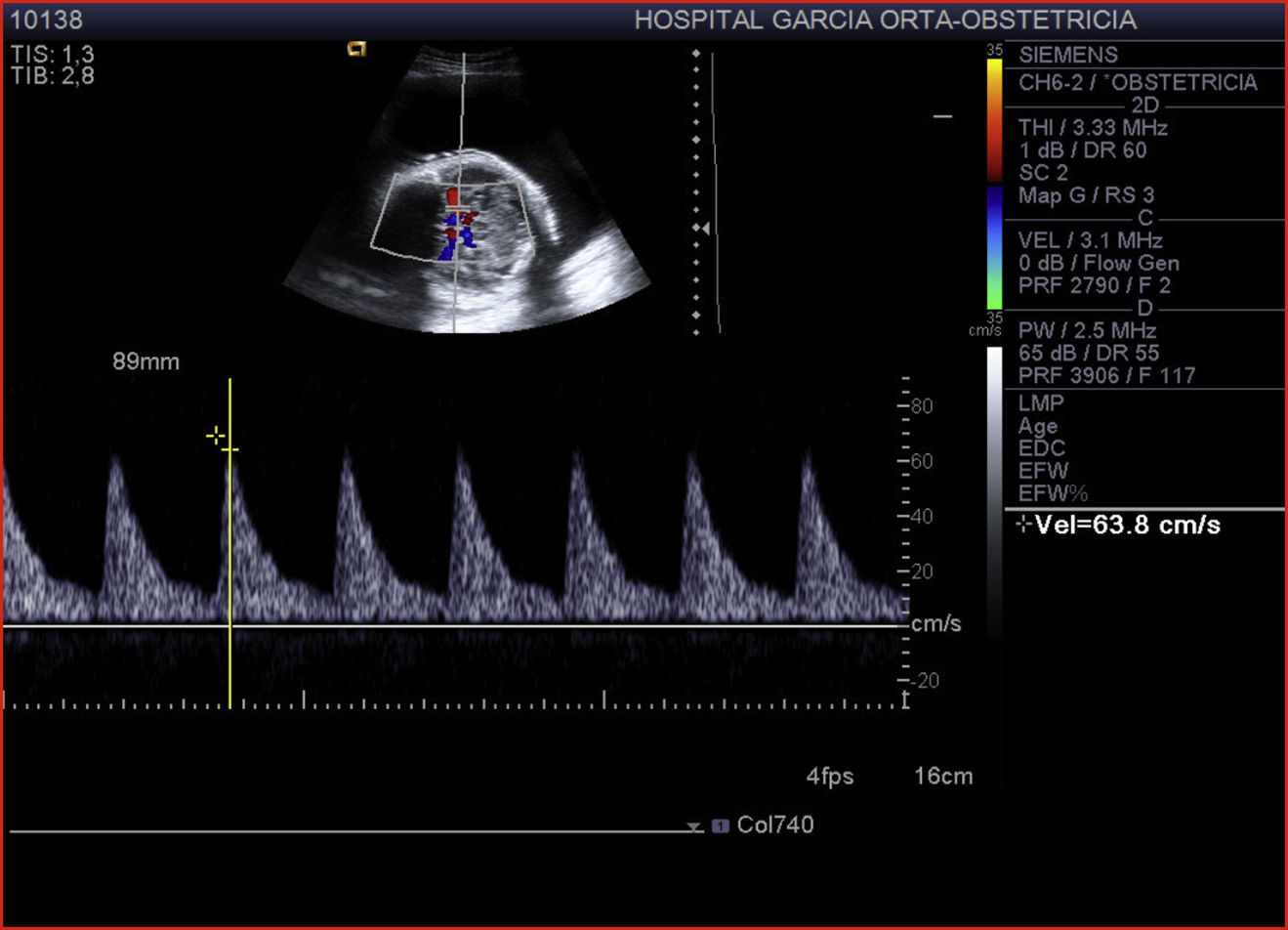
Serial ultrasound scans showed receding alterations in the tumor's characteristics – a reduction in the vascularization and the appearance of hypoechoic areas in its interior, which suggested tumor necrosis (Fig. 3). At 34 weeks and 2 days gestation, an extensive area of subchorionic hematoma (69mm×50mm×10mm) was detected, adjacent to the tumor. Due to the risk of impending placental abruption, we decided to terminate the pregnancy with a cesarean section, delivering a female infant weighing 2030g, with 1- and 5-minute Apgar scores of 9 and 10, respectively. Hemoglobin evaluation of the newborn revealed 13.1g/dL, but no transfusion was needed.
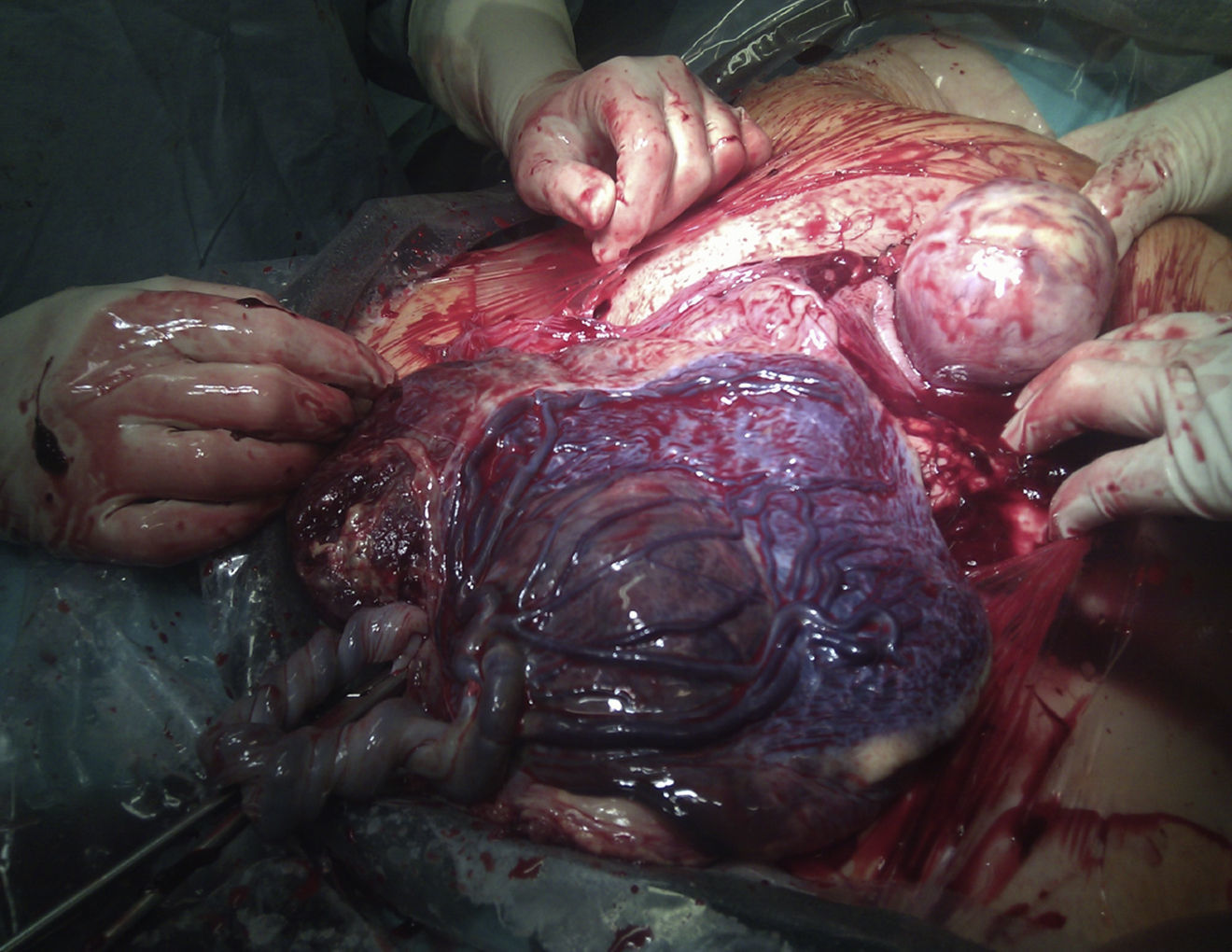
The placenta weighed 430g, with a mass consistent with a chorioangioma measuring 76mm×35mm bordering the chord insertion (Fig. 4). Microscopy examination revealed extensive necrosis of the tumor and thrombosis of an adjacent fetal vessel.
DiscussionPlacental chorioangiomas were initially described by John Clarke in 1798.1 They are the most common non-trophoblastic placental tumors, occurring in approximately 1% of all pregnancies, and are thought to derive from primitive chorionic mesenchyme (with perfusion arising from the fetal circulation).2,3 The majority of chorioangiomas are small and remain undetected with no clinical significance, however, those greater than 4–5cm can give rise to a variety of complications, such as fetal anemia, polyhydramnios, placental abruption, premature labor and, ultimately, fetal demise, with an estimated mortality of 30–40%.3,4
Diagnosis is made by bidimensional ultrasound, usually in the second trimester, where a well circumscribed, encapsulated, echogenic mass is seen protruding into the amniotic cavity, frequently localized in close proximity to the cord insertion.
Pulsed Doppler can help differentiate chorioangiomas from other placental tumors, as the first usually have a vascularized core.5 The degree of vascularity of the tumor is crucial in determining the potential risk for complications – as postulated by Jauniaux and Ogle, the greater the vascularity (independent of tumor size), the larger the association with fetal and neonatal complications.6
Management usually lies in treating the complications, but, in selected cases, ablation of the tumor's vascular bed (e.g. by alcohol or coil embolization) can result in a decrease in its vascularity, which in turn may lead to a reduction in the probability for potential complications. These techniques, however, are not without risk.7
In this case study, we present a giant hypervascular chorioangioma, causing fetal hemodynamic repercussions which were seen to reverse. The proximity of the tumor vessels to umbilical cord insertion made the occlusion the tumors vessels a last resort. It is possible that the tumor necrosis suggested by ultrasound led to a reduction in its degree of vascularity, which avoided the severe hemodynamic consequences initially foreseen. The regular monitoring with CTG and frequent ultrasound scanning with Doppler studies allowed for a timely intervention after fetal lung maturation, with a favorable result.
Conflicts of interestThe authors declare no conflicts of interest.