Policies and health actions generate benefits that extrapolate the specificity of its purpose of providing welfare for the population, given its recognized impact in generating technological innovations, employment and income. However, such progress levels are unevenly distributed in countries, so that certain diseases and allocative and ethical questions associated with the development of new mechanisms for diagnosis, of treatment and cure did not find satisfactory answers yet. In Brazil, such a scenario has not been shown different, demanding a wider discussion encompassing the country's economic and social conditions. Contrasting the analytical and empirical results observed in policies and actions toward the Health Economic-Industrial Complex (CEIS) to establish the barriers as well as structural and economic opportunities for the promotion of health innovations in Brazil, this work raises a number of critical considerations in view of identifying and systematizing gaps in health innovation in the country, thereby proposing a positive comprehensive research agenda on the topic.
In the last decade, Brazil developed some guidelines aiming at strengthening the national system for the promotion of Science, Technology and Innovation (S,T&I) in health. As a highlight, we mention the advent of the Sectoral Funds in 1999; of the Industrial, Technological and Foreign Trade Policy (PITCE) in 2003; the Productive Development Plan (PDP) in 2008; the Greater Brazil Plan (PBM) in 2011; the National Strategy for Science, Technology and Innovation (ENCTI) of the Ministry of Science, Technology and Innovation (MCTI) from 2012 to 2015 and, more recently, from 2016 to 2019. In addition to these policy actions, some others are being established as a way to strengthen innovation and technology development in the health segment, such as the creation of the Executive Group of the Health Industrial Complex (GECIS) in 2007, the CT-Health Fund and the National S,T&I Policy for Health in 2004 and the Program for the Development of the Health Industrial Complex (PROCIS) in 2012. In this work we mention the names of the programs in English but maintain their original Brazilian Portuguese acronyms.
In Brazil, persist a lack of coherent and functional health policies that include a more effective participation of universities and firms in the creation and transformation processes of knowledge into internationally competitive innovations. This aspect obfuscates the gains achieved so far (Viana & Elias, 2007). This point is still featured in the document of the “ENCTI from 2016 to 2019” of the MCTI (Ministry of Science, Technology and Innovation, 2015), which shows the high Brazilian dependence on foreign technologies and innovations in health care. This is a clear justification for highlighting the need for a research agenda in the area of health innovations in Brazil.
These aspects influence the Brazilian development agenda, giving rise to concerns on what increases the vulnerability of the national health system, bringing to light the need to deepen the scientific knowledge based on the subject. Despite the institutional gains achieved when comparing the current situation with that of two decades ago (Marques, 1999), a challenge that persists remains overcoming the fragile national production structure, with an emphasis on both health products and the medical supplies sides (Gadelha, Vargas, Maldonado, & Barbosa, 2013). Other aspects are added, such as the reorientation of technological innovations, a structural link in public policy, and the establishment of the collective welfare of the country (Gadelha, Costa, & Bahia, 2015).
The Brazilian government has a significant role in the development of a socially and economically important production base to increase the technological density of the Economic Industrial Health Complex (CEIS). According to Gadelha (2003), the CEIS is a structural link that involves not only social demands for goods and services in health, but also a technologically competitive production base. It consists of dynamic and systemic secondary links that, although quite different from each other, share the same political and institutional frameworks. Thus, the action of the Brazilian government is potentially inducing the dynamics of a dense and complex production chain as the CEIS because of the centrality of government in the procurement of goods and services and in inducing regional policies in health services (Bahia, Costa, Gadelha, & Vargas, 2015).
There is therefore the need for a wide-ranging discussion about the difficulties of communication and consolidation of CEIS in light of specific characteristics, economic and social conditions and the corporate and government dynamics. Thus, contrasting the analytical and empirical results, this paper aims to highlight the health innovation gaps in Brazil and raise a set of concerns around three central axes toward the composition of a research agenda on health innovations in Brazil. The intention is to place the barriers and structural/conjectural opportunities for the support of health innovation in Brazil. It is worth mentioning that the issues and considerations raised no claim of completeness of the theme, as the focus of this work is to contribute to a broader debate on this subject, which we believe is important to the development of Brazil and other developing countries in similar conditions.
This paper is divided into six sections, including this introduction. Section 2 discusses the concept of Health Innovation System (HIS), rescuing a number of recent considerations of the literature on the evolution of HIS, highlighting its implications for Brazil. Section 3 provides an overview of challenges and international efforts in health S,T&I. Section 4 presents the methodological aspects of the research. Section 5 contextualizes and discusses health innovation gaps in Brazil. Finally, Section 6 elaborates the final considerations.
Health Innovation Systems (HIS): a review of literatureThe stylized dynamics of a Health Innovation System (HIS) stems from the widespread knowledge available in the literature on innovation systems (IS). A HIS is a system driven by endogenous and localized interactions between various units, such as the ecology of agents and their connections, by coordination mechanisms brought by the institutional environment, and by the growing interdependencies between domains (Orsenigo, Dosi, & Mazzucato, 2006). Different aspects such as scientific research, regulation, patient care and market processes are translated to these domains, whereby innovations are non-deterministic and emergent processes (Bloom & Wolcott, 2013). The role of social technologies is also important, as well as the institutional propagators along the coordination processes that facilitate the implementation of scientific and technological advances within the clinical activity in medicine (Consoli & Mina, 2009). Having said that, a HIS characterizes a rich ecosystem formed by individuals, institutions and organizations whose interactions aim to contribute over time to the emergence of coherent paths of technological change. Such environments emphasize the collective nature and long-term innovation processes and their dependence on generated feedback mechanisms during the delivery process of medical innovations to society, without, however, skew the incentive systems that move the different subsystems.
Therefore, an HIS encompasses a broad sphere of medical technologies and clinical services, such as new drugs, devices and medical practices that occur in the context of social technologies and institutional structures, which in turn generate the conditions for both release and dissemination. As a result, the attention of public policy must be given not only to the development of intermediate goods for the provision of health services, but also for organizational and institutional settings that support the development and introduction of new medical technologies (Gadelha et al., 2013).
The greatest challenge of our time for the consolidation of a HIS is in the design of more appropriate interpretative models of the diffusion and utilization processes of medical technologies. However, an extensive literature states that use and development of technologies are variables that go together in an innovation process that mutually shapes one another throughout a learning process, which, in turn, expands or reduces the scope for the application of the technology (Bloom & Wolcott, 2013; Gelijns & Rosenberg, 1994). The greatest difficulty, however, is in the set of assumptions that support each interpretative model.
For example, Consoli and Mina (2009) discuss the role of hospital managers, patients, insurers and regulators in the rate of diffusion and direction of medical innovations throughout the importance of these actors in the explicit identification of priorities and in the redefinition of modes of functioning and funding strategies that stimulate the emergence and spread of new technologies. Consoli and Mina (2009) argue that studies on the roles users in the adoption of innovations in the medical field are treated as static components of their analysis.
On the other hand, approaches more typically framed in the fields of sociology and health policies see the incorporation of medical technologies as a result of a process of change in time, which involve considerations on the evolution of the mechanisms by which the demand for new treatments and technologies are established and financed. Innovation in health herein outlined involves a variety of forms of knowledge whose evolutionary paths are rooted in the contexts in which they emerge and interact (Bloom & Wolcott, 2013). Such analytical considerations emphasize the historical and institutional perspectives, as well as technological dimensions outlined above. Therefore, a proper understanding of how an HIS evolves in terms of its main objectives comes from whether its development perspective is geared toward a dynamic or a static framework, whereby, in each case, institutional processes are compared with technological processes (Consoli & Mina, 2009).
Consoli and Mina (2009) suggest HIS approaches to be seen on a functional perspective. That is, development strategies based on the optics of Health Innovation Systems should focus on the aspects that originally initiate an Innovation System. This means that the greatest wealth of the concepts and theories of Innovation System is in its ability to emerge and develop in response to specific problems whose solutions employ different forms of expertise that depend on its coordination. In other words, the contours of such systems suffer continuous evolution, transcending sectoral or technical barriers. The most important aspects of this process are all the changes in the institutional structure, which gives supports to the IS.
Therefore, the IS approach aligns to both the overall medical and clinical settings. On the one hand, the organization of health services starts a wide range of activities involving technical skills and practical knowledge, which require efficient coordination mechanisms aimed to achieve certain standards of patient care (Gadelha et al., 2013). On the other, the search for the implementation of new clinical solutions in the context of an IS directs the redistribution of knowledge along the areas of expertise, giving opportunities for new connections that, in its turn, lead to other connections and so on (Bloom & Wolcott, 2013).
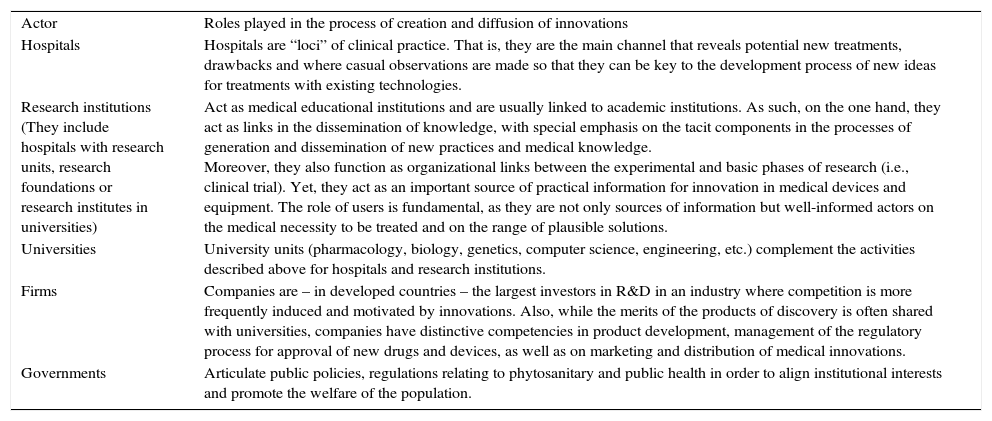
In this line of reasoning, the concept of CEIS is an interpretative model of the operation of an HIS that starts from the dynamic perspectives of relations, on both the institution and the technology sides. In Box 1 we summarize the main actors in a CEIS, as well as their roles in the process of generation, dissemination and use of innovations in the healthcare industry.
Main actors of a health innovation system
| Actor | Roles played in the process of creation and diffusion of innovations |
| Hospitals | Hospitals are “loci” of clinical practice. That is, they are the main channel that reveals potential new treatments, drawbacks and where casual observations are made so that they can be key to the development process of new ideas for treatments with existing technologies. |
| Research institutions (They include hospitals with research units, research foundations or research institutes in universities) | Act as medical educational institutions and are usually linked to academic institutions. As such, on the one hand, they act as links in the dissemination of knowledge, with special emphasis on the tacit components in the processes of generation and dissemination of new practices and medical knowledge. Moreover, they also function as organizational links between the experimental and basic phases of research (i.e., clinical trial). Yet, they act as an important source of practical information for innovation in medical devices and equipment. The role of users is fundamental, as they are not only sources of information but well-informed actors on the medical necessity to be treated and on the range of plausible solutions. |
| Universities | University units (pharmacology, biology, genetics, computer science, engineering, etc.) complement the activities described above for hospitals and research institutions. |
| Firms | Companies are – in developed countries – the largest investors in R&D in an industry where competition is more frequently induced and motivated by innovations. Also, while the merits of the products of discovery is often shared with universities, companies have distinctive competencies in product development, management of the regulatory process for approval of new drugs and devices, as well as on marketing and distribution of medical innovations. |
| Governments | Articulate public policies, regulations relating to phytosanitary and public health in order to align institutional interests and promote the welfare of the population. |
Source: authors’ elaboration on Gadelha et al. (2013), Gelijns and Rosenberg (1994), Consoli and Mina (2009), and Mazzucato and Dosi (2006).
Conceived as a link in the expansion of the operation of the CEIS, Brazil's National Health Plan from 2016 to 2019, or PNS 2016–2019, comes under the guidelines of the National Health Council (CNS) to stimulate the expansion of domestic production of strategic technologies in healthcare. Therefore, one of the PNS's objectives is to “promote the production and dissemination of scientific and technological knowledge, health situational analysis, health innovations and the expansion of domestic production of strategic technologies for the Unified Health System (SUS)” (Ministry of Health, 2016, p. 69). Despite this focus, both the PNS 2016–2019 and the ENCTI 2016–2019 do not show, for example, a proposal for the configuration of an institutional framework encompassing actors, roles, responsibilities and resources aimed at linking a process of diffusion and use of medical technologies promoted by a national HIS or by many regionalized HIS around specific themes, as well as the existing or required resources to ensure its feasibility. In the attempt to contribute to this debate on the need to expand the Brazilian HIS that the next topics of this work are established. But before that, we believe it is necessary to present a set of broader perspectives on the matter, along with the current challenges for health innovation.
Perspectives and challenges in health innovationIn order to face more emphatically the current worldwide problems in health innovation, the OECD suggests that the attention of public policies and the interested society segments should focus on three main aspects: (i) science and technology; (ii) industrial organization; and (iii) financial barriers (Organization for Economic Cooperation and Development, 2010).
The HIS is the process by which new drugs, vaccines and diagnostics are produced and made available to its users. It is an environment that has suffered from declining productivity, rising operating and research and development (R&D), and risks of patents’ infringements in developing countries (Durand-Zaleski, Chevreul, & Jeanblanc, 2009; Hyewon, 2014; Organization for Economic Cooperation and Development, 2013; Stossel, 2015). Still, failure and rejection rates remain high despite of the promises brought by new technologies. It is possible that there is a difficulty of pharmaceutical companies to properly address the solutions to the different demands generated in the HIS, reflecting to some extent in their market value, which has led to a number of mergers, acquisitions and strategic alliances worldwide (Davis & Abraham, 2013). Summarizing, there is uncertainty about the future structure of the biopharmaceutical industries and global biotechnology, creating challenges in their management processes of knowledge, intellectual property and innovation.
The structure of the biopharmaceutical industry is a hotly debated topic. Some see the increased outsourcing of services and knowledge management as a new production organization of the pharmaceutical industry oriented to the formation of ecosystems over global networks, outsourcing certain services, such as R&D. It is a common reality in other sectors, such as semiconductors (Lange, Muller-Seitz, & Windeler, 2013). Others, however, believe that the difficult capital investment decisions and the complexity of the health sector indicate a return to a more vertically integrated structure (Organization for Economic Cooperation and Development, 2010).
The search for financing in the early stages of research, the high development costs of products and government approvals, financial pressures and their impact on the market value of biotech and pharmaceutical companies, as well as restrictions on the public purse has been a constant in the industry (Industrial Research Institute, 2015; Stossel, 2015).
Therefore, in view of the challenges in science and technology, in industry organization, and in the financial constraints (on the public and private sides), the prospects of policies for densifying production chains harboring different interests throughout their nodes, even among those in the public sector, present challenges not only in the governance structure, but also on the outcomes expected by society. Health Innovation Systems in industrialized economies are in transition, seeking more efficient forms of productive and knowledge organization, as well as more functional models for evaluating uncertain and long-term maturity investments in knowledge intensive projects (Organization for Economic Cooperation and Development, 2013). In a context such as of Brazil, in which the problems and challenges mentioned above coexist with the low national capacity to carry out R&D and to produce innovations aligned with the national picture of health and disease of the population, such problems become of even greater dimensions.
Materials and methodsThere is a significant number of researches by Brazilian authors exploring the institutional links to the consolidation of local innovation systems, the cultural and systemic determinants of innovation among firms, as well as on the dynamics underpinning university–industry cooperation for innovation and its role in generating successful spin-offs (Botelho & Almeida, 2010; Machado & Barzotto, 2014; Paranhos & Hasenclever, 2011; Viana & Elias, 2007).
However, there is still little knowledge about how public policy, in particular the S,T&I policies, influence business conditions in general and, more specifically, the business models and business strategies of firms, given the barriers and the very dependence of Brazilian companies to public funding.
Given the limited availability of studies on this topic assessing the context of Brazil and other developing countries, the authors have adopted a “how” and “why” questioning perspective as a theory-building approach (Yin, 2003). The research is therefore exploratory, as it directly responds to the need of building the foundations of a theory exploring the relationship between the gaps in health innovation in Brazil and the research agenda required to analyze, propose and debate the amplified set of actions required to overcome these gaps. Consequently, given the exploratory nature of this research paper, we avoid generating hypotheses to test relationships between variables (Edmondson & McManus, 2007).
The first stage in this research consisted in the review of literature to present the state of the art in science, technology and innovation in health. The second stage comprised documental analysis involving the Brazilian health policies framework and the situation of the domestic industry in health-related areas. The analysis generated a process through which a company, public policy or sectoral context studied indicated further evidence of government and business spheres to be analyzed. Because of this process, two new documents released by the Brazilian Federal Government were included in the research for analysis: The National Strategy for Science and Technology (ENCTI) from 2016 to 2019 and the National Health Plan (NHP) from 2016 to 2019. In this way, we believe we can contribute to a better understanding of the recent health S,T&I policy framework in Brazil, as well as with a set of propositional issues related to a future agenda for more comprehensive research on the theme, which we deem necessary to reduce the gaps between innovation and health in the country.
Data analysis had two purposes in this research. First, it allowed the identification of the analytical framework within which the authors highlighted the set of gaps for health innovation. Second, it allowed for a more detailed understanding of the current outlook of the Brazilian public policy, including a systematization of the challenges ahead. The data were crosschecked with information from public sources (press, company websites, scientific articles and consultancy reports), which allowed the construction and the triangulation of evidence provided by the study.
The authors acknowledge that caution is required in making generalizations based on the results of an exploratory research. However, we expect that the exploratory nature of this study will not invalidate its merit as an empirical research effort, as it highlights the need for a clearer adherence of S,T&I health policies with the national industrial and scientific structures. This approach is aligned with international best practices in exploratory research employing surveys or case studies on themes exploring how S,T&I policies evolve in response to demands of society (Lange et al., 2013; Lehoux, Daudelin, Williams-Jones, Denis, & Longo, 2014; Probert, Connel, & Mina, 2013).
Still, the identification of the required constructs for the proposal of a set of questions relevant for a research agenda that, accompanied by an extrapolation in the final remarks and the urgency in meeting these issues, proved to be a valid strategy for exploring such a complex theme in a developing country context. Similar approaches were presented in Parasuraman and Grewal (2000) and Aguinis and Glavas (2012).
As a way to analyze the data, the authors set out the conceptual framework of analysis carried out by the OECD (Organization for Economic Cooperation and Development, 2010, 2013), choosing to systematize the gaps in science and health technology in Brazil along in three main axes: (i) science and technology; (ii) industrial organization; and (iii) financial barriers. In each of these axes we present a set of propositional questions aimed at stimulating an integrated research agenda and a debate on health innovation in the context of a developing country like Brazil. Next, we present and discuss the three axes in the light of the recent Brazilian experience.
Gaps and challenges for BrazilIn view of various challenges to the consolidation of a CEIS in the country, the Brazilian Innovation Agency (FINEP) and the National Bank for Economic and Social Development (BNDES), along with the Ministry of Health (MS), have presented a set of structured proposals to ensure a decentralized development to the actions for Science, Technology and Innovation in Brazil. Based on the structure presented by the documents of the OECD (2010, 2013), we discuss the gaps and challenges in Brazil in light of the Brazilian federal government action plans envisaging more effective innovation health developments in the country, as presented by both the ENCTI from 2016 to 2019 and the PNS from 2016 to 2019.
Science & technologyOne cannot consider the science and technology policy framework in Brazil without mentioning the country's Innovation Law. With the entry of the Innovation Law (Law No. 10.973/2004) and its regulation through Decree No. 5,563 in October 2005, Brazil started to have a new funding instrument for innovation and scientific research and technology in the national production environment. The Brazilian Innovation Law aims to establish a set of mechanisms to facilitate the transfer of researchers between the science and technology institutions and business segments, with researchers working in the private sector without losing their formal link with their home institutions. In addition, several of its main mechanisms and guidelines are focused on the promotion and funding of university–industry cooperation. Despite the huge challenges ahead, the Innovation Law introduced in the country the notion that an important part of the bottlenecks in university–industry cooperation is to reduce institutional and legal barriers that prevented those actors who have already envisioned university–industry cooperation as a key link in the generation of high economic impact innovations.
However, after ten years of its enactment, the Innovation Law has not proved as effective as expected. Some strategic sectors, such as health technologies, biofuels, semiconductor and oil & gas have not managed to take off, despite the framework enacted for their development, even after the introduction of this Law and other support mechanisms derived from the Law (Alves, Quelhas, da Silva, & Lameira, 2015; Pinto & Feldmann, 2016; Suzigan, Albuquerque, & Cario, 2011).
The purpose of the Innovation Law was to extend the public–private partnership for innovation, but the interface between the public and private sectors does not happen only in the context of research networks, but also in the legal relationship between the parties. One of the recurring diagnosis is that the bottleneck of this partnership would be mainly in the public sector (Alves & Pimenta-Bueno, 2014; Suzigan et al., 2011). It was in this context that the law authorized the creation of Special Purpose Companies (SPC) to develop projects in partnership with private partners. These companies should be subsidiaries of research institutions so that, in the future, this should allow SCPs to count on the income generated by this type of institutional innovation. There are, however, concerns about the consistency of the Law. First, because it creates some legal instruments for university–industry cooperation but does not improve, for example, the flexibility and autonomy of public institutions in managing their human and financial resources. Later, the Law devotes significant attention to the commercialization efforts of the innovation, but not to the creation of research capacity within private enterprises (Botelho & Almeida, 2010).
Until recently, the Brazilian Innovation Law lacked more precise regulation regarding aspects such as the treatment of intellectual property produced by university researchers with companies, as well as the appropriate legal treatment to researchers in the rigid statutory regime of federal public universities who are actively involved in private companies, among other things. Resulting from an intense debate over the last decade in Brazil, Law No. 13,243 of January 11, 2016, provides new incentives to scientific and technological development, research, and innovation for the country. This new Law emerged in lieu of the 2004 Innovation Law. However, it is still early to know if such aspects as listed above shall be indeed settled, since many of these issues still need further specific regulations at the federal level and, consequently, also in the state levels.
Yet, although a wider investigation of its determinants in the country remains necessary, it is possible that the structure and dynamics of health innovations in Brazil are being set out on generally assumed foundations rather than thoroughly discussed and analyzed with the actors and stakeholders involved. Innovations in the biomedical and pharmaceutical fields depend on the context in which they operate and should not occur isolated from the characteristic framework underlying their socioeconomic systems, which are necessary for the definition of their organizational and market basis. For example, the case involving the national mobilization around the epidemic potential of the Zika virus required a broader national effort, with different forms of expertise formed around a specific issue of potential socioeconomic consequences. Such problems do also occur in other areas of the clinical practice and general health in Brazil, each requiring different forms of coordination and resource mobilization around the same functional structure at the national and regional basis, as it should be the country's CEIS.
Therefore, besides the challenges brought by the decline in production and exports of two links of the Brazilian CEIS (Chemical Industry and Biotechnology Base and Mechanical, Electronics and Materials Industry Base), there is still another challenge to be overcome by national health S,T&I policies. Regarding the innovation process, in general, the pharmaceutical and national medical equipment industry also reveals a clear detachment of the world's technological frontier (Gadelha et al., 2013). This is evident particularly in terms of the significant gap between the national and international competitive standards in R&D efforts, especially in those segments with higher technological density as biological drugs or biopharmaceuticals (Federal Planning Bureau, 2013; Gadelha et al., 2015).
The considerations above result in the discussion made in Brazil on the importance of coordination among institutional actors along the CEIS to address the risks outlined (Gadelha et al., 2013). Some researchers believe that the motivation of these aspects is the relative neglect of the role played by the service sector in innovation studies (Consoli & Mina, 2009), therefore influencing how the articulation of public policies for the Health Innovation System evolves and consolidates.
In face of what was earlier discussed, one of the goals in the Ministry of Health's PNS (2016, p. 69) is to “promote the production and dissemination of scientific and technological knowledge, health situational analysis, health innovation and the production expansion of national strategic technologies for the Unified Health System (SUS)”. The goals set out in the PNS aim to meet a four-year planning horizon (2016–2019), thereby suggesting the still low evolution of the health innovation process in Brazil. To achieve these ends, the PNS presents a comprehensive set of strategic goals (Ministry of Health, 2016, p. 70). The first is to increase from 1 to 9 the number of technologies internalized in the country's Unified Health System (SUS), which will be produced by the Partnerships for Productive Development (PDP). Second, to promote scientific research, technology and innovation aimed at improving the health condition of the population and to improve the mechanisms and management tools for the regulation and health care in the SUS. Third, to develop and/or absorb through the PDPs 8 new drugs.
These objectives and targets in the PNS show that little progress has been made in recent years and that the problems faced are still persisting in health innovation policies and actions. The national effort is still shy, which implies the need for a research agenda on the following questions:
- •
Assuming that the university-business cooperation presupposes very different organizational structures – depending on the maturity of the relationship, on the objectives for the cooperation, etc. – how to better encourage, in the context of the targets, goals and strategies encompassed in the PNS 2016–2019, the university–industry cooperation for health innovation?
- •
How to increase the flow of researchers, scientists and technology and innovation managers of public and private institutions in health and related areas, aiming at a better socioeconomic exploitation of the knowledge shared that is useful for both the public and the private parties?
- •
As globalization accelerates, and in face of the specificities and disparities between Brazilian States, how to coherently address the development of new platforms and technological standards for the health of the population, with a view to a necessary convergence of technologies in areas such as biology, engineering, computer science, synthetic biology and nanotechnology?
- •
With distinct and specific interests in multiple territories of the country, the consolidation of local capacity to boost the potential for innovation involves ensuring access to multiple data sources, domestic and foreign. Make these data sources interoperable in a continental country is a challenge that requires more efficient use of sophisticated information and communication technologies to interconnect the resources and make them more efficiently available to their users.
The domestic market of medicines, drugs and adjuvants changed substantially from 2010 onwards, with imports of medicines ranking five times higher than the exports. For drugs and adjuvants, the scenario is even less favorable for Brazilian exports in relation to imports. The main causes of such a performance degradation, in the industry point of view, was attributed to the federal and state tax structures and the detrimental public oversight and regulatory barriers to domestic producers over those of foreign origin (Brazilian Association of Pharmaceutical Chemicals Industry and Pharmaceutical Supplies, 2014).
Despite the drop in exports of medicines and pharmaceutical supplies, the scenario that prevailed until 2010 was of representative growth. Most likely, in addition to the structural issues that affect the performance of the Brazilian industry, the unfavorable international economic environment also contributed to the drop in the performance of Brazilian exports of medicines and pharmaceutical supplies. One of the elements that contributed to the growth in production observed until 2010 – and consequently of Brazilian exports – is the consolidation of the ‘generic’ medicines segment in the country, which represented a turning point in the growth trajectory of the national pharmaceutical industry.
Still, despite the decline in exports from 2010 onwards, imports of pharmaceutical drugs and supplies continue to grow more than exports, especially from China (Brazilian Association of Pharmaceutical Chemicals Industry and Pharmaceutical Supplies, 2014). The fall in exports is a reflection of the overall reduction in Brazilian industrial production since 2011. Also, in 2012 the scenario for the medical equipment market – the mechanical, electronic and materials base of the CEIS – has also changed, reflecting the behavior of the national industry in other sectors as well.
Still, the growth of domestic sales of supplies and equipment for medical and diagnostic purposes has been supported by increasing imports of equipment and raw materials rather than by the domestic production in these segments. Apparently, the increase in domestic sales, particularly of medicines, biopharmaceuticals and medical and dental equipment, even in a still adverse economic scenario shows that the CEIS services base in the country continues to demand inputs and products that are being gradually supplied by imports.
Possibly, the worst scenario for the country would be the absence of the Partnerships for Productive Development (PDPs). The PDPs allowed partnerships between public and private producers for the production of drugs, vaccines, medical equipment and devices for diagnosis. The public sector, particularly the Ministry of Health, was the main client of the partnerships taking place in the framework of the PDPs. Obviously, the fulfillment of the expectations built around these actions will depend on the continuity of long-term policies, the economic conditions, the quality of funded projects and on the criteria for the selection and establishment of partnerships. The PDP, through the existing legal framework, becomes viable by means of the public procurement led by the Ministry of Health, which entails preference margins for the acquisition of domestic products and raw materials.
The ‘Programa Inova Saúde’, or Health Innovate Program, can also become an important partner in the consolidation of these instruments. It is an initiative of the Ministry of Science, Technology and Innovation (MCTI) along with the Brazilian Innovation Agency (FINEP). This initiative occurs in cooperation with the Ministry of Health (MS), the Brazilian Bank for Economic and Social Development (BNDES) and the National Scientific and Technological Development Council (CNPq) to support Research, Development and Innovation (R,D&I) projects from public and private institutions operating under the CEIS. Launched in April 2013, it is still early to assess its effectiveness. However, some aspects related to other initiatives in Brazil and abroad can motivate the construction of an elaborate set of contributions so that the Innovate Health Program can increase its chances of achieving the objectives pursued by its idealizers. The Health Innovate Program was quoted in ENCTI document, noting that: (…) the program achieved significant results in relation to its main objective of creating the support and financing conditions whose results can effectively contribute to the reduction of the country's technological dependence on the supply of important inputs in the field of human health. The program is inserted into the Innovate Enterprise Plan (Programa Inova Empresa), which will allocate R$ 3.6 billion until December 2017 for supporting innovation activities of the Health Complex. (Ministry of Science, Technology and Innovation, 2015, p. 43).
Even with the argument that the program has reaped positive results, the only indication for the expansion of Innovate Health Program is a possible investment of R$ 3.6 billion by the end of 2017. It is still a timid investment compared with other programs like Brazil's Profarma, coordinated by the BNDES.
The consolidation of the generic medicines policy has also boosted the growth of the Brazilian pharmaceuticals market. The BNDES’ Profarma was enacted in this context, when the improvement of the pharmaceuticals value chain was defined as a priority by the PITCE in 2004. The increase in production capacity of the Brazilian pharmaceuticals and health equipment industry, the need to adapt to international standards of production, the expansion of innovation efforts and the need to strengthen national companies were the main objectives defined in the creation of Profarma. Having been redesigned in 2007 to increase the penetration of the CEIS into the national health segments, Profarma focuses on the induction and support of technological innovation projects, as well as to align the industry agenda with the demands of the MS. In its third renewal, active until 2017, Profarma expects to inject an additional R$ 5 billion in these initiatives.
A detailed assessment of the Profarma program involving all its beneficiaries has not yet been performed. Therefore, it is not yet possible to assess the extent of economic externalities and social benefits produced such as skilled job creation by the firms supported, impacts on the CEIS, patents derived by the financed projects and the supported firms turning public through Initial Public Offers and the like. A challenge for Profarma is also to stimulate innovation in small businesses. According data collected by the authors on the institutional websites of the partners of the program, 3/4 of resources released benefited medium and large companies. Small businesses often present difficulties in providing collaterals and to adhere to the strict terms of the public calls (Alves & Pimenta-Bueno, 2014).
Still, a similar situation occurs in the nuclear technology sector, which is strategic for health innovations. Despite the observed improvements, nuclear technologies are underutilized in the country, with relatively low investments in the public sphere and practically none in the private, as noted by the ENCTI document itself (Ministry of Science, Technology and Innovation, 2015, p. 15).
The new possibilities for outsourcing R&D services in health, as noted worldwide, are an important link to be captured by national policies, since attracting foreign research labs can bring positive externalities that contribute to the consolidation of the CEIS. This aspect goes beyond the public policy framework mentioned in previous lines, as it involves a more comprehensive articulation with a myriad of actors aiming to design the most appropriate set of incentives and protection measures to facilitate the entry into the country of these global players.
Actions and national business strategies should therefore focus on business models that allow business players to remain economically viable in an environment of uncertainty and increased competition with both industrialized and developing economies. Each of the national CEIS segments demand detailed assessments of new trends in the markets for raw materials, products, technologies and health services, especially public health, requiring different strategies. These strategies should encompass: (i) a solid schedule for private R&D going beyond the next five years; (ii) an efficient management of intellectual property and contracts in partnership with national and foreign entities for the development of new products and services in health; and (iii) marketing strategies that are successful for expanding domestic products and services into new markets, particularly abroad.
Existing restrictions and constraints are a result of the still modest incidence of innovations in Brazilian companies (Botelho & Almeida, 2010; Pinto & Feldmann, 2016), as well as the low launch of new products and services derived by the collaboration of firms with universities and research centers (Alves & Pimenta-Bueno, 2014; Suzigan et al., 2011). Therefore, the role of policy actions such as Innovate Health, Profarma, the PDPs and sector funds (see next section) may be an important link for the solution of these bottlenecks in the coming decades. However, without economic policies that reduce the risks for private investment in the development of goods and services that incorporate, manage and disseminate new technologies, the low appetite of businesspeople in running such risks continue to inhibit and wane the participation of the private sector in these actions. This occurs despite the high S,T&I public policy efforts enacted along the past two decades.
Regarding the industrial organization, the PNS (Ministry of Health, 2016, p. 71) sets out three important goals. The first is to increase from 13 to at least 18 the number of industrial parks supported by the National Program for the Development of the Industrial Health Complex (PROCIS). Second, to start at least 4 large partnership projects encompassing research, development and innovation (R,D&I) efforts under the new framework of the PDPs. Third, to implement a Technological Compensation Agreement (ACT), including the construction of a linear accelerator industrial facility within the framework of the Radiotherapy Expansion Plan in the SUS.
In this scenario, some issues still need to be addressed in the Industrial Organization component. They are as follows:
- •
How to increase exports and Brazil's domestic production in pharmacological and radiopharmaceuticals industries? An increase of five industrial parks, as highlighted in the PNS 2016–2019, will enable the reversal in the trade balance in the coming four years?
- •
How to generate stability and stimulus to pharmacological and radiopharmaceutical production segments in order to allow the framework conditions for the competitiveness of these domestic industries?
- •
With the R&D productivity drop of the pharmaceutical industry in the world, the country can be an important locus for the attraction of investments in new of laboratories in the country, given the lower local R&D overhead costs compared to developed countries. Having said that, what mechanisms can be envisioned for such promotion to occur in the best interest of the improvement in the quality and access to health care in the country? In addition, how the National Health Program will allow the construction of a more comprehensive R&D agenda for the next 4 years?
- •
The entry of new players in the global market, as the R&D capacity is globalizing, increases opportunities for competitive companies from emerging economies. What conditions should be improved and created so that Brazil can become a prominent player in the segment, given the national research infrastructure of universities and research centers, along with major development agencies such as BNDES, FINEP, and CNPq, among others? What conditions should be improved for the private sector to increase its interest and participation in the process of consolidation of a health research agenda in developing countries like Brazil?
Financial instruments operated by FINEP and BNDES are the most representative in fostering S,T&I efforts in the country. The set of available instruments include reimbursable financing, non-refundable (sunk-cost) financing and subsidies. Some other instruments also extend to equity investing like seed and venture capital, especially from direct public sources or privately managed funds with public funding. The existing funds also assume the possibility of combining different modes of financing for Brazilian companies (e.g. reimbursable and sunk-cost funding), as well as the application for grants to fund cooperative projects between companies and universities.
In addition to the policy instruments and programs mentioned earlier, another critical link in the financing of health S,T&I is played by Brazil's so called ‘sectoral funds’. FINEP operates the sectoral funds under the National Scientific and Technological Development Fund (FNDCT). The challenges ahead are still high, given the growing context of resource contention. Cumulatively from 1999 to 2015, the retentions in releases of financial resources from sectoral funds reached R$ 10.7 billion in current values. The values released by these funds in the same period amounted R$ 7.7 billion.1 Having said that, about 58% of budgeted resources for sectoral funds were not released to its users and therefore did not achieve the purposes to which they were designed.
One of the 15 sectoral funds, the CT-Health, had R$ 703.8 million budgeted for investments in health-related innovation projects between 2002 and 2015. Only R$ 409.8 million has reached its beneficiaries. For another health-related fund, CT-Biotechnology, out of the previously R$ 307.1 million budgeted for the same period, only a total of R$ 188.4 million has been released. The resources released so far seem to be still timid to help the country reach the innovation funding patterns of other countries. The decline in releases of sector funds between 2014 and 2015 was 69%. For the Health and Biotechnology sectoral funds, respectively, and at the same period, the funding cuts have achieved 66% and 87%. By comparison, only the United States, China and Japan spent half of the $1.6 trillion of global R&D spending in 2013, nearly a quarter of them in health-related areas (Battelle, 2013).
Among the other sectoral funds, the one with more direct and indirect interfaces with the health segments is the CT-Green-and-yellow (CT Verde e Amarelo), given its interdisciplinary focus. An assessment of projects funded under the CT-Health, CT-Biotechnology and projects supported by CT-Green-and-Yellow with interfaces in health is required since the quality of the projects supported can also contribute to densify research and innovation capacities in the health sector.
The challenges for Brazilian funding agencies are significant, especially in a budget-constrained scenario that may continue in the coming years. The whereabouts in the global economy may also contribute to the increased risk in the business model and in the corporate strategies of the companies supported by Brazilian public funding sources.
Despite the existing constraints in the country, exports of aircrafts and the productivity gains achieved in agriculture and livestock production are good examples of the national technological performance. The role of government has been important, but one cannot disregard the role of the private sector with its capital linked to long-term decisions. Brazil has not yet managed to experience the expected overflow in the intensification of private R&D efforts translating in a better innovative performance of firms in health-related segments (Cassiolato & Soares, 2015; Plaza & Santos, 2011). Specificities in the health segment abound, given its regulatory character by government authorities, long and costly development cycles, time to market, complex intellectual property management processes and high uncertainty in the continuity of their technological paths (Lange et al., 2013; Lehoux et al., 2014).
As a segment of intrinsic complexity, there are important gaps in the nature of private funding in the health sector in the country, particularly with regard to high-tech enterprises. This aspect deserves further investigation, as it implies conditions that can unnecessarily translate into even greater opportunity costs to the private investors, thereby affecting their resource allocation decisions for investments in new projects in the area of health. In fact, when looking at data from the Brazilian Private Equity and Venture Capital Association (ABVCAP), one observes that private equity investments in health-related sectors have been declining since 2011, while others grew – despite the adverse economic scenario prevailing in the country (Brazilian Private Equity and Venture Capital Association, 2016). As we withdraw the recent acquisitions of equity in private hospitals by national and foreign private equity funds operating in the country, the data are even more worrisome, given the importance of this type of investment to innovation (Metrick & Yasuda, 2011).
The PNS from 2016 to 2019 is generalist when presenting its plans to reduce the financial barriers underpinning more coherent and functional health innovations in Brazil. The goals set out by the PNS in regard are as follows (Ministry of Health, 2016, p. 84): (1) to agree on new criteria for apportionment of resources among the federal entities starting from each federative unit's health responsibilities; (2) to establish new modes of resource transfer, inducing full care lines for access to health specializations; and (3) to reduce, on an annual basis, the average price of contractual acquisitions based on PDPs.
Due to the still existing financial barriers for health innovation, we propose the following set of questions on this component:
- •
With the escalating development costs and increased regulatory risks, particularly in the development of drugs, what actions can be envisaged to reduce these costs and risks and to increase private investment, domestic and foreign, in the country?
- •
With high constraints on public spending, how to encourage the private sector to participate more actively? What benefits should be offered to domestic and foreign agents to invest in the various links of the CEIS in the country?
- •
How functionally to fill in the gaps in the funding side, for example, for the so-called ‘valley of death’ (development time gap between scientific discovery and the authorization for clinical testing in humans), in the funding for translational research, as well as for the gaps in the funding available for disease/clinical approaches of lower commercial interest, etc.?
- •
How can the attractiveness of domestic companies be improved to investors, so that they can understand the synergies and value proposition of these enterprises, given the need for further efforts to improve the valuation of assets and companies based on the knowledge they possess?
The low rate and intermittent development of government programs and markets encouraged by governmental actions made that so far the economic, financial and social benefits resulting from the opportunities generated had little impact in terms of reducing the gap between health R&D and innovation in the country. This was due to factors ranging from the complexities involved in scaling up to the governance issues of various institutions and public bodies, including budgetary instability, in combination with the absence of monitoring and evaluation of specific policies and their consequent reformulations and refinements. However, if public policies were not yet sufficient to enable a densification of a national HIS, as proposed by CEIS, they have been providing an important extended life for hospitals, research centers, suppliers and users of health goods and services to accumulate experience in human resource qualification and in the improvement of R&D processes in such a manner to reduce in the future their dependency on public resources.
In view of the set of considerations elaborated in this research paper, it remains urgent to consolidate and expand the efforts for building a research agenda strictly focused on the resolution of restrictions arising from health innovation gaps in the country. Both in the national and international contexts, such agenda ought to consider an extension of the policy scope and respective strategies for monitoring and evaluation of results of the experiments of other countries like Germany, China, France, India, Israel, Switzerland, United States and Japan, as well as in-depth studies of specific ecosystems, institutional arrangements and incentive patterns in selected international programs.
Next, one must establish, from the in-depth analysis of these experiences and of the most recent studies, a comparative assessment of the performance of the Brazilian health innovation policy. This is a necessary component for the strengthening of the constraints of a more competitive CEIS, which reflects the specific links of the Brazilian reality. Third, and in a complementary and concomitant manner, one must establish a multi-institutional research program on indicators and metrics for monitoring and evaluation of health innovation. Finally, one must prioritize the following elements: (i) a mapping and an in depth-analysis of aspects and components identified as critical of health innovation ecosystems, which affect the organization of the health science and technology system; (ii) a study of the evolutionary conditions of governance and of the dynamics of institutional arrangements of Brazilian health innovation policy, which affects the organization of the industry; and (iii) a critical analysis of its current incentive patterns, both public and private, which affect the funding mechanisms.
Such considerations engender a set of measures aimed at a more coordinated, coherent and continuous promotion of CEIS in regards to a competitive international insertion of the national productive base, an improvement of public and private funding institutions and a university–industry relationship more oriented to technological innovation in strategic areas for health in the country. In addition, but not less important, to policy improvement in areas that, even indirectly, affect the quality of domestic services and products provision in pharmaceuticals, inputs and medical equipment.
The Brazilian CEIS, therefore, must incorporate the concerns brought about by aspects of the internationalized science and technology base, of the competitive organization of industry and of the growing shortage of financial resources, to make more efficient the complex process from research to the development of new health technologies and their subsequent dissemination in medical practice, particularly under the SUS, so as to reflect the picture of health and disease of the population with its regional specificities and needs. It is not, as is known, a linear process with beginning, middle and end; but rather a cycle with creation and evolution of complex connections between the agents, typical of a ‘behavioral ecology’ partly shaped by incentive systems established by institutions, including the market, and public and private organizations, which produces the basis for an institutionally more mature and evolutionary CEIS, thus with efficacy and sustainable.
Conflict of interestThe authors declare no conflicts of interest.
The data presented in this Section was collected by the authors from the Ministry of Science, Technology and Innovation website. Available in <http://www.mct.gov.br/index.php/content/view/725.html>. Accessed on 14 October 2016.
Peer Review under the responsibility of Departamento de Administração, Faculdade de Economia, Administração e Contabilidade da Universidade de São Paulo – FEA/USP.