Agenesis of the inferior vena cava is a rare malformation. Its most common cause is dysgenesis during embryogenesis, but it may also be related to intrauterine or perinatal thrombosis. It is usually asymptomatic, associated or not with other congenital malformations and may be related to increased risk of chronic venous insufficiency and deep vein thrombosis, especially in young individuals. Diagnosis is often incidental, during abdominal surgery or radiological procedures. We reported five cases of agenesis of the inferior vena cava detected during electrophysiological procedures.
Agenesia da Veia Cava Inferior
Agenesia da veia cava inferior é uma malformação rara. Sua causa mais comum é a disgenesia durante a embriogênese, mas também pode estar relacionada a trombose intrauterina ou perinatal. Normalmente é assintomática, em associação, ou não, com outras malformações congênitas, e pode cursar com maior risco de insuficiência venosa crônica e trombose venosa profunda, especialmente em jovens. Seu diagnóstico frequentemente é acidental, durante cirurgias abdominais ou procedimentos radiológicos. Relatamos cinco casos de agenesia da veia cava inferior detectada durante procedimentos eletrofisiológicos.
The electrophysiological study is an invasive test used to diagnose heart rhythm and conduction disorders. The test can be used to measure atrioventricular conduction intervals, clarify arrhythmogenic mechanisms, and evaluate antiarrhythmic agent efficacy. Currently, it is used to identify and map re-entrant circuits and ectopic foci for subsequent treatment with catheter ablation. Therefore, the electrophysiological test has diagnostic, therapeutic, and prognostic value.
Access to the heart is usually attained through a femoral or subclavian venipuncture to insert a catheter into the heart chambers. Agenesis of the inferior vena cava is generally an asymptomatic condition that may be unknown to the patient, and can occur in approximately 0.5% of the population.1 During electrophysiological procedures, catheter progression difficulties in the cephalad direction raise the possibility of this anomaly; therefore, manoeuvres are required to confirm the presence of agenesis.
The present study reports on five patients who were admitted to the Electrophysiology Laboratory at the Instituto de Cardiologia do Rio Grande do Sul to undergo ablation and electrophysiological procedures, during which these patients were diagnosed with agenesis of the inferior vena cava.
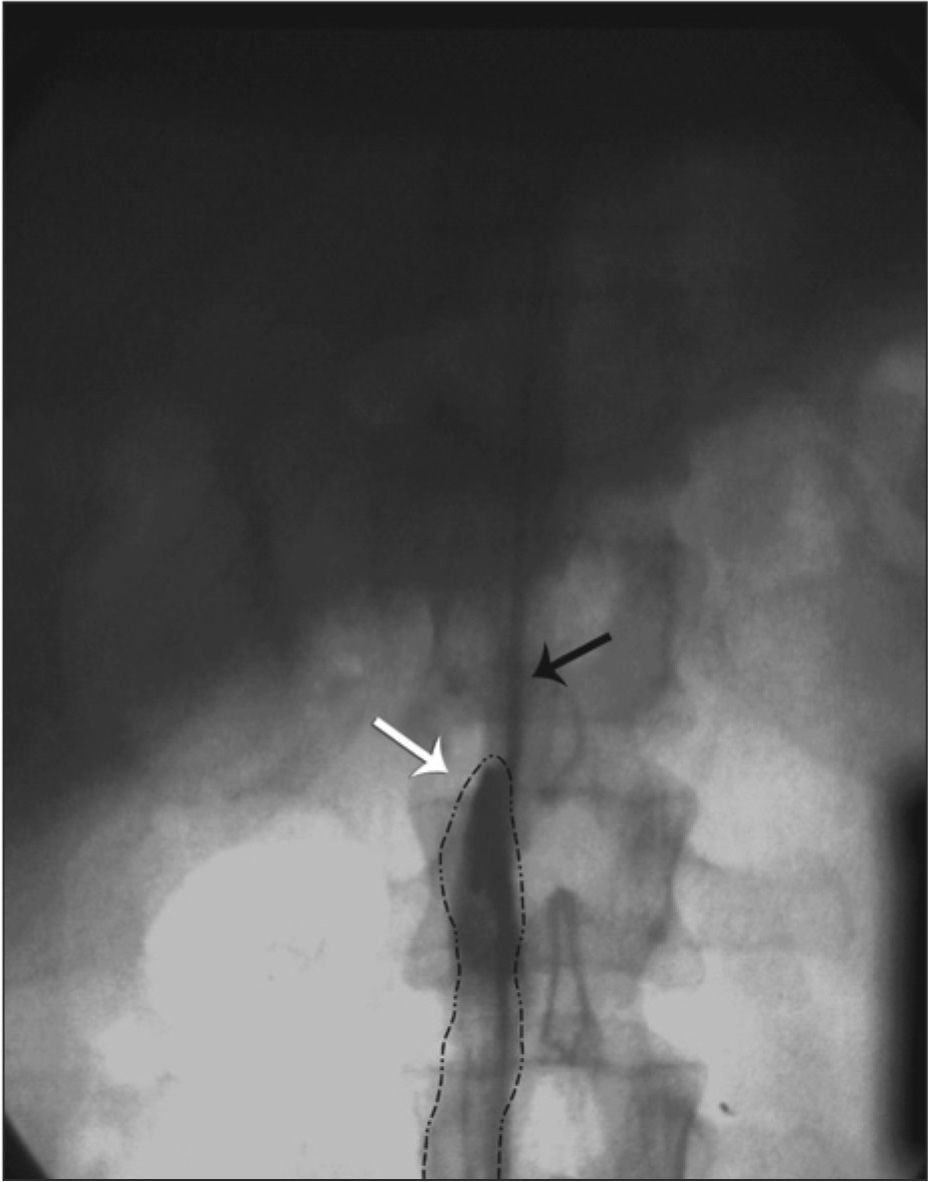
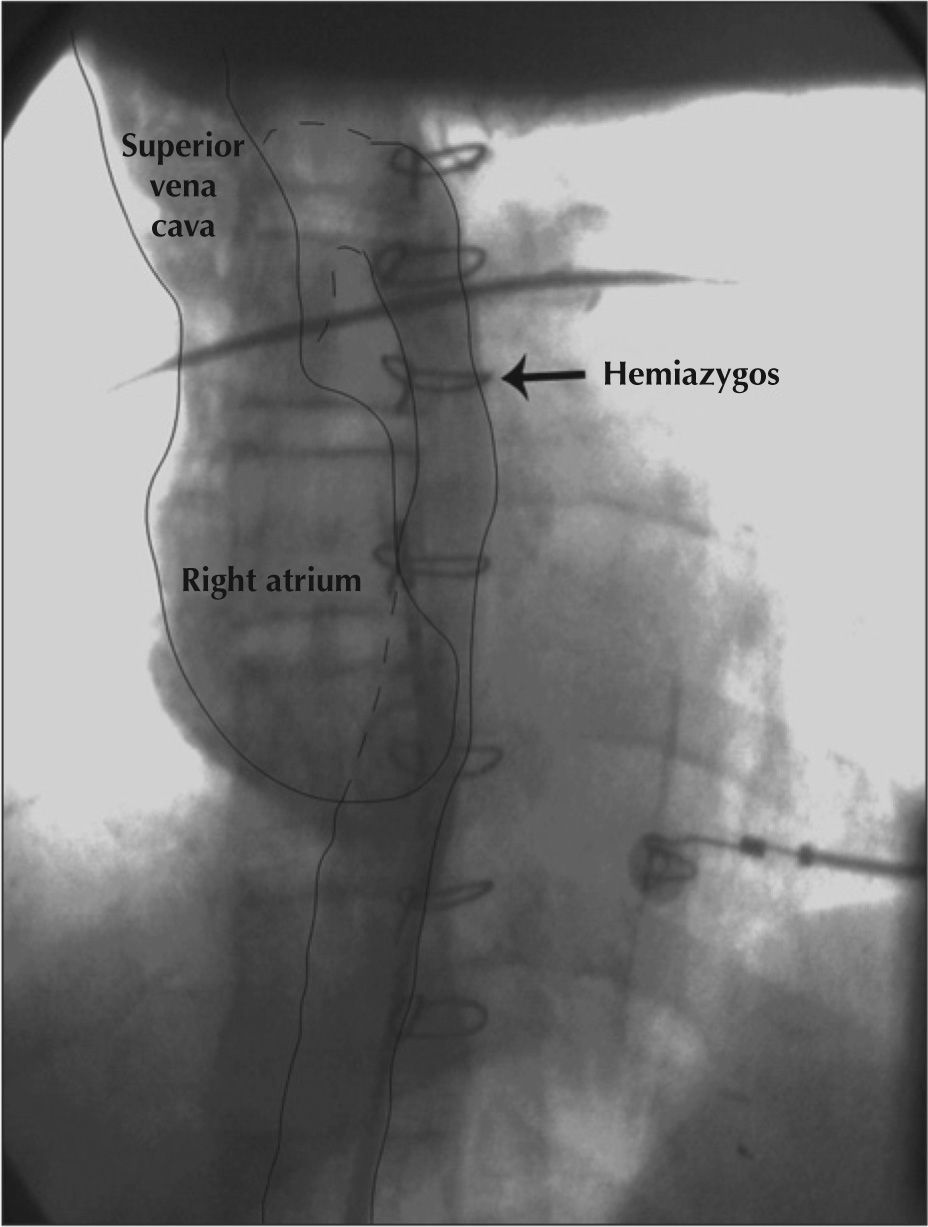
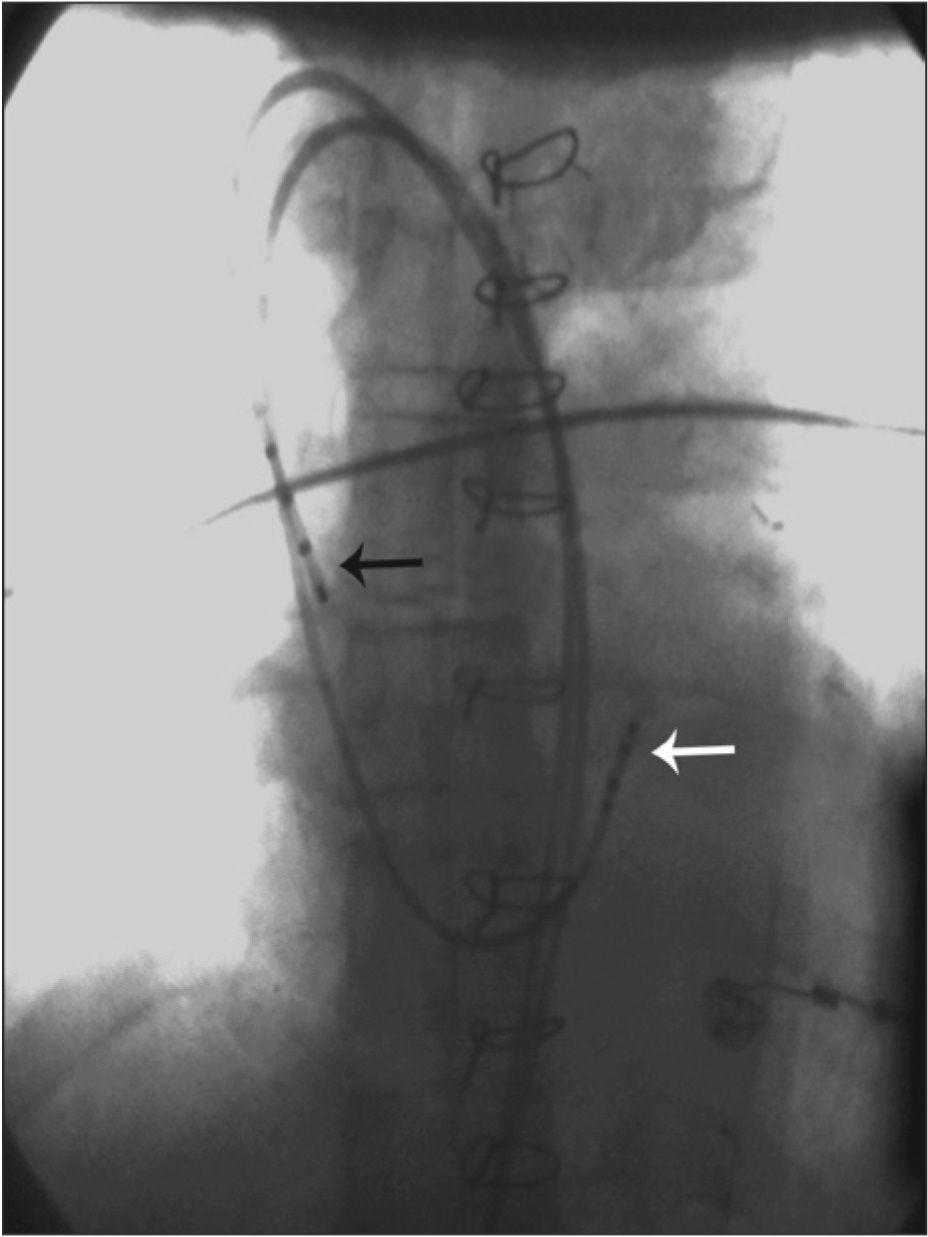
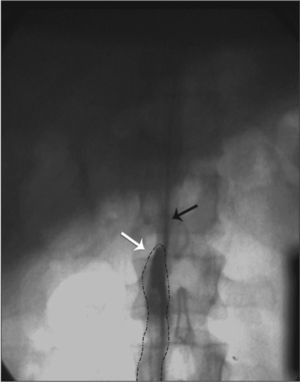
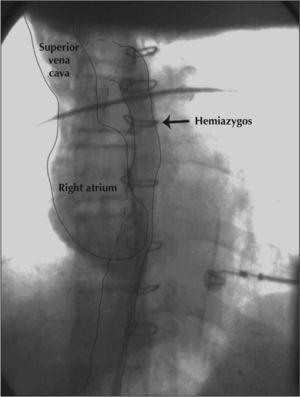
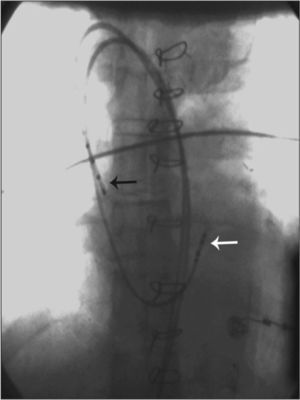
CASE REPORTSCase 1Male patient, 60 years-old, with a history of ischemic stroke in 2005 and acute myocardial infarction in 2007, prior to coronary artery bypass graft (CABG) surgery, and normal ventricular function. In February 2010, the patient was admitted to the Electrophysiology Laboratory for investigation of syncope unrelated to exertion, with no premonitory symptoms; he was submitted to an electrophysiological study with right femoral vein puncture. During catheter insertion, there was difficulty in advancing the cephalad catheter. A venography was performed (Figure 1), which showed agenesis of the inferior vena cava and dilated hemiazygos vein, with venous drainage into the common trunk, the superior vena cava, and subsequently the right atrium (Figure 2). After the venography, an electrophysiological study was performed using a stimulation protocol (Figure 3), which showed normal sinus function and normal atrioventricular and intraventricular conduction.
Female patient, 12 years-old, with tetralogy of Fallot repair (systemic-pulmonary shunt performed in 2000) and a permanent pacemaker for sinus node dysfunction (implanted in 2000). In March 2012, the patient was admitted to the Electrophysiology Laboratory to undergo an electrophysiological study for sudden death stratification. A right femoral venipuncture was performed. Catheterization of the right chambers was attempted using fluoroscopy, without success. A pigtail catheter was inserted, and the venography was performed, which showed the absence of the inferior vena cava and venous drainage through the hemiazygos vein to the superior vena cava. Ventricular pacing was not performed, due to the inability to insert the catheters.
Case 3Female patient, 21 years of age, was referred to the Electrophysiology Laboratory to undergo an electro-physiological study in April of 2012 to evaluate frequent episodes of tachycardia. The patient had a history of syncope, and complex congenital heart disease repair had been performed 19 years earlier (double outlet right ventricle, pulmonary stenosis, atrial septal defect); she underwent a permanent pacemaker implant in 2004. During the examination, a femoral venipuncture was performed, and a right-chamber catheterization was attempted with the insertion of a multipolar electrode catheter, which was unsuccessful due to agenesis of the inferior vena cava. Programmed ventricular pacing was performed with a pacemaker, which showed a sinus rhythm and a complete atrioventricular block that did not induce sustained ventricular tachycardia.
Case 4Female patient, 40 years of age, was referred to the Electrophysiology Laboratory for an electrophysiological study and ablation. A right femoral venipuncture was performed for catheter insertion. During catheter insertion, there was difficulty in advancing the cephalad catheter. An angiography of the venous system was performed, which showed an anomalous course of venous drainage into the lower half of the body, directed to the superior vena cava. The catheters were inserted into the heart cavity through the superior vena cava and positioned initially in the low right atrium, coronary sinus, and His bundle region. The atrial extrastimulation demonstrated dual atrioventricular nodal conduction and induced reproducible episodes of supraventricular tachycardia with concentric retrograde atrial activation. Slow nodal pathway ablation was performed successfully. However, postoperatively, the patient had deep vein thrombosis and pulmonary embolism of small intensity, with no associated symptoms. Anticoagulation was initiated, and the patient improved.
Case 5Female patient, 62 years of age, was referred to the Electrophysiology Laboratory for an electro-physiological study and ablation due to a palpitation complaint. Three diagnostic electrode catheters were introduced into the right chamber; however, catheter progression showed the presence of anomalous drainage into the lower half of the body to the superior vena cava. During the examination, posteroseptal accessory bundle was diagnosed, with successful bundle ablation.
DISCUSSIONVenous system development during embryogenesis is a complex process, during which the development, regression, and anastomosis of three pairs of veins (posterior cardinal, subcardinal, and supracardinal) form the inferior vena cava.2,3 If the originally paired structures are not joined between the sixth and eighth weeks of gestation, malformations can occur, such as a duplicated inferior vena cava, inferior vena cava agenesis, and the interruption of a certain segment (infrahepatic, prerenal, renal, or infrarenal), among others.3,4 Inferior vena cava malformations are present in 0.07% to 8.7% of the population3 and may be asymptomatic or associated with nonspecific symptoms. However, they may also be associated with an increased risk of deep venous thrombosis, which is present in 5% of young individuals who have deep venous thrombosis.5
Agenesis (also called atresia or aplasia) of the inferior vena cava is a rare malformation that occurs in 0.005% to 1% of the population. Its most common cause is dysgenesis during embryogenesis (due to the simultaneous occurrence of a defect in the venous system of the three embryonic segments), but it can also occur due to in utero or perinatal thrombosis (without embryological abnormalities).6 Since the patient shows no symptoms, the diagnosis of agenesis is often accidentally attained during abdominal surgery or radiological procedures;5 in these cases, collateral circulation develops from the lumbar, azygos, and hemiazygos systems, which compensate for the malformed lower vena cava function.7 However, in the event of insufficient collateralization, the slow blood flow in the lower limbs and pelvis leads to venous stasis and to an increased propensity for thrombosis.8 Thus, chronic venous insufficiency or deep vein thrombosis (especially in the iliac and femoral veins) may occur with a higher recurrence rate of thrombosis in these patients. Furthermore, comorbidities may be present, such as splenic abnormalities, intestinal malrotation, pulmonary dysgenesis, renal agenesis, dextrocardia, or other congenital heart diseases.5 Among the present patients, two had other congenital heart diseases, and one patient developed DVT followed by pulmonary thromboembolism.
Inferior vena cava agenesis should be suspected when young patients (up to 30 years-old) have idiopathic deep venous thrombosis, especially bilaterally in the iliac veins, and no risk factors (such as hypercoagulable states).8 However, it is important to remember that, in the absence of other anomalies, agenesis can be asymptomatic due to collateral venous system development.7
In case of diagnostic suspicion, imaging examinations should be performed. The best imaging methods to diagnose inferior vena cava abnormalities are computed tomography and magnetic resonance angiography, since the diagnosis of inferior vena cava abnormalities solely by ultrasonography is considered to be difficult.1,2,5 Treatment should focus on the prevention of complications, especially thrombosis. For this reason, several authors have recommended the use of anticoagulants.7 The patient must be advised to avoid other risk factors for thrombosis, such as the use of oral contraception and long periods of immobilization, as well as unnecessary surgical interventions.7
Patients referred for electrophysiological study or ablation may come to the electrophysiology laboratory without a prior diagnosis of inferior vena cava agenesis. Thus, the electrophysiologist should remember that these morphological alterations can occur, in order to avoid inadvertent complications of vascular access and catheter handling. For this purpose, other routes (e.g., the subclavian vein) may be used to access the venous system.
CONFLICT OF INTERESTThe authors declare that they have been granted sponsorship for scientific events and equipment for the Electrophysiology Laboratory from St. Jude Medical and Biotronik.