Stroke remains the leading cause of morbidity and mortality in Brazil. Epidemiological data suggest that 10% to 30% of all strokes are due to atherosclerotic carotid artery disease and 8% due to vertebral artery disease. Endovascular treatment of extracranial lesions is an alternative to endarterectomy. We evaluated the results and predictors of adverse events in patients undergoing carotid and vertebral artery stenting.
MethodsAsymptomatic patients with lesion > 70% or symptomatic patients with lesions > 50% in carotid arteries and symptomatic patients with lesion > 70% in vertebral arteries were included. We evaluated the primary endpoint, defined as the composite incidence of death (procedural or non-procedural), major stroke, minor stroke or myocardial infarction (MI).
ResultsTwo hundred and twenty-four interventions with stenting were performed in 199 consecutive patients with a prevalence of males (73.9%), 69.8±9.9years of age and 37.7% were diabetics. Symptomatic patients represented about two thirds of the cases and the most commonly treated lesions were de novo lesions (96.4%). The left (46%) and right (44.6%) internal carotid arteries were the most commonly approached vessels. Composite primary endpoint was observed in 5% of the patients, procedure-related mortality in 1%, non-procedure related mortality in 1%, minor stroke in 1.5% and MI in 1.5%. Patients with a history of coronary artery disease had a 4-fold probability of presenting the primary endpoint [odds ratio (OR) 4.32, 95% confidence interval (CI 95%) 1.09-17.21); P=0.038].
ConclusionsIn our study we obtained a high success rate and had a low rate of adverse events, demonstrating the safety and efficacy of percutaneous stent implantation in the carotid and vertebral arteries.
Implante Percutâneo de Stent em Artérias Carótidas e Vertebrais: Dados do REMAT (Registro Madre Teresa)
IntroduçãoO acidente vascular encefálico (AVE) é a principal causa de morbidade e mortalidade no Brasil. Entre 10% e 30% dos AVEs estão associados à doença carotídea e 8%, à artéria vertebral. O tratamento endovascular das lesões extracranianas é alternativa à endarterectomia. Analisamos os resultados e avaliamos os preditores de eventos adversos em pacientes submetidos a angioplastia carotídea e vertebral com implante de stents.
MétodosIncluídos assintomáticos com lesão > 70% ou sintomáticos com lesão > 50% em artérias carótidas e sintomáticos com lesão > 70% em artérias vertebrais. Avaliamos desfecho primário, definido como a incidência combinada de morte relacionada ou não ao procedimento, AVE maior, AVE menor ou infarto agudo do miocárdio (IAM).
ResultadosRealizadas 224 intervenções com implante de stents em 199 pacientes consecutivos, com predomínio do sexo masculino (73,9%), idade de 69,8±9,9 anos e 37,7% eram diabéticos. Pacientes sintomáticos representaram cerca de dois terços dos casos e as lesões mais tratadas foram as lesões de novo (96,4%). As artérias carótidas internas esquerda (46%) e direita (44,6%) foram os vasos mais abordados. Desfecho combinado primário ocorreu em 5%, mortalidade relacionada ao procedimento em 1%, mortalidade não-relacionada ao procedimento em 1%, AVE menor em 1,5% e IAM em 1,5%. Pacientes com antecedente de doença arterial coronária mostraram chance de apresentar desfecho primário 4 vezes maior [odds ratio (OR) 4,32, intervalo de confiança de 95% (IC 95%) 1,09-17,21; P=0,038].
ConclusõesEm nosso estudo obtivemos alto índice de sucesso e baixa ocorrência de eventos adversos, que demonstram a segurança e a eficácia do implante percutâneo de stent em artérias carótidas e vertebrais.
Stroke remains the third leading cause of death in industrialized countries, and the leading cause of adult disability.1 In the United States, it is estimated that 795,000 strokes occur each year, generating direct and indirect costs of treating stroke victims of approximately US$ 68.9 billion annually.1,2 In Brazil, it is estimated that 250,000 strokes occur per year, representing the main cause of morbidity and mortality in the population.3
Extracranial cerebrovascular disease is an important cause of stroke and transient ischemic attack (TIA).4,5 Epidemiological data suggest that 10% to 30% of strokes are due to carotid artery disease and 8% are associated with vertebral artery territory. The most common cause is atherosclerosis, but fibromuscular dysplasia, media cystic necrosis, arteritis, and dissection are also present. Stroke and TIA may appear as a consequence of several mechanisms originating in the atherosclerotic plaque, such as thrombus embolism formation on the atherosclerotic plaque, flow reduction in a stenotic or occlusive plaque, atheroembolism, and subintimal dissection or hematoma.1
Endovascular treatment of carotid and vertebral artery obstructions is a constantly evolving technique and an alternative to endarterectomy in the prevention of strokes. In recent years, with the development of catheters, stents, and cerebral protection devices, expansion of the indications for angioplasty in the carotid and vertebral territories has been sought, in order to minimize procedure-related risks. The evidence supporting stenting in carotid arteriesvs endarterectomy come from studies such as Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Trial (SAPPHIRE),6,7 and Carotid Revascularization Endarterectomy vs. Stenting Trial (CREST),8,9 demonstrating results comparable to those of surgical treatment. However, in relation to angioplasty in vertebral arteries, the evidence is scarce. The only randomized study that compared endovascular treatment vs. clinical treatment in vertebral arteries1 was the Carotid And Vertebral Artery Transluminal Angioplasty Study (CAVATAS) study,10 which showed no significant difference in the outcomes between the two patient groups.
This study aimed to evaluate the results and determine predictors of adverse clinical events in patients undergoing carotid and vertebral angioplasty with stenting in this service.
METHODSPatientsBetween January of 2006 and January of 2012, 225 interventions were performed with 226 stent implantations in the carotid or vertebral arteries, in 200 consecutive patients admitted to the Hemodynamics and Interventional Cardiology Service of Hospital Madre Teresa (Belo Horizonte, MG, Brazil). Patients of both genders were enrolled, aged > 18 years, symptomatic in the last six months, with lesions > 50% in ipsilateral carotid artery, asymptomatic with lesions > 70% in the carotid artery, or symptomatic in the last six months with lesions > 70% in the vertebral artery. A patient diagnosed with pseudoaneurysm of the internal left carotid artery, in which a coated stent was used, was excluded from the analysis to ensure sample homogeneity, there by yielding a final sample of 224 interventions in 199 patients.
This study is in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the institution.
Angioplasty procedure and protocolAll procedures were performed electively at the Hemodynamics Laboratory of the Hospital Madre Teresa. All patients received acetylsalicylic acid at a dose of 100mg/day and clopidogrel at a dose of 75mg/ day, starting at least four days before the procedure. Acetylsalicylic acid was maintained indefinitely, and clopidogrel was maintained for at least 30 days after the intervention.
The interventions were performed by femoral access route in all patients under local anaesthesia with the Seldinger technique, using 6F or 7F sheaths. Anticoagulation was attained with administration of 100 U/kg of unfractionated heparin, aiming to achieve activated clotting time between 250–300 seconds. The use of sedatives was avoided in order to prevent impairment of patient neurological assessment during the procedure. The guide-catheters used in most procedures were JR4 or AL1, and long hydrophilic sheaths were used.
Stent implantations in the carotid and vertebral arteries was performed in accordance with the current guidelines, by experienced interventional cardiologists proficient in non-coronary procedures, board-certified by the Brazilian Society of Hemodynamics and Interventional Cardiology (Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista – SBHCI). In all carotid procedures, a distal embolic protection filter was employed. Pre-dilation of carotid lesions was employed only in sub-occlusive and calcified lesions. After positioning and releasing the endoprosthesis, intravenous atropine was administered at a dose of 0.5mg to 1mg, and post-dilation was performed in most cases with balloon inflation for complete stent expansion. The following stents were used: Precise, BX Velocity/Sonic, Presillion, and Palmaz – Genesis (Cordis Endovascular – Miami Lakes, United States); Wallstent, Express, and Liberté (Boston Scientific – Natick,USA); Protégé (ev3 Endovascular Inc. – Plymouth, United States); Multi-link Ultra and Xact (Abbott Vascular – Abbott Park, USA); and Dynamic (Biotronik Corporation – Berlin, Germany).
For the angioplasty of vertebral arteries, a similar technique to that employed in the coronary arteries was used, by performing pre-dilation in complex lesions and coronary or peripheral stent implantation, depending on the artery calibre.
Final control angiography and brain circulation angiography were performed in all patients. After confirmation of the angiographic success, the procedure was closed and the patient was referred to the intensive care unit (ICU). In the absence of complications, the patients were released to the infirmary or apartment, were discharged on the following day, and were instructed to return within a month to undergo a consultation with the attending physician and/or Hemodynamics Service for clinical follow-up.
Outcomes and definitionsNeurological events were defined as: TIA, any neurological deficit reversed in the first 24 hours postprocedure that did not result in residual neurological damage, including amaurosis fugax; minor stroke, new neurological event that resulted in a mild decrease of neurological function, not disabling or with minimal neurological sequelae; and major stroke, with established neurological damage, disabling, and/or classified as 9 points on the National Institutes of Health Stroke Scale (NIHSS).4,9,12
The diagnosis of acute MI was based on elevation of markers of myocardial necrosis (CK-MB or troponin) two-fold higher than the normal limit, requested when the patient showed signs and symptoms consistent with myocardial ischemia or ischemic alterations on electrocardiography, routinely performed in the ICU.9,13
Angiographic success was defined as residual lesion < 30% by quantitative angiography in the absence of thrombi or dissections. Procedural success was defined as angiographic success in the absence of TIA, minor or major stroke or death related to the procedure.
A primary clinical outcome was evaluated in the follow-up period, defined as the composite incidence of death related or not to the procedure, major stroke, minor stroke, or acute MI. A secondary clinical outcome, defined as the composite occurrence of TIA/amaurosis fugax, significant bleeding that required blood transfusion, or bradycardia requiring a temporary pacemaker, was also evaluated.
Statistical AnalysisData tabulation was performed in Microsoft Excel, and STATA software, version 12.0, was used for the statistical analysis.
The descriptive results were obtained using frequencies and percentages for categorical variables and measures of central tendency (means and medians) and measures of dispersion (standard deviations) for the quantitative variables.
Univariate analysis was performed to verify the association of clinical and angiographic variables with primary and secondary outcomes. All variables with Pvalue < 0.20 in the univariate analysis were included in the initial model of the multivariate analysis using logistic regression with the forward method, that is, with the inclusion of variables in the model one by one, from the most significant to the least significant. The variables with a level of significance < 5% were maintained in the final model. The Hosmer-Lemeshow test was used to verify the adequacy of the model.
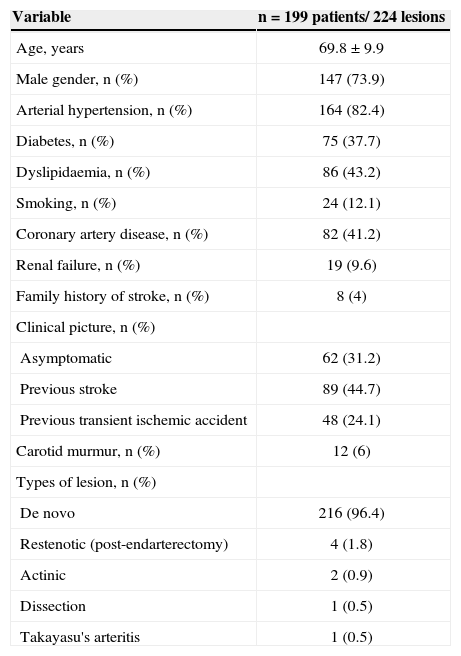
RESULTSRegarding the clinical characteristics, the present study had a predominantly male population (73.9%), aged 38 to 90 years, with a mean age of 69.8±9.9years, 37.7% diabetics, and 9.6% with renal failure. On admission, approximately two-thirds (68.8%) of patients were symptomatic, 44.7% with stroke and 24.1% with previous TIA, and the minority had carotid murmur (6%). The most often treated lesions were de novo lesions (96.4%), as well as post-endarterectomy restenotic lesions, actinic lesions, post-trauma dissection, and Takayasu’s arteritis (Table 1).
Clinical characteristics
| Variable | n=199 patients/ 224 lesions |
|---|---|
| Age, years | 69.8±9.9 |
| Male gender, n (%) | 147 (73.9) |
| Arterial hypertension, n (%) | 164 (82.4) |
| Diabetes, n (%) | 75 (37.7) |
| Dyslipidaemia, n (%) | 86 (43.2) |
| Smoking, n (%) | 24 (12.1) |
| Coronary artery disease, n (%) | 82 (41.2) |
| Renal failure, n (%) | 19 (9.6) |
| Family history of stroke, n (%) | 8 (4) |
| Clinical picture, n (%) | |
| Asymptomatic | 62 (31.2) |
| Previous stroke | 89 (44.7) |
| Previous transient ischemic accident | 48 (24.1) |
| Carotid murmur, n (%) | 12 (6) |
| Types of lesion, n (%) | |
| De novo | 216 (96.4) |
| Restenotic (post-endarterectomy) | 4 (1.8) |
| Actinic | 2 (0.9) |
| Dissection | 1 (0.5) |
| Takayasu's arteritis | 1 (0.5) |
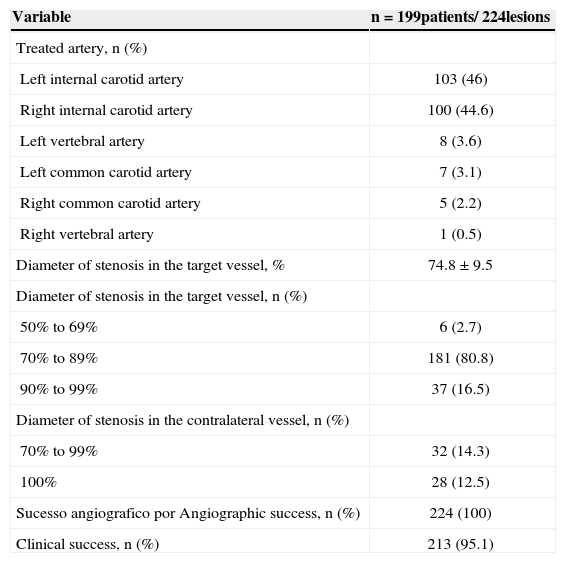
The degree of stenosis of the target lesion was, on average, 74.8%±9.5%; lesions of 70% to 89% were the most often treated, corresponding to 80.8% of the patients. In addition, 26.8% of the patients had lesion > 70% in a vessel contralateral to the target vessel, 12.5% of which were total occlusions. The left internal carotid artery was the most often treated vessel (46%), followed by the right internal carotid artery (44.6%), the left vertebral artery (3.6%), the left common carotid artery (3.1%), the right common carotid artery (2.2%), and the right vertebral artery (0.5%). Angiographic success was attained in all procedures, and the clinical success rate was 95.1% (Table 2).
Angiographic and procedural characteristics
| Variable | n=199patients/ 224lesions |
|---|---|
| Treated artery, n (%) | |
| Left internal carotid artery | 103 (46) |
| Right internal carotid artery | 100 (44.6) |
| Left vertebral artery | 8 (3.6) |
| Left common carotid artery | 7 (3.1) |
| Right common carotid artery | 5 (2.2) |
| Right vertebral artery | 1 (0.5) |
| Diameter of stenosis in the target vessel, % | 74.8±9.5 |
| Diameter of stenosis in the target vessel, n (%) | |
| 50% to 69% | 6 (2.7) |
| 70% to 89% | 181 (80.8) |
| 90% to 99% | 37 (16.5) |
| Diameter of stenosis in the contralateral vessel, n (%) | |
| 70% to 99% | 32 (14.3) |
| 100% | 28 (12.5) |
| Sucesso angiografico por Angiographic success, n (%) | 224 (100) |
| Clinical success, n (%) | 213 (95.1) |
A total of 225 stents were used in the 224 interventions. Precise stent (n=106) was chosen for most of the stenting procedures, followed by Wall stent (n=100), and Liberté stent (n=8), used in the vertebral arteries. The other endoprostheses used were the Express (n=3),Presillion (n=2), BX Velocity/Sonic (n=1),Palmaz-Genesis (n=1), Protegé (n=1),Multi-link Ultra (n=1), Xact (n=1), and Dynamic (n=1) stents. In one of the patients, it was necessary to implant two stents during the same intervention, a Wall stent overlapping a Precise stent in the right internal carotid artery to treat a segmental lesion.
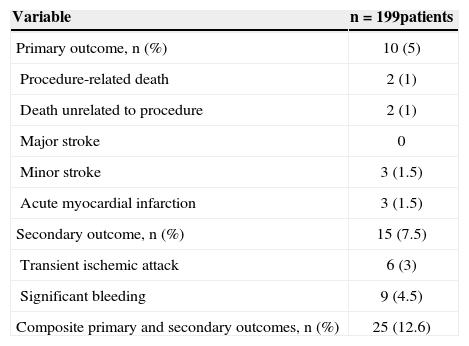
The follow-up period was, on average, 2.2±7.5months, with 70.1% of patients followed for up to one month, 20.5%for up to six months, and 9.4% for 12 months or more. The incidence of the primary composite outcome was 5%, with procedure-related mortality of 1%, mortality unrelated to procedure of 1%, minor stroke of 1.5%, and MI of 1.5%. There were no major strokes. TIA/amaurosis fugax and significant bleeding requiring blood transfusion occurred in 3% and 4.5% of cases, respectively. The combined rate of primary and secondary outcomes was 12.6%. No complications were observed in femoral artery access route requiring surgical intervention. There was no symptomatic or prolonged bradycardia requiring temporary pacemaker (Table 3).
Adverse clinical events
| Variable | n=199patients |
|---|---|
| Primary outcome, n (%) | 10 (5) |
| Procedure-related death | 2 (1) |
| Death unrelated to procedure | 2 (1) |
| Major stroke | 0 |
| Minor stroke | 3 (1.5) |
| Acute myocardial infarction | 3 (1.5) |
| Secondary outcome, n (%) | 15 (7.5) |
| Transient ischemic attack | 6 (3) |
| Significant bleeding | 9 (4.5) |
| Composite primary and secondary outcomes, n (%) | 25 (12.6) |
Multivariate analysis elucidates independent predictors of adverse events (Table 4). The procedures with patients who had coronary artery disease demonstrated a four-fold higher chance of presenting primary outcomes (odds ratio [OR]: 4.32; 95% confidence interval [95% CI]: 1.09 to 17.21; P=0.038). In addition, female gender (OR: 3.74; 95% CI: 1.13 to 12.35; P=0.03), family history of stroke (OR: 8.04; 95% CI: 1.20 to 53.83; P=0.032) and renal failure (OR: 9.53; 95% CI: 2.54 to 35.63; P=0.001) were predictors of the secondary outcome. In procedures whose patients had family history of stroke (OR: 5.50; 95% CI: 1.15 to 26.36; P=0.033), and renal failure (OR: 6.16; 95% CI: 2.11 to 17.97; P=0.001) composite primary or secondary outcomes were more likely to occur. This registry showed no association between the presence or absence of pre-procedure symptoms in relation to the primary or secondary outcomes.
Independent predictors of primary and secondary outcomes
| Events | Primary outcomesa(n=10) | Secondary outcomesb(n=15) | Primary and secondary outcomesc(n=25) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Female gender | N/D | N/D | N/D | 3.74 | 1.13-12.35 | 0.03 | N/D | N/D | N/D |
| Coronary artery disease | 4.32 | 1.09-17.21 | 0.038 | N/D | N/D | N/D | N/D | N/D | N/D |
| Family history of stroke | N/D | N/D | N/D | 8.04 | 1.20-53.83 | 0.032 | 5.50 | 1.15-26.36 | 0.033 |
| Renal failure | N/D | N/D | N/D | 9.53 | 2.54-35.63 | 0.001 | 6.16 | 2.11-17.97 | 0.001 |
Hosmer-Lemeshow test:
The data presented in this cross-sectional, observational, and clinical study disclosed relevant aspects on the profile and outcome of patients undergoing percutaneous stent implantation in the carotid and vertebral arteries in a philanthropic tertiary care center, a reference in the treatment of high-complexity cardiovascular diseases in the metropolitan region of Belo Horizonte, state of Minas Gerais, Brazil.
It is was observed that the information concerning the clinical characteristics of the assessed population, including age, gender, and traditional risk factors for atherosclerosis, were consistent with those observed in other studies.6−10 A high proportion of symptomatic patients (68.8%) and with target vessel lesion > 70% at admission, which was the expected profile of candidates for the intervention, was also observed.6,14,15 Regarding the approach of special patient populations, such as patients with post-endarterectomy restenosis, with lesions after cervical irradiation, or inflammatory arteritis, the intervention remains a challenge, since such lesions have intense fibrosis, which can hinder stent expansion. Series of cases have reported greater difficulty for endarterectomy, with higher safety of percutaneous stent implantation in this group of patients despite a higher rate of restenosis.1,16 The use of stent in dissection lesions is reserved for symptomatic patients who do not respond toanticoagulation.1 The present angiographic data are analogous to previously published works.6−10,17,18 In the CREST trial,8,9 however, the rate of occlusion of vessel contralateral to the target vessel was 2.7%, whereas in the present study the proportion of total occlusion of the contralateral vessel was 12.5%.
Regarding the outcome analysis, there was a high clinical success rate (95.1%) and a low percentage of adverse clinical events, a fact probably attributed to the expertise of the interventional cardiologists with cerebrovascular interventions, since the learning curve acquired with the volume of procedures decisively influences the results of percutaneous intervention in the cerebrovascular territory.6−9,19 It is worth noting the low rates of adverse clinical events during follow-up in relation to other studies.6−9,20 In the present, the percentage of primary outcomes (death/stroke/acute MI) was 5%. In the periprocedural period of the SAPPHIRE6 and CREST8,7,9 trials, the incidence of primary adverse events in patients undergoing angioplasty was 4.4% and 5.2%, respectively.
Since stroke is the leading cause of mortality in Brazil and a large number of stroke cases are attributed to vertebral and carotid atherosclerotic disease, its treatment can reduce the disabling sequelae and risk of death, offering greater expectation and better quality of life for the patient. From the social policies stand point, the timely intervention during the course of carotid and vertebral artery stenosis would represent the rescue of a portion of the population that uses primary and secondary health care services, as well as reducing costs for the tax payers, given that atherosclerosis in the cerebrovascular territory is part of a continuum, in which the progress of the disease is directly related to the population’s aging process.1 It is estimated that, in 2025, Brazil will have a contingent of more than 30 million individuals older than 60 years of age, constituting the seventh largest elderly population in the world, which represents21 thousands of stroke victims that will require medical assistance.
Considering the magnitude of the problem in Brazil, little attention is given from the authorities to public policies for stroke prevention and health system organisation. The rate of stroke in Brazilis higher than that in developed countries and the countries of South America; it is the fourth highest rate among all Latin American countries.22,23 Epidemiological data, however, suggest a tendency to the decrease in the stroke mortality rate in Brazil in recent years.23 The possible causes of the reduction in stroke mortality rate are related to the control of risk factors, improvement of the population’s socioeconomic status, development of diagnostic methods, and incorporation of high-tech procedures, such as cerebrovascular angioplasty by the Brazilian Unified Health System (Sistema Único de Saúde).
The endovascular treatment of obstructions in the carotid and vertebral arteries is a technique undergoing constant improvement, and it is an alternative to endarterectomy in the prevention of brain ischemic events. Although the evidence regarding the angioplasty in vertebral arteries is still scarce, in recent years, with the development of catheters, stents, and devices for cerebral protection, the indications of angioplasty in the carotid territory have expanded, minimising the procedure-related risks. The evidence that supports carotid angioplasty vs. Endarterectomy is based on the results of large registries and randomized clinical trials, such as SAPPHIRE6,7 and CREST,8,9 which allowed for the consolidation of percutaneous stenting in the carotid arteries as a class I recommendation, level of evidence B, for symptomatic patients with stenosis≥50% to 99%, and as class IIb recommendation, level of evidence B, in a symptomatic patients with stenosis≥70% to 99%, according to the latest guideline from the United States, developed by a multidisciplinary task force.1
Study limitationsThe study limitations are the retrospective analysis of data, the fact that it was conducted in a single center, and the short period of follow-up after hospital discharge. The multivariate analysis detected the probable independent predictors of adverse events; however, due to the amplitude of the confidence intervals, a consequence of the low frequency of the analysed events, little can be affirmed about the strength of the association between the analysed variables and the outcomes.
CONCLUSIONSThis retrospective registry showed a high success rate and low incidence of adverse events in patients undergoing percutaneous stent implantation in the carotid and vertebral arteries. The present results indicate that the procedure can be executed safely and effectively when properly indicated, using the adequate technique and performed by qualified interventional professionals in tertiary centers.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
The authors would like to thank Professor Dr. Viviane Santuari Parisotto Marino, for her support and presence in the writing of this manuscript.