Young patient with a history of smoking, hypertension and use of illicit drugs (cannabis, cocaine and crack) was admitted with precordial pain after physical exercise within the previous two hours. Electrocardiogram demonstrated ST segment elevation in leads V1 to V4 and the patient was referred to cardiac catheterization, which showed total occlusion of the left anterior descending artery and a large amount of thrombi in the right coronary artery. The patient was treated with direct stenting in the left anterior descending artery and triple antiplatelet therapy with aspirin, clopidogrel and abciximab in combination with non-fractioned heparin for 24 hours. Angiography and intravascular ultrasound assessment after 48 hours demonstrated a complete resolution of thrombi in both coronary arteries.
Trombose Simultânea em Duas Artérias Coronárias Epicárdicas Durante Infarto Agudo do Miocárdio
Paciente jovem, com histórico de tabagismo, hipertensão ar terial e uso de drogas ilícitas (cannabis, cocaína e crack), foi admitido com dor precordial após atividade física, com cerca de duas horas de evolução. O eletrocardiograma demonstrou supradesnivelamento do segmento ST de V1 a V4, e o paciente foi encaminhado para cateterismo cardíaco, que evidenciou oclusão total da artéria descendente anterior e grande quantidade de trombos na coronária direita. Foi tratado com implante direto de stents na artéria descendente anterior e terapia antiplaquetária tripla com aspirina, clopidogrel e abciximab associada a heparina não-fracionada, mantidas por 24 horas. Reavaliações angiográfica e ultrassonográfica após 48 horas demonstraram resolução completa dos trombos em ambas as coronárias.
Acute myocardial infarction (AMI) with ST segment supra-unlevelling is more commonly caused by the rupture of the vulnerable atherosclerotic plaque with formation of thrombus and total occlusion of the vessel. In most of ases, a single culprit vessel is found. However, occlusion in multiple vessels, even though uncommon, can occur.1, 2 The exact mechanism of multiple occlusions is not well defined, and different mechanisms have have been proposed.
The rupture of vulnerable plaques may be the result of inflammation, catecholamine action, or increased sympathetic tone. In angiographic studies, the percentage of patients with acute myocardial infarction (AMI) who had thrombi in non-culprit lesions was 32.8%, 1 and this occurrence is associated with a higher number of adverse clinical outcomes. These studies defined angiographic thrombus as an intraluminal filling defect, as an abrupt vessel occlusion with contrast persistence observed in multiple projections, or as an occluded vessel with a convex margin that retains contrast and persists for several cardiac cycles. 3
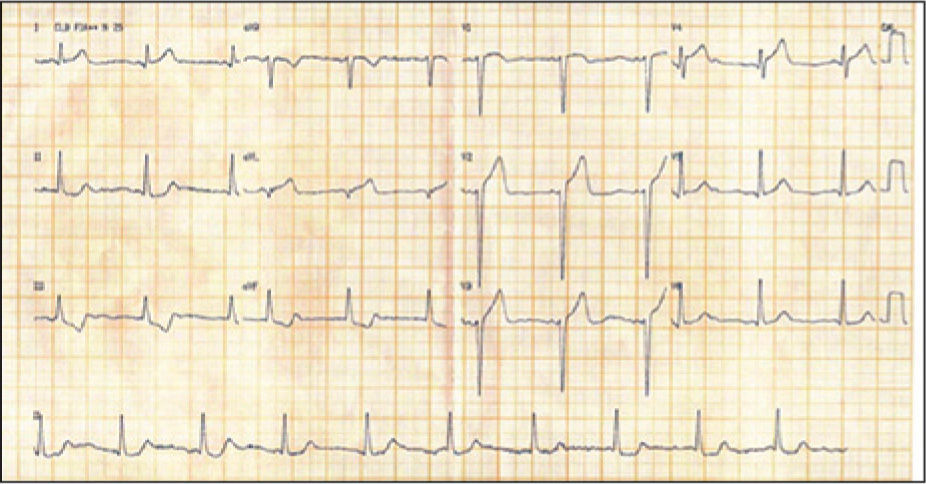
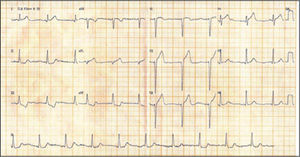
CASE REPORTA 34-year-old male patient with a long history of smoking, hypertension, and illicit drug use (cannabis, cocaine, and crack) was admitted to the emergency room due to chest pain of high intensity without irradiation, which began after physical activity and swea ting associated with a 2.5hours evolution. At physical examination, his blood pressure was 180/90mmHg, and the oxygen saturation, 94 % (FiO2: 21%), as well as normal heart and lung auscultation. The electrocardiogram (ECG) initially showed sinus rhythm, a ventricular rate of 60 beats per minute, and ST-segment elevation in leads V1 to V4 (Figure 1).
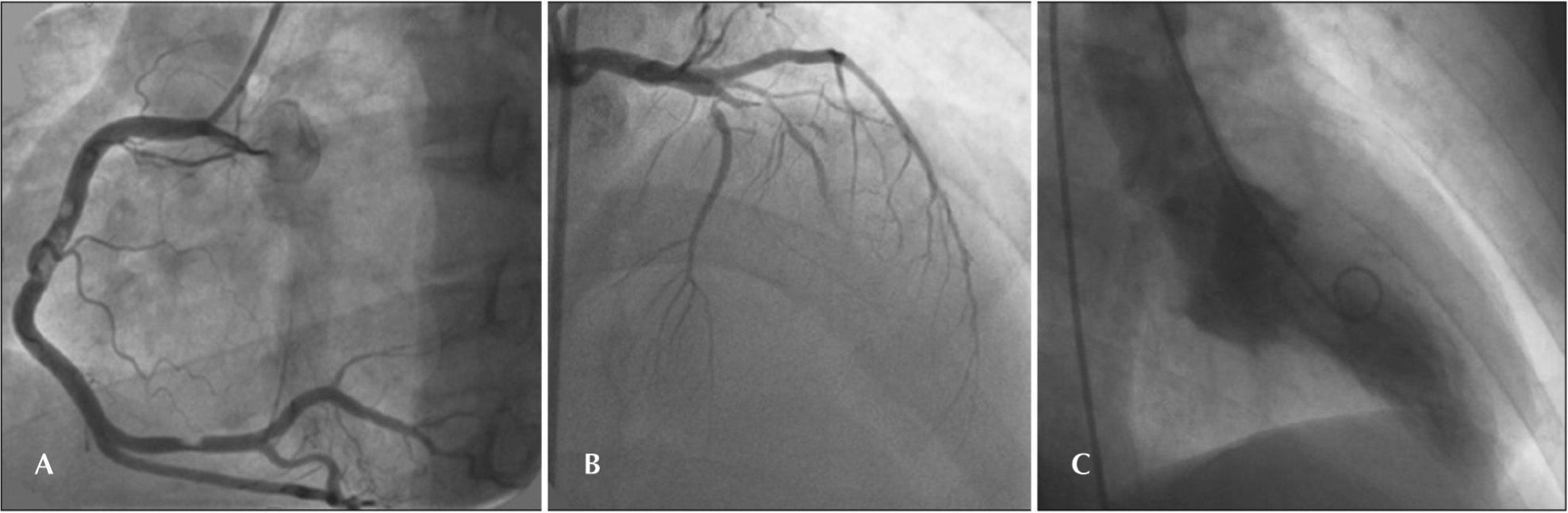
Due to the chest pain and ischaemic alterations on ECG, AMI with ST-segment elevation was diagnosed. 200mg of acetylsalicylic acid and 600mg of clopidogrel were administered, and then the patient was referred to the interventional cardiology laboratory to undergo primary percutaneous coronary intervention (PCI). Angiography showed right dominance, multiple thrombi in the right coronary artery, a left anterior descending artery (related to the AMI and occluded, with a Thrombolysis in Myocardial Infarction [TIMI] flow of 0), and a circumflex artery with no evidence of atherosclerotic lesions. Left ventriculography evidenced apical hypokinesia (Figure 2).
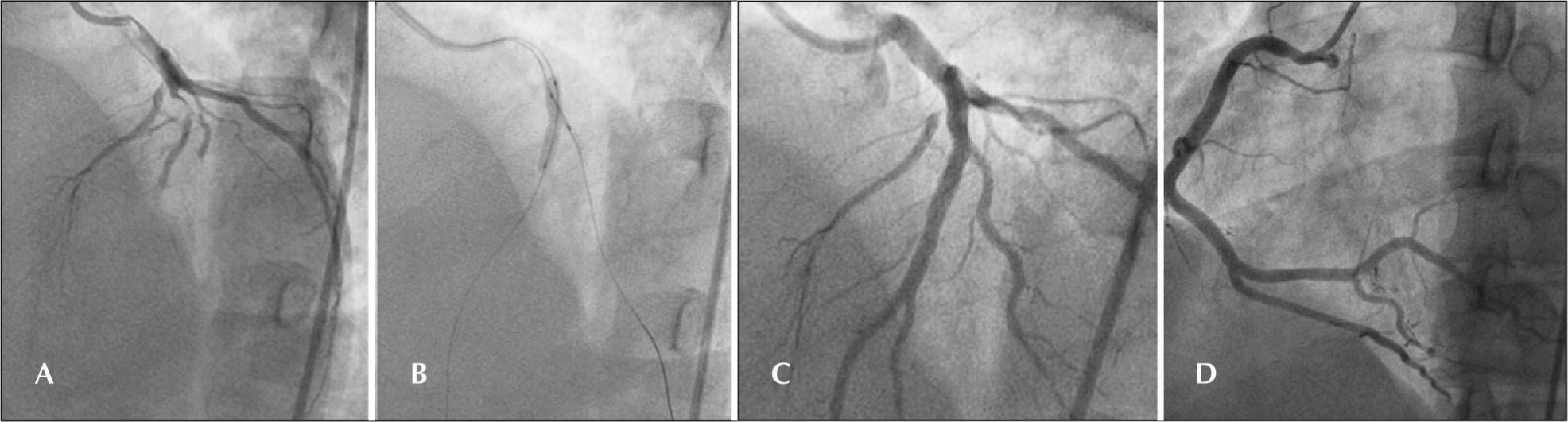
Since the right coronary artery lesions were not the culprits, it was decided to clinically follow them and treat the culprit lesion in the left anterior descending artery with conventional stenting. A 0.014-inch wire with moderate support was inserted from the anterior descending artery past the occlusion and was positioned in the distal portion, thus obtaining distal TIMI 3 flow. Another 0.014-inch floppy wire was positioned in the first diagonal branch. Direct stenting was performed with a 3.5×24mm bare-metal stent in the anterior descending artery with a final kissing balloon, using a complacent balloon in the first diagonal branch (Fig. 3 A, B, and C). The control angiography showed an image suggestive of dissection at the distal edge of the stent, and thus another 3.5×12mm stent was implanted distally, with an overlap of the stent borders.
The patient received unfractionated heparin and a loading dose of glycoprotein IIb/IIIa inhibitors (abciximab) during the PCI. After the procedure, triple antiplatelet therapy with acetylsalicylic acid, clopidogrel, and abciximab was maintained (associated with unfractionated heparin for 24 hours at the coronary care unit).
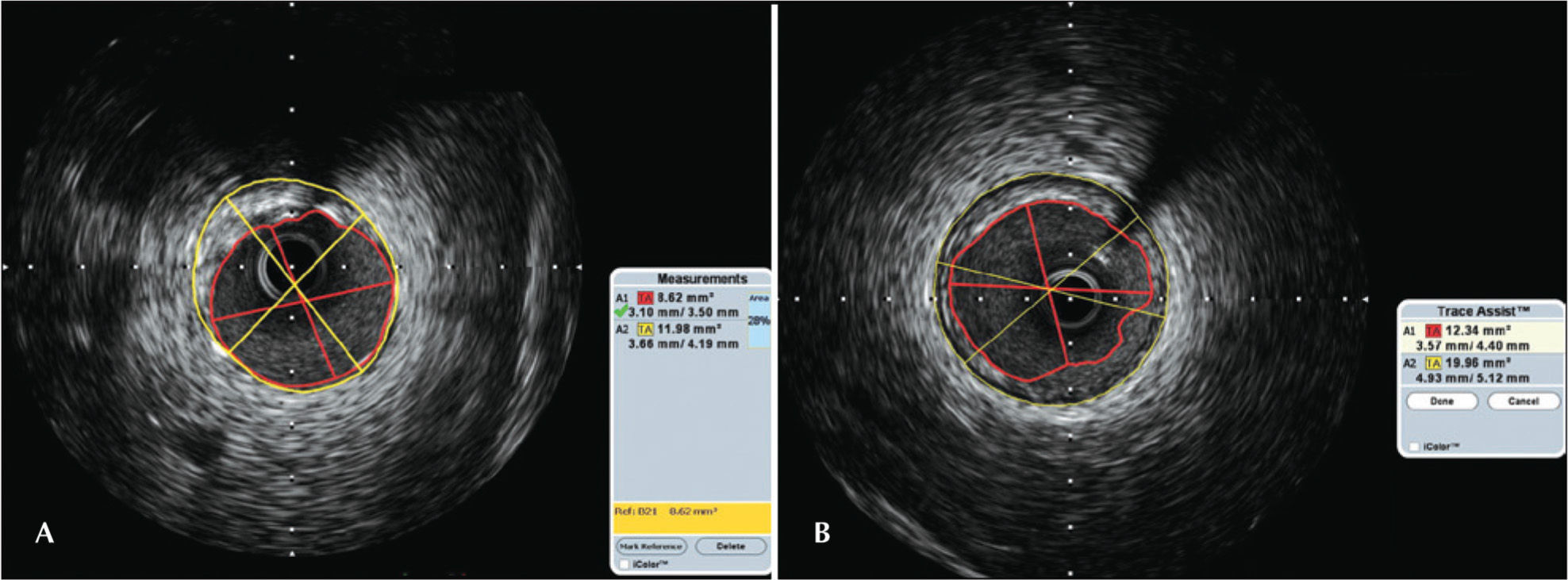
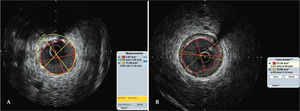
After 48 hours, a new angiography demonstrated the complete resolution of thrombi in the right coronary artery (Figure 3 D). Intracoronary ultrasound (IVUS) was performed in the anterior descending and in the right coronary arteries to assess stent implantation (Figure 4 A and B). IVUS showed a minimal luminal area of 7.2mm 2 in the anterior descending artery, and a new balloon dilatation was performed to obtain a final area of 8.58mm 2. Although IVUS is not the best method for thrombi visualization, thrombi were not observed in these territories. However, incipient atherosclerotic plaques were found in the proximal and middle thirds of the right coronary artery, and were more pronounced in the middle third of the anterior descending artery.
In A, anterior descending artery assessed using intracoronary ultrasound. In B, right coronary artery assessed using intracoronary ultrasound. of ischaemia recorded one the ECG must be treated first. In cases where the ECG is not clear, the culprit artery responsible for the larger at-risk myocardial territory should be treated first. 8
In necropsies of patients who died from AMI, Burke and Virmani 1 observed that 25% to 50% of these patients had multiple coronary thromboses. Using coronary angiography, Goldstein et al. 2 found simultaneous coronary thrombi in patients with AMI.
Many predisposing conditions for multiple coronary thromboses have been suggested, such as cocaine use, hypercoagulable state, coronary spasm, high concentrations of catecholamines, diabetes mellitus, and essential thrombocytosis. 3
Multiple thromboses in coronary arteries are extremely rare in current clinical practice. Pathological studies have demonstrated their presence in 10% of the patients who died from AMI. 4 Patients with multiple thromboses tend to have more severe clinical manifestations in up to 50% of the cases described in the literature. 5
PCI with aggressive adjunct drug therapy is very important in cases of multiple occlusions because cardiogenic shock is common in these high-risk patients. 6 In the present patient, however, it was decided to perform a PCI in the culprit artery. Glycoprotein IIb/ IIIa inhibitors, dual antiplatelet therapy, and unfractionated heparin were administered for 24 hours after the procedure. The high thrombotic burden found in both arteries may be explained by the hypercoagulable state generated by the illicit drug use. Additionally, IVUS showed atherosclerotic plaques in the left anterior descending and right coronary arteries that were more pronounced in the culprit vessel. The priority of revascularization during primary PCI in AMI patients should be guided using the ECG. 7 In general, the area of ischaemia recorded one the ECG must be treated first. In cases where the ECG is not clear, the culprit artery responsible for the larger at-risk myocardial territoryshould be treated first.8
Multiple thromboses in the coronary arteries of patients with AMI and ST-segment elevation are uncommon. In the literature, cases of simultaneous occlusion in coronary arteries occur in isolated cases; thus, it becomes difficult to define treatment strategies in these scenarios. Revascularization within the shortest possible time is obviously imperative; these patients require reperfusion therapy and aggressive adjunct drug therapy, and mechanical support may be necessary to improve clinical prognosis.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.