In acute coronary syndrome, the use of multiple anticoagulant and antiplatelet drugs contributes to the risk of bleeding, including vascular access site bleeding, particularly in female patients. The use of the radial artery as a vascular access was shown to reduce the incidence of complications.
MethodsRetrospective study including patients with acute coronary syndrome undergoing percutaneous coronary intervention by radial access, divided by gender. Patient profiles were analyzed, as well as the early and late outcomes.
ResultsPatients with acute coronary syndrome (n=188) were submitted to percutaneous coronary intervention using the radial access, and 34.6% of them were female. Clinical variables were similar between groups, except for the EuroSCORE and creatinine clearance, characterizing a slightly more complex profile in women. There were no differences in angiographic and procedure-related characteristics for most of the variables. Two-thirds of the patients had multivessel disease and non-C type lesions were the most treated. In-hospital death rates (5.8% vs. 5.5%; p=0.81), myocardial infarction (1.4% vs. 0; p=0.76) and emergency percutaneous intervention (1.4% vs. 0; p=0.76) were similar between groups; severe bleeding was rare (1.4% vs. 0; p=0.76). In the late evolution, major adverse cardiac events (18.3% vs. 17.1%; p=0.67) were similar.
ConclusionsThe transradial approach for percutaneous coronary intervention proved to be as effective in women as in men in the setting of acute coronary syndrome, with a high success rate and similar clinical outcomes. It also proved to be safe, since bleeding events were rare in the evaluated population.
Comparação dos Resultados da IntervençãoCoronária Percutânea por Via Radial na Síndrome Coronariana Aguda Entre Mulheres e Homens
IntroduçãoNa síndrome coronariana aguda, o uso de múltiplos fármacos anticoagulantes e antiagregantes plaquetários contribui para o risco de sangramentos, incluindo aqueles da via de acesso vascular, particularmente no sexo feminino. O uso da artéria radial como via de acesso vascular mostrou reduzir aincidência de complicações.
MétodosEstudo retrospectivo, que incluiu pacientes com síndrome coronariana aguda submetidosa intervenções coronárias percutâneas por via radial, divididas de acordo com o genero. Foram analisados os perfisdos pacientes, assim como as evoluções clínicas iniciais e tardias.
ResultadosPacientes com síndrome coronariana aguda (n=188) foram submetidos à intervenção coronária percutâneapor acesso radial, sendo 34,6% mulheres. Os grupos não mostraram diferenças em relação às variáveis clínicas, com exceção do EuroSCORE e o clearance de creatinina, que caracterizaram um perfil um pouco mais complexo nas mulheres. Em relação às características angiográficas e do procedimento, não foram observadas diferenças em relação à maioria das variáveis. Dois terços dos pacientes tinham acometimento multiarterial, e as lesões tipo não C foram asmais tratadas. As taxas hospitalares de óbito (5,8% vs. 5,5%; p=0,81), infarto do miocárdio (1,4% vs. 0; p=0,76) e intervenção coronária percutânea de urgência (1,4% vs. 0; p=0,76) foram semelhantes entre os grupos; os sangramentos graves foram raros (1,4% vs. 0; p=0,76). Na evolução tardia, os eventos cardíacos maiores (18,3% vs. 17,1%; p=0,67) foram semelhantes.
ConclusõesIntervenção coronária percutânea por via radial mostrou-se tão efetiva nas mulheres quanto nos homens, no cenário da síndrome coronariana aguda, com alta taxa de sucesso e evolução clínica similar. Mostrou também ser segura, uma vez que os sangramentos foram eventos raros na população avaliada.
Despite the many advances made in the treatment of acute coronary syndrome (ACS) in recent decades, this condition remains a major cause of mortality, and the application of therapies in accordance with the scientific evidence in clinical practice remains heterogeneous. This problem is particularly true for specific populations, such as women, for whom disparity in treatment has been observed since the initial trials.1
The need for complete anticoagulation and of antiaggregation with multiple drugs, including glycoprotein IIb/IIIa inhibitors, contributes to the risk of hemorrhagic complications with the percutaneous approach to ACS. Bleeding from the site of vascular access is an important cause of morbidity and mortality after the procedure, particularly in women.2 In percutaneous coronary interventions (PCI) performed electively or as an urgency procedure, the use of the radial artery rather than the femoral artery as the vascular access route has shown similar success rates, and a reduction in the number of puncture site complications.3,4 However, published studies assessing the impact of female gender on the results of PCI performed by radial route in ACS patients are still scarce.
This study aimed to evaluate the clinical, angiographic, and procedural profiles, as well as the early and late evolution of women and men with ACS treated by PCI using the radial approach.
METHODSStudy populationThis was a retrospective study with consecutive inclusion of patients with ACS with and without ST-segment elevation, treated by transradial approach. Patients with cardiogenic shock who had radial pulse present at the time of PCI were also included in the series.
ProcedureThe radial artery puncture was performed with the patient holding the right upper limb extended at his/her side; hand in the supine position, under local anesthesia performed with 2–3mL of 2% lidocaine. For the artery puncture, a JELCO ® 20g was used and, after the puncture, 5–7F sheaths with length of 11cm, specific for radial artery, were inserted. After the procedure, the arterial sheath was removed in-room, without heparin reversal. A gauze and tape compressive dressing was applied. Typically, the pressure dressing is removed two hours after the procedure.
All patients were treated with bare-metal stents and received a loading dose of 300mg acetylsalicylic acid and 600mg of clopidogrel, followed by a maintenance daily dose of 100mg and 75mg, respectively, as well as unfractionated heparin (70 to 100 U/kg IV) during the procedure.
The follow-up was conducted after hospital discharge at 1, 3, 6, and 12 months, and yearly thereafter, via clinical visitor phone contact.
DefinitionsThe lesion morphology, according to the classification by the Society for Cardiovascular Angiography and Interventions (SCAI), was defined as: type I, patent non-C type lesion; type II, patent C type lesion; type III, occluded non-C type lesion; and type IV, occluded C type lesion. Angiographic success was defined as the achievement of a stenosis diameter < 30% with final flow of 3 according to the Thrombolysis in Myocardial Infarction (TIMI) criteria.
Bleeding was defined according to TIMI criteria:5 minimum, for any clinical sign of bleeding associated with a drop in hemoglobin < 3g/dL; minor, for any clinical sign of bleeding associated with a drop in hemoglobin of 3–5g/dL; and major, for intracranial hemorrhage, a signal of clinically significant bleeding associated with a drop in hemoglobin > 5g/dL, or fatal bleeding. The Bleeding Academic Research Consortium (BARC) criteria were also used,6 namely: type 0 – no bleeding; type 1 – small bleeding not requiring medical care or hospitalization; type 2 – any sign of bleeding that does not fit into types 3, 4, or 5, but with at least one of the following criteria: non-surgical medical intervention, need for hospitalization or increased level of care, need for clinical evaluation; type 3A – bleeding associated with a drop in hemoglobin of 3–5g/dL, or bleeding requiring blood transfusion; type 3B – bleeding associated a drop in hemoglobin > 5g/dL, cardiac tamponade, bleeding requiring surgical treatment for its control (except dental/nasal/skin/hemorrhoids) or the use of vasoactive drugs; type 3C – intracranial bleeding (except micro-bleeding or hemorrhagic transformation, distinct subcategories of bleeding confirmed by autopsy, imaging procedures or peritoneal lavage, or intraocular bleeding that compromises the vision); type 4 – bleeding related to coronary artery bypass graft (CABG); and type 5 – fatal bleeding.
Major adverse cardiac events (MACE) were defined as a combination of cardiac death, nonfatal acute myocardial infarction (AMI), and need for target vessel CABG. Stent thrombosis was classified as acute, subacute, late, and very late, according to the Academic Research Consortium (ARC) criteria.6
Statistical analysisContinuous variables were expressed as mean and standard deviation, and comparisons were performed using Student’s t-test for independent samples. Qualitative variables were expressed as numbers and percentages and compared by the chi-squared or Fisher’s exact test, when appropriate.
The SPSS 12.0 for Windows was used to perform statistical calculations. P-values < 0.05 were considered significant.
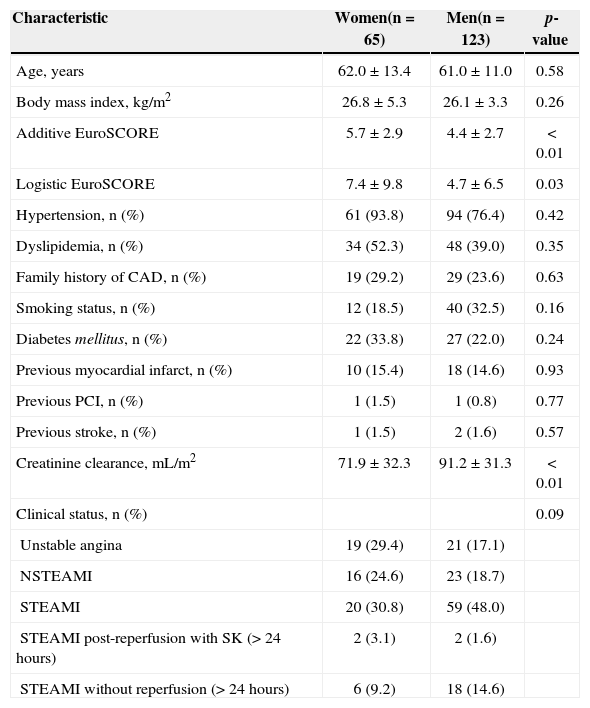
RESULTSFrom June 2011 to December 2013, 188 patients with ACS underwent PCI via the transradial access; 65 (34.6%) were female. The mean ages were 62.0±13.4years and 61.0±11.0years (p=0.58), and the incidences of diabetes were 33.8% vs. 22.0% (p=0.24), respectively, for women and men. The groups did not differ with respect to most clinical variables, except for the logistic and additive EuroSCOREs creatinine clearance (71.9±32.3mL/kg/min vs. 91.2±31.3mL/ kg/min; p < 0.01), which characterized a slightly more complex profile in female patients (Table 1).
Basal clinical characteristics
| Characteristic | Women(n=65) | Men(n=123) | p-value |
|---|---|---|---|
| Age, years | 62.0±13.4 | 61.0±11.0 | 0.58 |
| Body mass index, kg/m2 | 26.8±5.3 | 26.1±3.3 | 0.26 |
| Additive EuroSCORE | 5.7±2.9 | 4.4±2.7 | < 0.01 |
| Logistic EuroSCORE | 7.4±9.8 | 4.7±6.5 | 0.03 |
| Hypertension, n (%) | 61 (93.8) | 94 (76.4) | 0.42 |
| Dyslipidemia, n (%) | 34 (52.3) | 48 (39.0) | 0.35 |
| Family history of CAD, n (%) | 19 (29.2) | 29 (23.6) | 0.63 |
| Smoking status, n (%) | 12 (18.5) | 40 (32.5) | 0.16 |
| Diabetes mellitus, n (%) | 22 (33.8) | 27 (22.0) | 0.24 |
| Previous myocardial infarct, n (%) | 10 (15.4) | 18 (14.6) | 0.93 |
| Previous PCI, n (%) | 1 (1.5) | 1 (0.8) | 0.77 |
| Previous stroke, n (%) | 1 (1.5) | 2 (1.6) | 0.57 |
| Creatinine clearance, mL/m2 | 71.9±32.3 | 91.2±31.3 | < 0.01 |
| Clinical status, n (%) | 0.09 | ||
| Unstable angina | 19 (29.4) | 21 (17.1) | |
| NSTEAMI | 16 (24.6) | 23 (18.7) | |
| STEAMI | 20 (30.8) | 59 (48.0) | |
| STEAMI post-reperfusion with SK (> 24 hours) | 2 (3.1) | 2 (1.6) | |
| STEAMI without reperfusion (> 24 hours) | 6 (9.2) | 18 (14.6) |
CAD, coronary artery disease; PCI, percutaneous coronary intervention; NSTEAMI, non-ST-segment elevation acute myocardial infarction; STEAMI, ST-segment elevation acute myocardial infarction; SK, streptokinase.
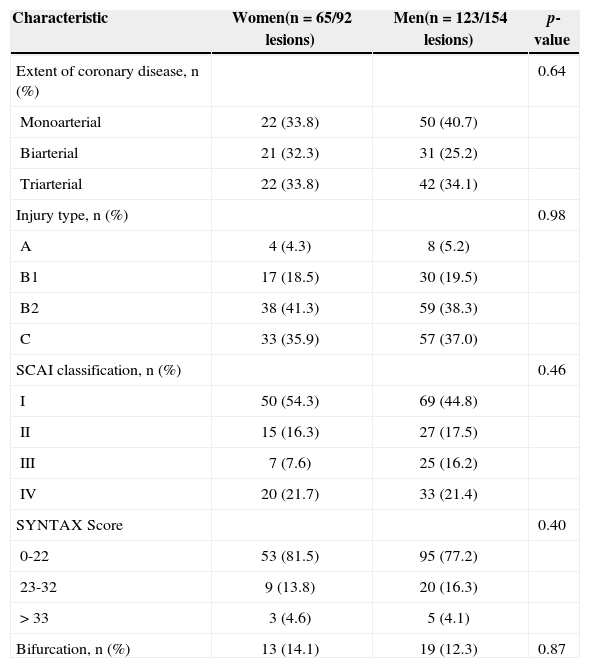
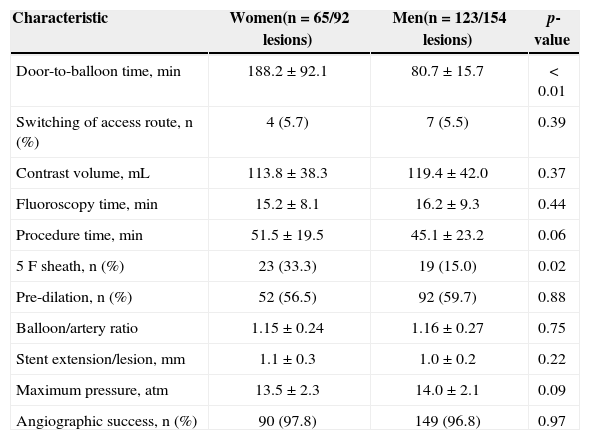
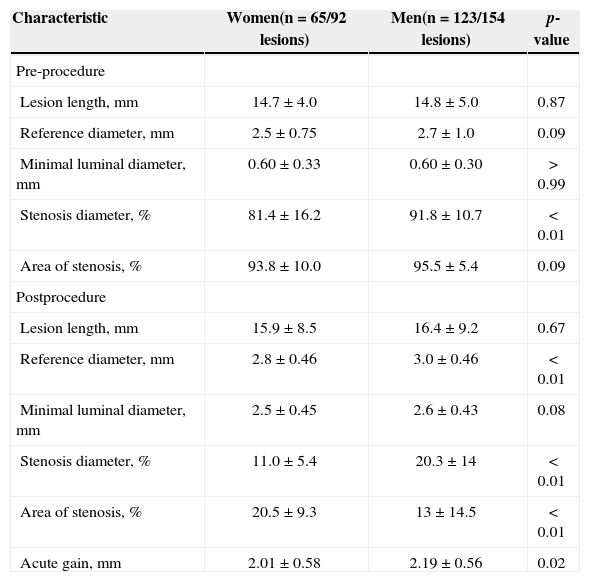
Regarding angiographic (Table 2) and procedural (Table 3) characteristics, no differences in relation to most of the variables between the groups were observed. Two-thirds of patients had multi-artery involvement, and non-C type lesions were the most frequently treated.The door-to-balloon time was significantly higher in patients undergoing primary PCI (188.2±92.1minutes vs. 80.7±15.7minutes; p < 0.01). Switching between access routes was rare (5.7% vs. 5.5%; p=0.39), and the volume of contrast used, fluoroscopy time, and procedure duration were similar between groups. 5F sheaths were used more often in the group of women (33.3% vs. 15.0%; p=0.02). The angiographic success was high and no difference between groups (97.8% vs. 96.8%; p=0.97) was noted. Quantitative coronary angiography (Table 4) showed that female patients had less calibrous vessels, with smaller diameters of stenosis.
Angiographic characteristics
| Characteristic | Women(n=65/92 lesions) | Men(n=123/154 lesions) | p-value |
|---|---|---|---|
| Extent of coronary disease, n (%) | 0.64 | ||
| Monoarterial | 22 (33.8) | 50 (40.7) | |
| Biarterial | 21 (32.3) | 31 (25.2) | |
| Triarterial | 22 (33.8) | 42 (34.1) | |
| Injury type, n (%) | 0.98 | ||
| A | 4 (4.3) | 8 (5.2) | |
| B1 | 17 (18.5) | 30 (19.5) | |
| B2 | 38 (41.3) | 59 (38.3) | |
| C | 33 (35.9) | 57 (37.0) | |
| SCAI classification, n (%) | 0.46 | ||
| I | 50 (54.3) | 69 (44.8) | |
| II | 15 (16.3) | 27 (17.5) | |
| III | 7 (7.6) | 25 (16.2) | |
| IV | 20 (21.7) | 33 (21.4) | |
| SYNTAX Score | 0.40 | ||
| 0-22 | 53 (81.5) | 95 (77.2) | |
| 23-32 | 9 (13.8) | 20 (16.3) | |
| > 33 | 3 (4.6) | 5 (4.1) | |
| Bifurcation, n (%) | 13 (14.1) | 19 (12.3) | 0.87 |
SCAI, Society for Cardiac Angiography and Interventions.
Procedure characteristics
| Characteristic | Women(n=65/92 lesions) | Men(n=123/154 lesions) | p-value |
|---|---|---|---|
| Door-to-balloon time, min | 188.2±92.1 | 80.7±15.7 | < 0.01 |
| Switching of access route, n (%) | 4 (5.7) | 7 (5.5) | 0.39 |
| Contrast volume, mL | 113.8±38.3 | 119.4±42.0 | 0.37 |
| Fluoroscopy time, min | 15.2±8.1 | 16.2±9.3 | 0.44 |
| Procedure time, min | 51.5±19.5 | 45.1±23.2 | 0.06 |
| 5F sheath, n (%) | 23 (33.3) | 19 (15.0) | 0.02 |
| Pre-dilation, n (%) | 52 (56.5) | 92 (59.7) | 0.88 |
| Balloon/artery ratio | 1.15±0.24 | 1.16±0.27 | 0.75 |
| Stent extension/lesion, mm | 1.1±0.3 | 1.0±0.2 | 0.22 |
| Maximum pressure, atm | 13.5±2.3 | 14.0±2.1 | 0.09 |
| Angiographic success, n (%) | 90 (97.8) | 149 (96.8) | 0.97 |
Quantitative coronary angiography
| Characteristic | Women(n=65/92 lesions) | Men(n=123/154 lesions) | p-value |
|---|---|---|---|
| Pre-procedure | |||
| Lesion length, mm | 14.7±4.0 | 14.8±5.0 | 0.87 |
| Reference diameter, mm | 2.5±0.75 | 2.7±1.0 | 0.09 |
| Minimal luminal diameter, mm | 0.60±0.33 | 0.60±0.30 | > 0.99 |
| Stenosis diameter, % | 81.4±16.2 | 91.8±10.7 | < 0.01 |
| Area of stenosis, % | 93.8±10.0 | 95.5±5.4 | 0.09 |
| Postprocedure | |||
| Lesion length, mm | 15.9±8.5 | 16.4±9.2 | 0.67 |
| Reference diameter, mm | 2.8±0.46 | 3.0±0.46 | < 0.01 |
| Minimal luminal diameter, mm | 2.5±0.45 | 2.6±0.43 | 0.08 |
| Stenosis diameter, % | 11.0±5.4 | 20.3±14 | < 0.01 |
| Area of stenosis, % | 20.5±9.3 | 13±14.5 | < 0.01 |
| Acute gain, mm | 2.01±0.58 | 2.19±0.56 | 0.02 |
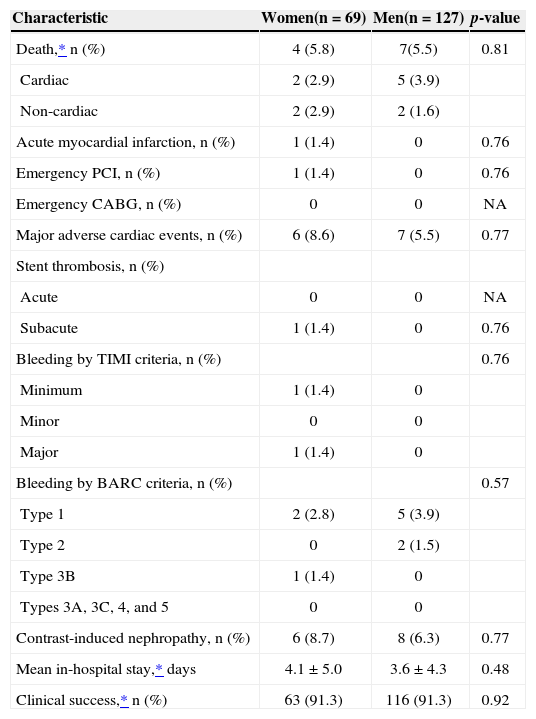
In-hospital death rates (5.8% vs. 5.5%; p=0.81), myocardial infarction (1.4% vs. 0; p=0.76), and urgent PCI (1.4% vs. 0; p=0.76) were similar between groups (Table 5). There was one case of subacute stent thrombosis in the group of women, with consequent myocardial infarction with ST-segment elevation and urgent percutaneous reintervention. Regarding the occurrence of bleeding, there was only one case of severe bleeding among women (major, type 3B by TIMI and BARC criteria, respectively), which occurred in a patient in whom switching of the access route to the femoral artery was necessary, and who required vascular surgical intervention.
Hospital outcomes
| Characteristic | Women(n=69) | Men(n=127) | p-value |
|---|---|---|---|
| Death,* n (%) | 4 (5.8) | 7(5.5) | 0.81 |
| Cardiac | 2 (2.9) | 5 (3.9) | |
| Non-cardiac | 2 (2.9) | 2 (1.6) | |
| Acute myocardial infarction, n (%) | 1 (1.4) | 0 | 0.76 |
| Emergency PCI, n (%) | 1 (1.4) | 0 | 0.76 |
| Emergency CABG, n (%) | 0 | 0 | NA |
| Major adverse cardiac events, n (%) | 6 (8.6) | 7 (5.5) | 0.77 |
| Stent thrombosis, n (%) | |||
| Acute | 0 | 0 | NA |
| Subacute | 1 (1.4) | 0 | 0.76 |
| Bleeding by TIMI criteria, n (%) | 0.76 | ||
| Minimum | 1 (1.4) | 0 | |
| Minor | 0 | 0 | |
| Major | 1 (1.4) | 0 | |
| Bleeding by BARC criteria, n (%) | 0.57 | ||
| Type 1 | 2 (2.8) | 5 (3.9) | |
| Type 2 | 0 | 2 (1.5) | |
| Type 3B | 1 (1.4) | 0 | |
| Types 3A, 3C, 4, and 5 | 0 | 0 | |
| Contrast-induced nephropathy, n (%) | 6 (8.7) | 8 (6.3) | 0.77 |
| Mean in-hospital stay,* days | 4.1±5.0 | 3.6±4.3 | 0.48 |
| Clinical success,* n (%) | 63 (91.3) | 116 (91.3) | 0.92 |
PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; NA, not applicable; TIMI, Thrombolysis In Myocardial Infarction; BARC, Bleeding Academic Research Consortium.
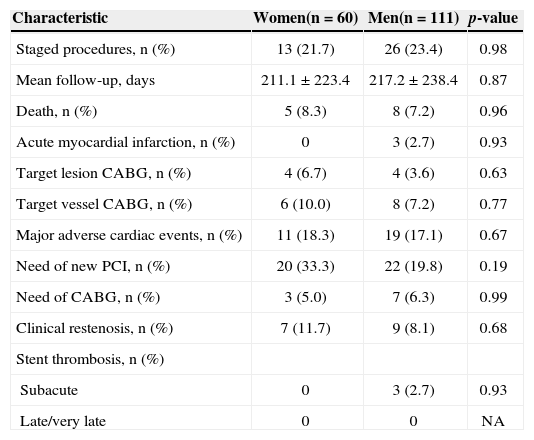
At late follow-up (Table 6), the average follow-up times were 211.1±223.4days and 217.2±238.4days (p=0.87), respectively, for women and men. No differences in rates of death (8.3% vs. 7.2%; p=0.96), myocardial infarction (2.7%vs. 0; p=0.93), target vessel CABG (10.0% vs. 7.2%; p=0.77), and MACE (18.3% vs. 17.1%; p=0.67) were observed. There were three cases of subacute stent thrombosis (0%vs. 2.7%, p=0.93) and no cases of late or very late stent thrombosis.
Late evolution
| Characteristic | Women(n=60) | Men(n=111) | p-value |
|---|---|---|---|
| Staged procedures, n (%) | 13 (21.7) | 26 (23.4) | 0.98 |
| Mean follow-up, days | 211.1±223.4 | 217.2±238.4 | 0.87 |
| Death, n (%) | 5 (8.3) | 8 (7.2) | 0.96 |
| Acute myocardial infarction, n (%) | 0 | 3 (2.7) | 0.93 |
| Target lesion CABG, n (%) | 4 (6.7) | 4 (3.6) | 0.63 |
| Target vessel CABG, n (%) | 6 (10.0) | 8 (7.2) | 0.77 |
| Major adverse cardiac events, n (%) | 11 (18.3) | 19 (17.1) | 0.67 |
| Need of new PCI, n (%) | 20 (33.3) | 22 (19.8) | 0.19 |
| Need of CABG, n (%) | 3 (5.0) | 7 (6.3) | 0.99 |
| Clinical restenosis, n (%) | 7 (11.7) | 9 (8.1) | 0.68 |
| Stent thrombosis, n (%) | |||
| Subacute | 0 | 3 (2.7) | 0.93 |
| Late/very late | 0 | 0 | NA |
PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; NA, not applicable.
In this center’s experience, PCI by radial approach proved as effective in females as in males in the setting of ACS, and also presented low rates of switching of the access route, bleeding, and puncture site complications.
Numerous studies have shown the benefits of using the radial approach in relation to the femoral route in ACS. Hetherington et al.7 showed, in an observational study of patients undergoing transradial primary PCI, a similar rate of in-hospital adverse cardiac events, as well as a reduction of vascular complications compared to femoral access. However, in RIFLE-STEACS, a randomized study, primary or rescue PCI using the radial vs. the femoral approach was associated with significantly lower cardiac mortality and bleeding rates.8 Likewise, Vorobcsuk et al.,9 in a meta-analysis of 12 studies with 3,324 patients undergoing PCI for myocardial infarction with ST-segment elevation by radial versus femoral approach, emphasized a reduction of 70% of the access site bleeding with the radial approach, and a lower incidence of adverse cardiac events and mortality. In the MORTAL registry; 38,872 patients with and without ACS undergoing PCI by radial or femoral approaches were retrospectively studied. The authors observed that transfused patients had a significantly increased mortality at 30 days and at 1 year, and that the radial approach reduced the transfusion rate. After adjusting for all variables, the radial approach was associated with a significant reduction in mortality at 30 days and at 1 year.10 Finally, RIVAL, the largest randomized study to date, compared radial and femoral accesses in 7,021 patients with ACS and showed, in patients with myocardial infarction with ST-segment elevation, gains in favor of radial access, which were largely influenced by a reduction of mortality, probably thanks to the reduction in bleeding rates.11 These results were found only among those surgeons most experienced in radial access (400 cases/year). In Brazil publications from Andrade et al.12 and from the present authors13 reproduced the benefits of the option for the radial approach in primary PCI.
Regarding the approach of women with PCI, historically this group of patients presents worse acute and late outcomes, compared with men.14 More recent studies have demonstrated that unadjusted ischemic events remain unfavorable for women; however, statistical adjustment for baseline differences usually neutralizes the impact of the female gender factor.15
Regarding vascular complications of access route and of bleeding, there are few studies addressing the impact of the female gender on the results of PCI, especially in cases of ACS. Tizón-Marcos et al.,16 in a sub-analysis of the EARLY study, evaluated 1,348 ACS patients undergoing PCI by radial approach, by comparing the results according to gender. In agreement with the present results, the women in that sub-analysis showed worse renal function and greater use of 5F sheaths, with no difference in the rate of ischemic events and major bleeding, when compared to men. The authors suggested that the systematic transradial approach is more important than the choice of an antiplatelet and antithrombotic regimen for the reduction of bleeding and adverse outcomes in this population.16
Study limitationsThis study has limitations inherent to all retrospective and observational studies. Additional limitations are related to the small population and to the fact that the study was conducted in a single center, where radial access is the predominant technique for the performance of coronary, diagnostic, and therapeutic procedures.
CONCLUSIONSIn this center’s experience, PCI by radial approach proved as effective in females as in males in the setting of ACS, with a high success rate of the procedure and similar clinical outcomes. PCI was also shown to be safe, since bleeding was a rare event in the evaluated population.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
SOURCE OF FINANCINGNone.