The type of cerebral protection used during carotid stenting in the elderly is controversial. Our objective was to evaluate the results of proximal and distal cerebral embolic protection devices (EPDs), in patients>70 years through diffusion-weighted magnetic resonance imaging (DW-MRI).
MethodsBetween 2008 and 2011, 60 patients with indication for carotid stenting were randomized to EPD with Mo.Ma® or Angioguard®, of which 26 patients were>70 years of age. Results of DW-MRI performed before and 48 hours after the procedure were evaluated by an independent neurologist blinded to the type of EPD used. New ischemic lesions, their localization and size were analyzed.
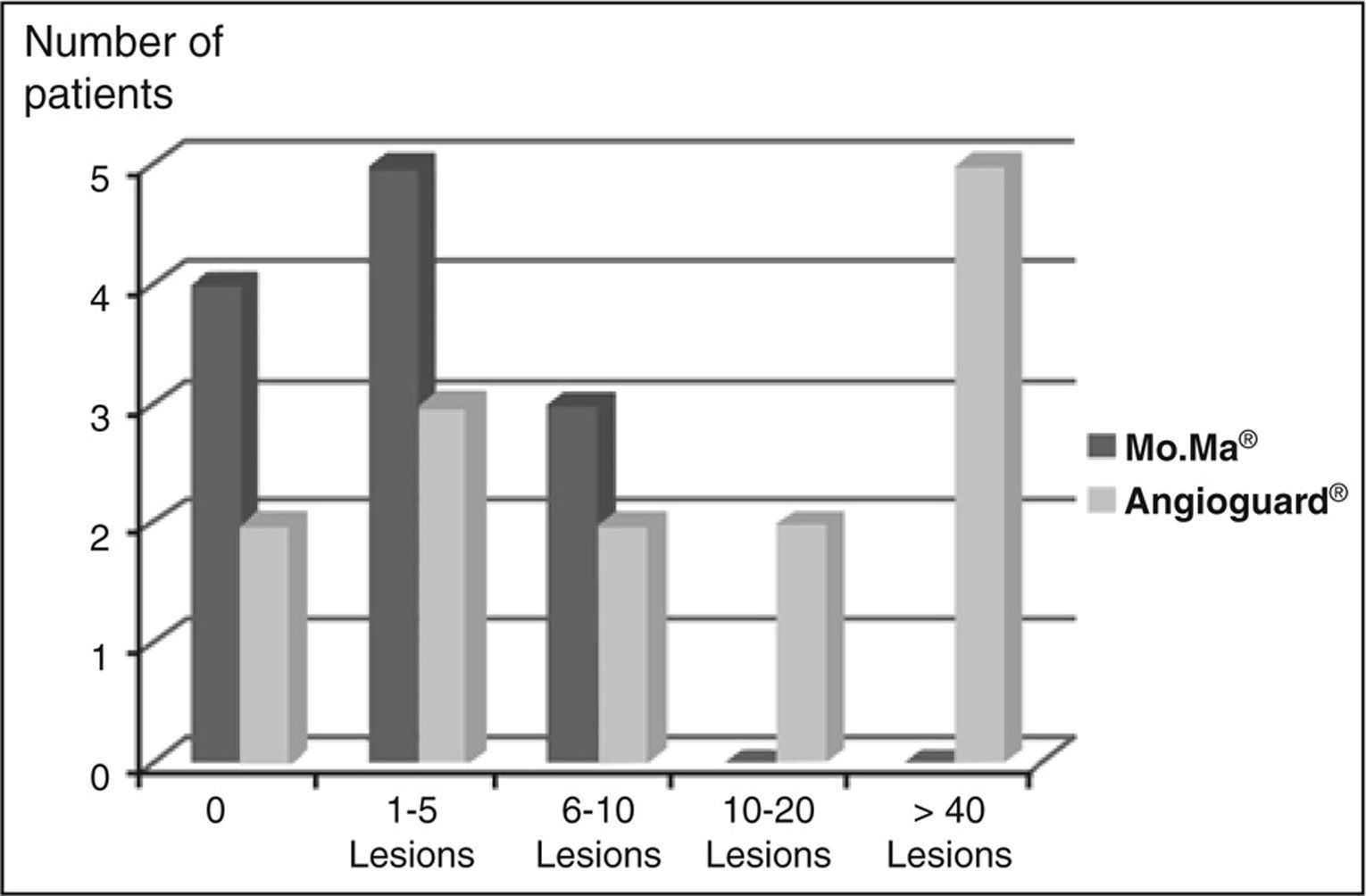
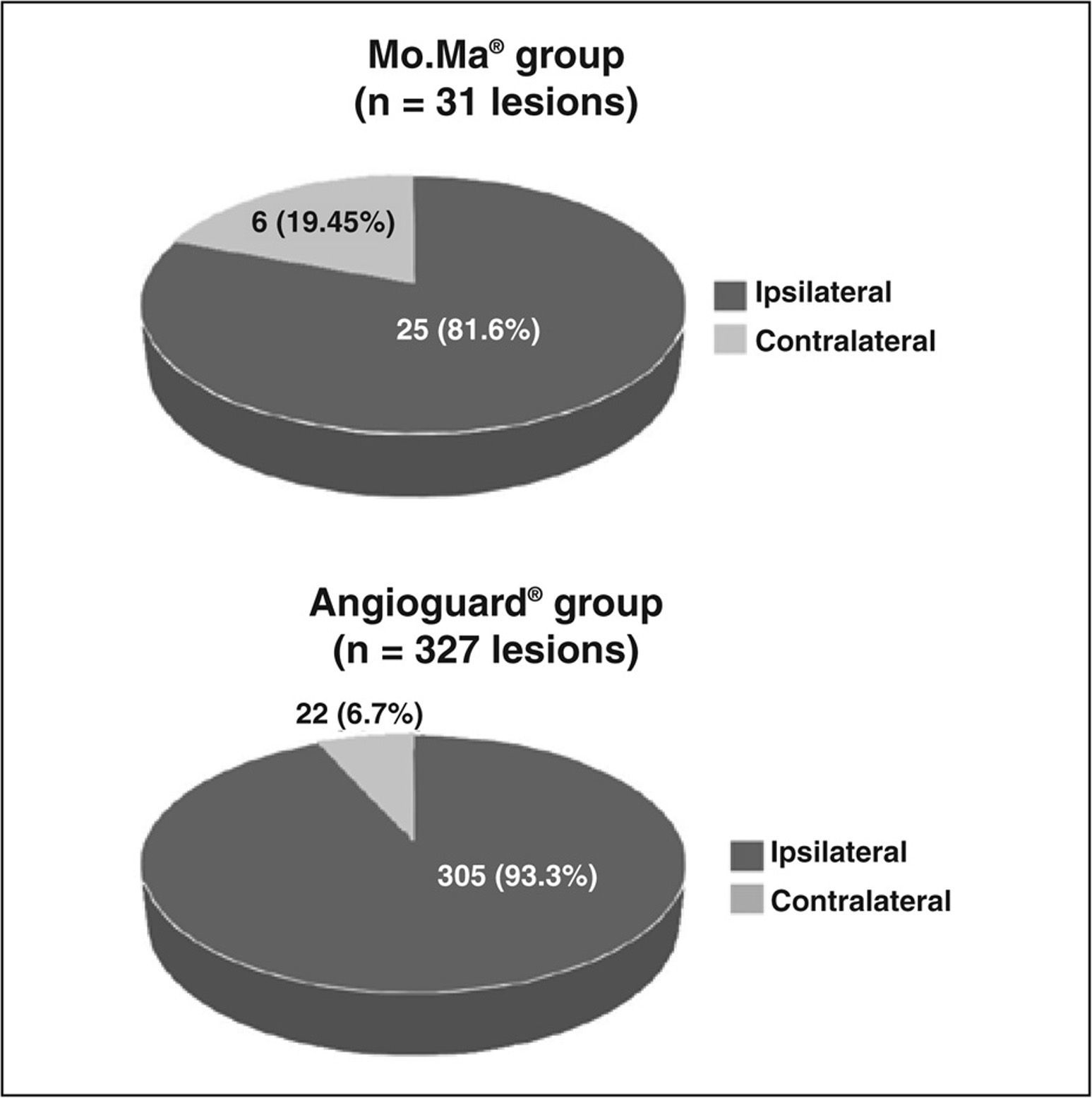
ResultsNew cerebral ischemic lesions were found in 8/12 (66.7%) patients in the Mo.Ma® group and 12/14 (85.7%) patients in the Angioguard® group (P=0.37). The vast majority of the lesions (> 90%) were ipsilateral to the treated artery in both groups and the size of the lesions was<0.5cm in most cases. The number of lesions per patient was lower with the Mo.Ma® device (median [variation]: 3 [1 to 8] lesions vs 15 [2 to 76] lesions; P<0.001). All of the patients with more than 40 lesions were in the Angioguard® group.
ConclusionsDespite the use of EPDs (proximal or distal), new ischemic lesions were observed in both groups in elderly patients. A proportionately larger number of patients with Angioguard® had new ischemic lesions when compared to those with Mo.Ma®. The Mo.Ma® device seems to decrease the number of lesions per patient.
Proteção Cerebral em Pacientes Idososdurante Implante de Stent Carotídeo
IntroduçãoO tipo de proteção cerebral utilizado durante o implante de stent carotídeo é controverso em idosos. Nosso objetivo foi avaliar os resultados dos dispositivos de proteção embólica cerebral (PEC), proximal e distal, em pacientes>70 anos de idade, por meio da ressonância magnética ponderada de difusão (RM-PD).
MétodosEntre 2008 e 2011, 60 pacientes com indicação de stent carotídeo foram randomizados para PEC com Mo.Ma® ou Angioguard®, dos quais 26 tinham>70 anos de idade. Os resultados da RMPD realizada antes e 48 horas após o procedimento foram avaliados por neurologista independente e cego para o tipo de PEC utilizado. Foram analisados o número de novos focos isquêmicos, sua localização e o tamanho.
ResultadosNovos focos isquêmicos cerebrais foram encontrados em 8/12 (66,7%) pacientes do grupo Mo.Ma® e em 12/14 (85,7%) pacientes do grupo Angioguard® (P=0,37). A maioria das lesões (> 90%) era ipsilateral à artéria tratada em ambos os grupos, e o tamanho das lesões foi<0,5cm na maioria dos casos. O número de lesões por paciente foi menor com o dispositivo Mo.Ma® (mediana [variação]: 3 [1 a 8] lesões vs. 15 [2 a 76] lesões; P<0,001). Todos os pacientes que tiveram mais de 40 lesões pertenciam ao grupo Angioguard®.
ConclusõesMesmo utilizando PEC (proximal ou distal), novas lesões isquêmicas foram observadas em ambos os grupos em pacientes idosos. Proporcionalmente maior número de pacientes com Angioguard® teve novos focos isquêmicos se comparados aos pacientes do grupo Mo.Ma®. O dispositivo de PEC Mo.Ma® parece diminuir o número de lesões por paciente.
Extracranial carotid disease has surgical endarterectomy as the standard treatment. The percutaneous treatment with stent implantation1 has emerged as a less invasive alternative for high-surgical risk patients.
The microemboli generated during the percutaneous procedure are the biggest challenge to be overcome. Theron et al.2 were the first to report the use of cerebral embolic protection devices (EPDs) in clinical practice. They used a balloon occlusion system in the internal carotid, distal to the lesion; at the end of the procedure, when analysing the aspirated material, they found particles with potential risk of embolisation of intracranial vessels.
Currently, there are two strategies for cerebral embolic protection: proximal EPDs, which produce endovascular clamping of blood flow through expanded balloons in the common carotid artery and the external carotid artery, and that cause interruption or reversal of blood flow in the internal carotid, allowing for the capture of particles of all sizes through aspiration of the blood column; and distal EPDs, constituted by filters with pores that capture particles>100μm, positioned distally to the internal carotid artery lesion. The latter are simpler to use and are the preferred choice of interventionists.
This study aimed to analyse the behavior of two different types of EPDs in elderly patients (> 70 years), evaluating the findings of the diffusion-weighted magnetic resonance imaging (DW-MRI) before and 48 hours after carotid stent implantation.
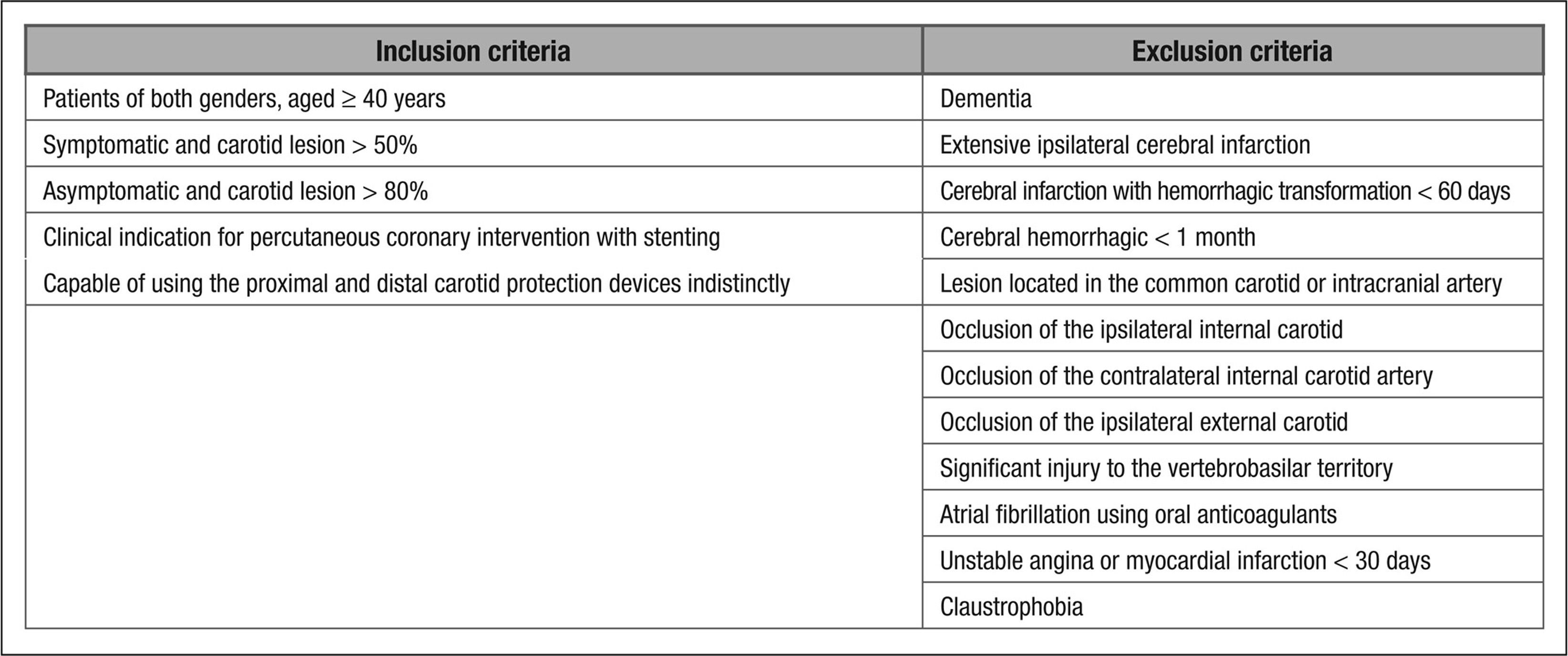
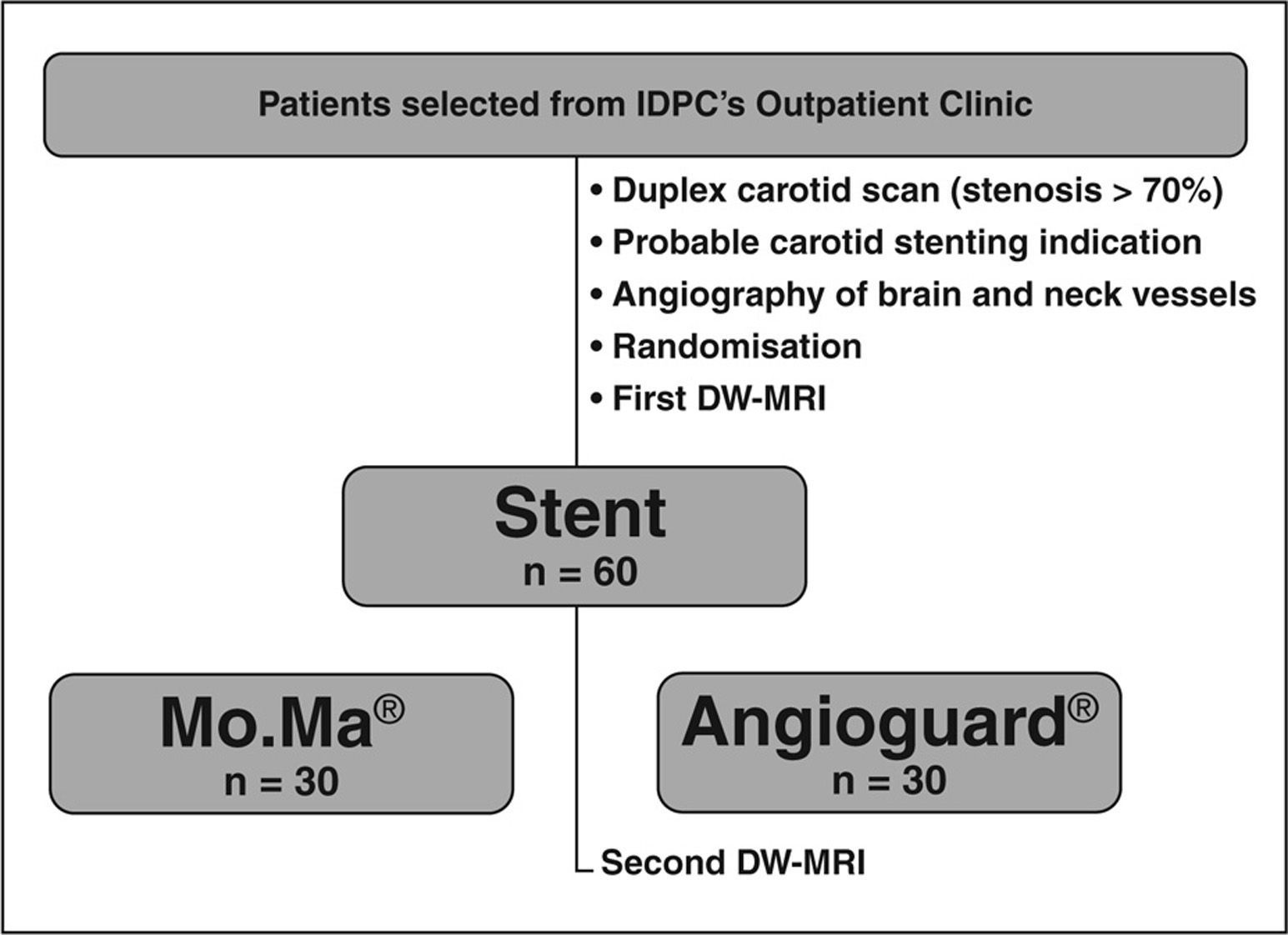
METHODSThis was a prospective, single-center, randomized study that included patients with carotid stenosis, whether symptomatic or asymptomatic, candidates for stenting and capable of indistinctly receiving the proximal EPD Mo.Ma® (Invatec Corporation-Brescia, Italy) or distal EPD Angioguard® (Cordis Endovascular – Miami Lakes, United States) (Figure 1).
All patients received the nitinol carotid stent PRECISE® (Cordis Endovascular – Miami Lakes, United States), which is an open-cell self-expanding stent, and requires a 6F release system.
DW-MRI was used to detect hyperacute brain microinfarcts caused by microparticles released during the endovascular procedure, with the assessment of the number, size, and location of new ischemic foci. DWMRI images were obtained in a 3.0 Tesla equipment (Excite HD; GE Medical Systems – Milwaukee, USA) with an eight-channel head coil. The DW-MRI was performed before and 48 hours after the percutaneous procedure. The results were evaluated by an independent neurologist blinded to the type of EPD used. Patients were followed-up for a period of at least one year.
Randomisation of patients to the Mo.Ma® and Angioguard® groups was accomplished electronically using the Complex Samples module of SPSS software. To ensure balance in relation to the number of patients in each group, randomisation was performed in groups of six (three for the Mo.Ma® group and three for the Angioguard® group).
All the fundamental requirements of Resolutions no. 196/96, 251/97, and 292/99, on guidelines and regulating norms in research involving human subjects, by the National Health Council/National Board of Research Ethics/Brazilian Health Surveillance Agency (Agência Nacional de Vigilância Sanitária – ANVISA) were met, as well as the Good Practices in Clinical Research of ICH – GCP.
Objectives and definitionsThe main objective of this study was to compare, by DW-MRI, the incidence and extension of ischemic events after carotid stenting in patients>70 years of age, using two types of EPD (proximal vs. distal).
The following definitions were adopted:
- −
Transient ischemic accident: defined as a temporary alteration in blood supply to a brain area, resulting in sudden and brief (less than 24 hours, typically less than one hour) decrease of brain functions. Symptoms vary depending on the affected area, and include visual alterations, speech alterations, and localized sensory and motor deficiencies.
- −
Stroke: new neurological deficit with focal symptoms and signs consistent with focal ischemic lasting over 24 hours. Minor stroke causes neurological deficit that completely resolves within 30 days. Major stroke causes neurological deficit that does not completely resolve within 30 days.
- −
Procedural success: when there was technical success (capacity to use the cerebral EPD and stent implantation with a residual lesion≤30 %), associated with clinical success (no cerebrovascular and cardiovascular events during the procedure).
- −
Myocardial infarction: symptoms compatible with myocardial ischemic associated with ischemic electrocardiographic alterations and increase of at least twofold the normal value of myocardial necrosis markers.
In the statistical analysis, qualitative data were summarized as absolute and relative frequencies (percentages) and compared with Student’s t-test. Quantitative data were expressed as means and standard deviations and compared using Fisher’s exact test.
A value of P<0.05 was considered significant. The statistical softwares used were SPSS for Windows, version 19.0, and R (R Core Team), version 16.0.
RESULTSBetween July of 2008 and July of 2011, 60 patients were randomized (Figure 2). During the trial period, over 250 procedures with carotid stent implantation were performed at the institution, and 67 patients met the inclusion criteria and were randomized. During the trial, two patients withdrew their consent and five others were excluded because, during the procedure, the anatomical characteristics of the lesions made them more suitable for one of the cerebral EPDs, violating the inclusion criteria. Of the 60 patients included, 26 (43.3%) were aged>70 years and were the subject of this analysis.
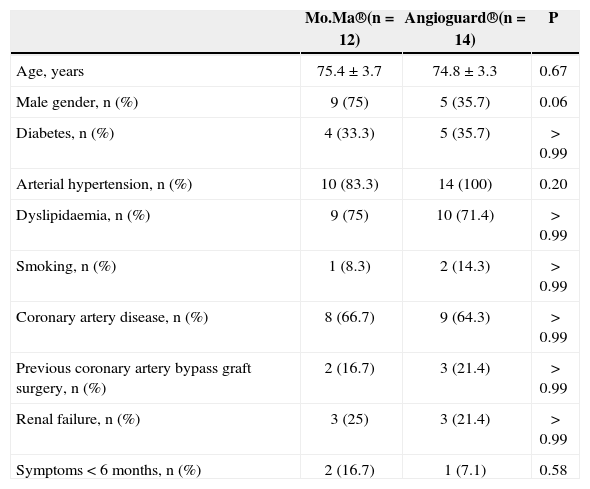
Twelve patients were allocated to the Mo.Ma® group and 14 to the Angioguard® group, with a mean age of 75±3.5years and similar clinical characteristics (Table 1).
Clinical characteristics
| Mo.Ma®(n=12) | Angioguard®(n=14) | P | |
|---|---|---|---|
| Age, years | 75.4±3.7 | 74.8±3.3 | 0.67 |
| Male gender, n (%) | 9 (75) | 5 (35.7) | 0.06 |
| Diabetes, n (%) | 4 (33.3) | 5 (35.7) | > 0.99 |
| Arterial hypertension, n (%) | 10 (83.3) | 14 (100) | 0.20 |
| Dyslipidaemia, n (%) | 9 (75) | 10 (71.4) | > 0.99 |
| Smoking, n (%) | 1 (8.3) | 2 (14.3) | > 0.99 |
| Coronary artery disease, n (%) | 8 (66.7) | 9 (64.3) | > 0.99 |
| Previous coronary artery bypass graft surgery, n (%) | 2 (16.7) | 3 (21.4) | > 0.99 |
| Renal failure, n (%) | 3 (25) | 3 (21.4) | > 0.99 |
| Symptoms<6 months, n (%) | 2 (16.7) | 1 (7.1) | 0.58 |
Successful stent implantation was attained in all patients with the EPD indicated at the randomisation, without crossover. The mean procedure time was similar between the groups (29.5±10.3min vs. 24.2±10.4minutes; P=0.21).
New cerebral ischemic foci were found in 8/12 (66.7%) patients in Mo.Ma® group and in 12 /14 (85.7%) patients in Angioguard® group (P=0.37). The number of lesions per patient was lower with Mo.Ma® device (median [range]: 3 lesions [1 to 8] vs. 15 lesions [2–76]; P<0.001). All five patients with>40 lesions were from the Angioguard® group (Figure 3).
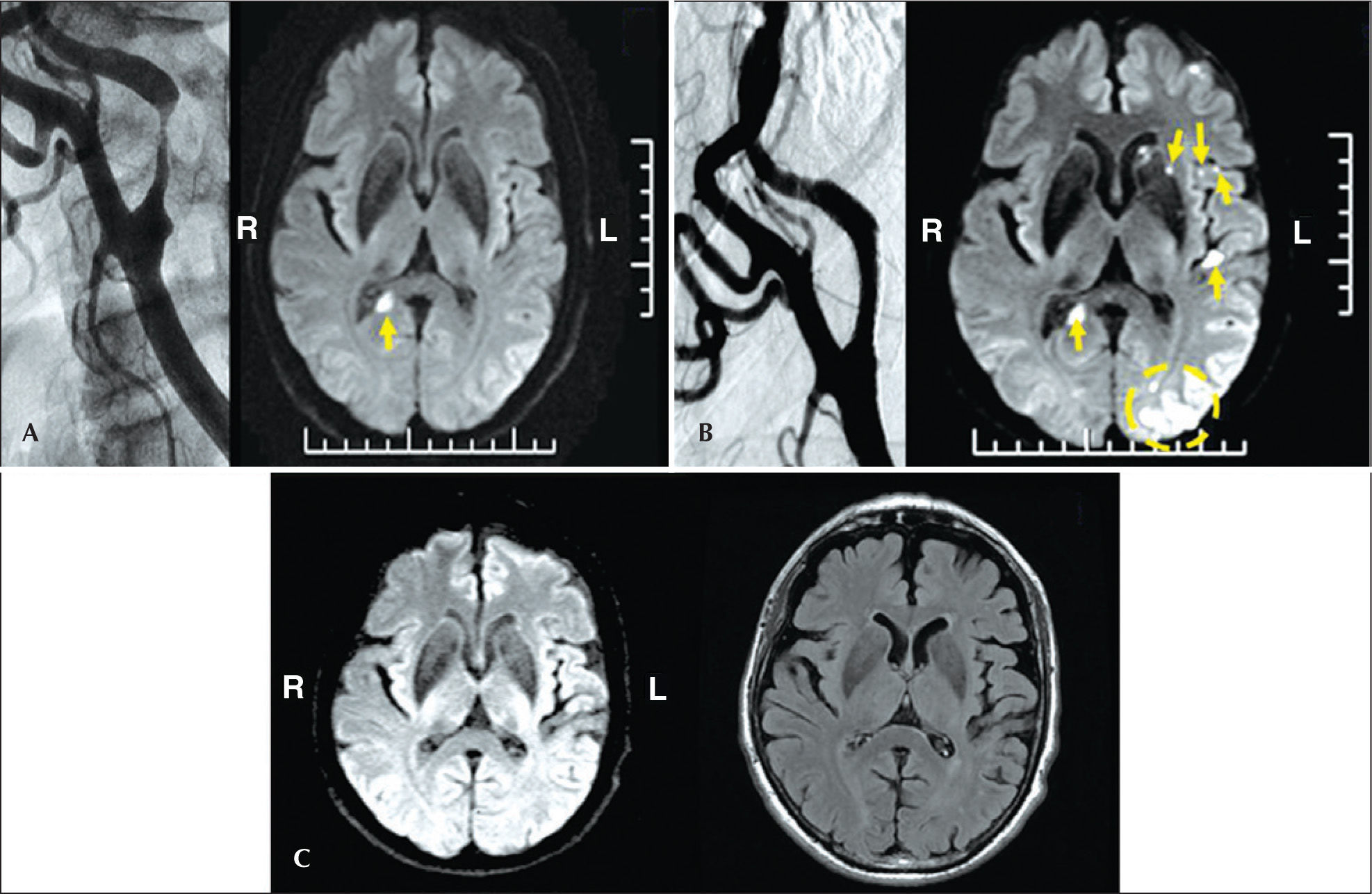
The lesions were mostly ipsilateral to the artery treated in both groups. Figure 4 shows the anatomical distribution of cerebral microlesions according to the type of cerebral protection. The lesions were mostly small (< 0.5cm in over 90% of them).
Procedural success was 96.2%, with one patient presenting stroke during the intervention, which showed complete recovery in less than 30 days (minor stroke). A subsequent late DW-MRI performed in this patient showed the disappearance of lesions (Figure 5). At the follow-up of at least one year, no death or major stroke occurred in the two groups of patients.
– In A, pre-intervention: on the left, angiography showing a 90% lesion in the left carotid; on the right, diffusion imaging showing old white matter infarct in the occipital lobe (arrow). In B, post-intervention: on the left, angiography showing final result after stenting; on the right, diffusion imaging showing hyperacute ipsilateral microinfarcts (arrows). In C, late follow-up (one year): on the left, diffusion image showing resolution of post-procedure alterations and on the right, flair image confirming the findings. R, right; L, left.
The main findings of the present study were that the number of brain microlesions per patient at the DW-MRI was significantly lower in the group of elderly patients treated with Mo.Ma® when compared to the group treated with Angioguard®, and that the carotid stent implantation with two types of EPD is feasible in elderly patients and effective in terms of prevention of major clinical events.
The underlying causes of the lower incidence of cerebral microembolisation at the DW-MRI in elderly patients who used proximal cerebral protection are not fully understood, and may include a combination of factors. Distal EPD needs to overcome the lesion before the protection starts working effectively. The main determinants of increased risk of stroke in these patients are the complexity of the aortic arch (higher proportion of type III aortic arch),3 type of treated lesion, 4,5 degree of calcification,6 and excessive angulation and tortuosity of the approached carotid.7
The study by Brott et al.8 in 2,502 patients, demonstrated no significant difference between carotid stenting with distal filter EPD and endarterectomy during the four years of follow-up regarding the primary outcome of death, infarction, and stroke (7.2% vs. 6.8%; P=0.51). Moreover, no difference was observed regarding events between genders (male/female) and presence of symptoms (symptomatic/asymptomatic). Regarding age, an increasing association was observed between increased risk of stroke and older age, when distal EPD was used.
Risk factors for use of distal EPD were studied in registries and reviews; 9 age and diabetes were systematically identified, as well as gender, smoking status, and the afore mentioned anatomical risk factors. However, it is still unknown whether the same factors for distal EPD must be considered for proximal EDP. When analysing the studies addressing the use of proximal EPD, it was observed that in 2,397 patients,10 there was a composite primary outcome of death, total stroke, or myocardial infarction at 30 days of 2.5 %, with incidence of death in 0.40%, of stroke in 1.71%, and myocardial infarction in 0.02%. The only independent predictors of events (death, myocardial infarction, and stroke) were age and diabetes. Of note, in all subgroups, including octogenarian patients, the incidence of events was<2.6%.
Finally, with the introduction of proximal EPD, rates of adverse events greatly decreased, with high-risk patients showing the greatest benefit (elderly included). To date, there have been no randomized studies comparing carotid stenting with proximal cerebral protection and endarterectomy.
Study limitationsThe main limitations of this study refer to the small number of cases, due to the difficulty to find patients who could indistinctly use both EDPs, and the absence of angiographic characterisation of the population, which could unbalance the groups, despite the randomization.
The small number of patients restricts the extrapolation of the present conclusions, which are limited to the displayed scenario and the EPD devices used, and thus cannot be extended to other commercially available devices.
CONCLUSIONSPatients>70 years of age appear to have better results when undergoing carotid stenting with proximal EPD (Mo.Ma®), showing fewer microinfarcts when compared to those using distal EPD (Angioguard®). Further studies with clinical outcomes are recommended to confirm the present findings.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.