We report the case of an 81-year-old patient with symptomatic severe aortic stenosis (AS) who developed refractory hemodynamic instability and respiratory arrest during a diagnostic cardiac catheterization. The patient was submitted to a percutaneous balloon aortic valvuloplasty as a life saving procedure with subsequent hemodynamic improvement and clinical stabilization. The possibility of surgical treatment for AS was excluded due to the high surgical risk. Clinical follow-up of up to 7 months after the procedure demonstrated significant improvement in functional class and good exercise tolerance.
Valvuloplastia Aórtica Percutânea como Medida Salvadora naEstenose Aórtica Crítica com Instabilidade Hemodinâmica
Relatamos o caso de uma paciente de 81 anos, com estenose aórtica (EA) grave sintomática, que, durante cateterismo cardíaco diagnóstico, evoluiu com instabilidade hemodinâmica refratária e posterior parada respiratória. Foi submetida à valvuloplastia aórtica percutânea por balão como medida salvadora, com subsequente melhora hemodinâmica e compensação clínica. A possibilidade de tratamento cirúrgico da EA foi descartada pelo alto risco cirúrgico. O acompanhamento clínico de até 7 meses após o procedimento demonstrou melhora significativa da classe funcional e boa tolerância aos esforços.
Senile aortic stenosis (AS) is the obstruction of the left ventricular outflow tract due to valvular structure calcification, whether or not associated with aortic valve fusion. It is the most commonly acquired aortic valve disease, and is present in 4.5% of population older than 75 years.1 Surgical aortic valve replacement is the first-choice therapy for patients with severe AS, resulting in symptom relief and increased survival. However, due to the high surgical risk, approximately one-third of octogenarians with symptomatic AS are rejected for surgery.2 Percutaneous balloon aortic valvuloplasty (PBAV) is a procedure considered to be a bridge in hemodynamically unstable patients not capable of undergoing surgical procedure. Due to the high incidence of restenosis and aortic regurgitation, it is currently indicated only in exceptional circumstances, for instance, as a palliative measure or intermediate to a definitive treatment.3 Currently, percutaneous aortic valve implantation (PAVI) is an option for patients with high risk for conventional surgical treatment. Since 2002, from the initial experience by Cribier et al.,4 over 50,000 PAVI shave been performed with different devices.5
The present study reports a case of an emergency PBAV performed due to the occurrence of severe and refractory hemodynamic instability during angiography procedure.
CASE REPORTThe patient was an 81-year-old female, with a known history of hypertension and dyslipidemia, with AS for five years, dyspnea on moderate exertion, and typical anginal chest pain. Approximately one year before, she experienced worsening of functional class, with dyspnea on mild exertion, syncope, and angina episodes. A transthoracic echocardiography performed in September 2012 demonstrated a tricuspid aortic valve with significant calcification, mean transvalvular gradient of 65mmHg, peak velocity of 5.3m/s, estimated valve area of 0.63cm2, left ventricular ejection fraction (LVEF) of 55%, and interventricular septum of 15mm, meeting the echocardiographic criteria for severe aortic stenosis (without aortic insufficiency).
In October 2012, the patient underwent diagnostic cardiac catheterization for preoperative evaluation purposes. During the examination, the patient developed refractory hemodynamic instability, acute respiratory failure, decreased level of consciousness, and subsequent respiratory arrest, requiring orotracheal intubation and high doses of vasoactive agents. Given the critical situation, with rapid clinical deterioration and need for increasingly higher doses of norepinephrine, it was decided to perform the PBAV promptly.
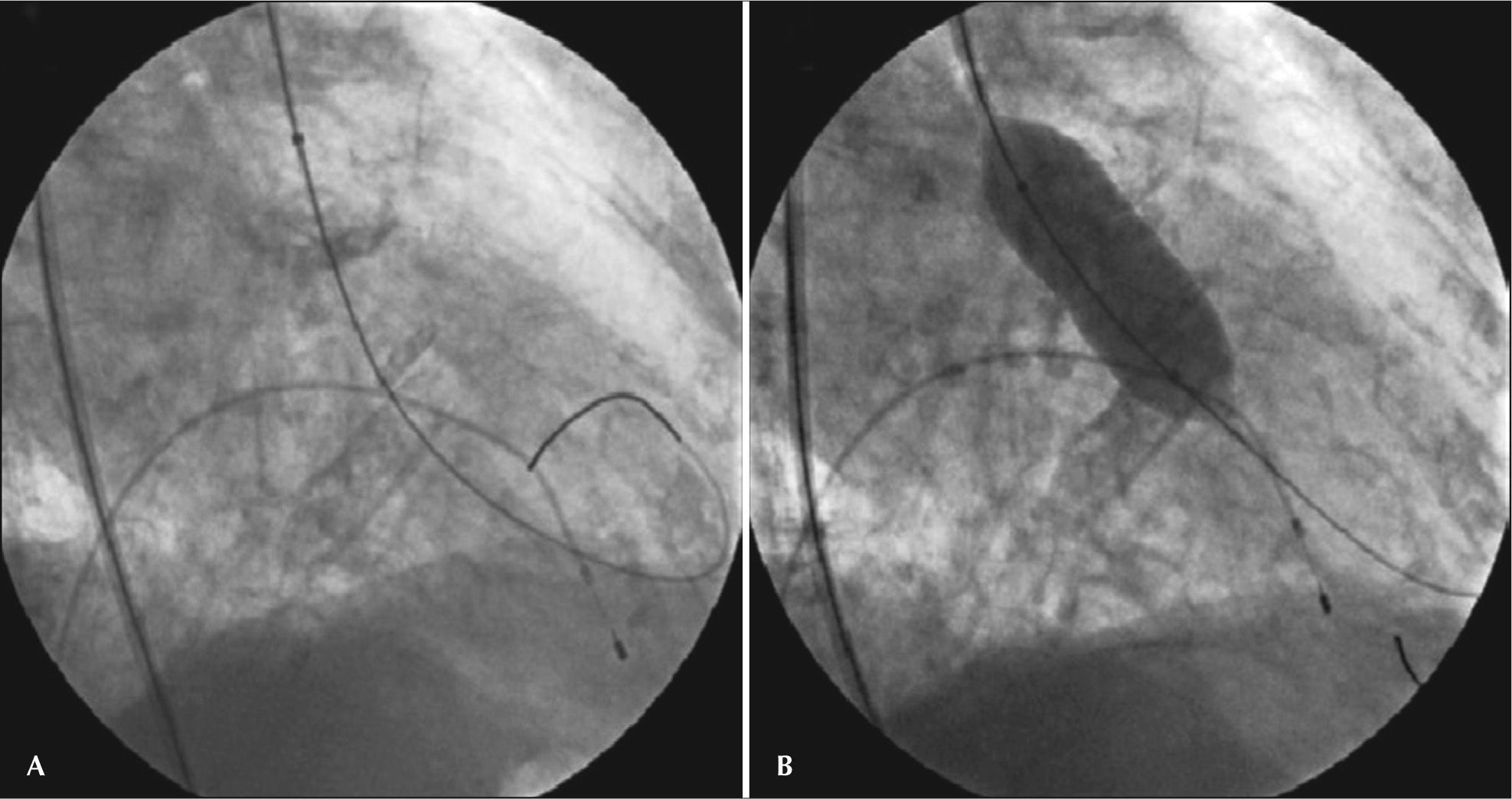
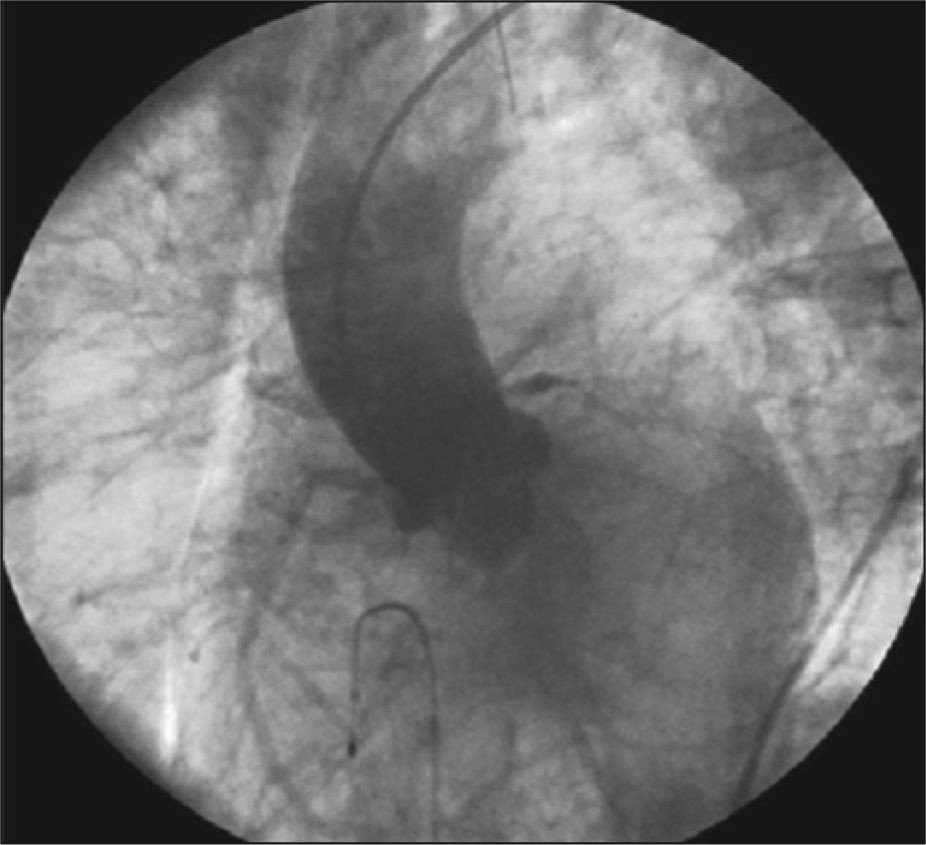
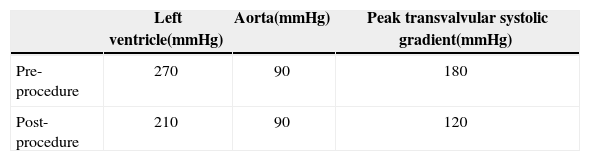
ProcedureThe PBAV was performed through the right femoral artery. A 23×45mm Aviator® Plus balloon (Cordis Corporation, Bridgewater, USA) was used, inflated once for less than 10 seconds (Figure 1), with the aid of rapid pacing with temporary transvenous pacemaker positioned in the right ventricle via the right femoral vein, for stable positioning of the balloon. An immediate decrease was observed in the aortic transvalvular systolic pressure gradient, from 180mmHg to 120mmHg (Table 1), with significant improvement in hemodynamic status and prompt norepinephrine weaning. The control angiogram showed only mild aortic valve regurgitation (Figure 2). Echocardiography was not available during or immediately after the procedure. The patient was then transferred to the intensive care unit, for clinical stability and decision-making on the future surgical treatment of the AS.
– Emergency percutaneous balloon aortic valvuloplasty: (A) passage of the extra-stiff guidewire through the aortic valve plane to deliver and position the balloon, (B) 23×45mm Aviator® Plus balloon inflated once for less than 10 seconds with the aid of rapid pacing with temporary transvenous pacemaker, positioned in the right ventricle through the right femoral vein for stable placement of the balloon.
The post-procedural outcome was favorable, and the patient was extubated within 24 hours, with restoration of hemodynamic stability without vasoactive drugs. Echocardiogram performed at the bedside 48 hours after PBAV maintained the criteria for severe AS, despite the clinical improvement (mean transvalvular gradient of 48mmHg; aortic valve area of 0.91cm2; LVEF 59%). Due to the risk surgical high (estimated mortality according to the European System for Cardiac Operative Risk Evaluation [EuroSCORE II] of 15.2% and a Society of Thoracic Surgeons [STS] risk score of 52.1%), as well as the difficulties to perform PAVI under the public health system, and considering the satisfactory progress after PBAV, it was decided to maintain the patient in clinical treatment.
The patient was discharged after ten days, in good general status and asymptomatic, with no complications from the procedure. She was referred to cardiologic clinical monitoring. Seven months after the procedure, the patient was asymptomatic from the cardiovascular perspective, without the occurrence of any adverse cardiac events, with good tolerance to exertion (functional class I), and no change in AS classification at the echocardiography.
DISCUSSIONPBAV was developed as a non-surgical option in 1980 for the treatment of patients with severe AS. It is a procedure in which one or more balloons are placed through the stenotic aortic valve and inflated in order to reduce lesion severity. It causes fractures in the calcium deposited in the valve leaflets, with enlargement of the aortic annulus and separation of commissures.6 Despite the considerable rates of possible complications (severe acute aortic regurgitation, vascular/hemorrhagic complications and access route-related complications, stroke, and death), the immediate results produce a moderate decrease in transvalvular gradients with symptomatic improvement, but only a small increase in valvular area, which determines high restenosis rates and poor medium- and long-term outcome.7
The PBAV technique has undergone improvements in last years, such as a decrease in the catheter diameter; more reliable balloons (smaller profile, and simpler and safer materials in the technical management); rapid ventricular rhythm established by a pacemaker, stabilizing the baloon in the aortic valve plane during dilation; and more appropriate guide wires (extra-stiff, super-stiff), among others. Currently, PBAV is strongly recommended as valve preparation for subsequent PAVI (pre-dilation), and has been increasingly used, in parallel with the bioprosthesis catheter-implantation technique.8
A patient with critical AS with acute heart failure or cardiogenic shock represents a therapeutic challenge, as this is a condition whose definitive treatment is complex and carries a high risk of death. PBAV is generally used in this context as a bridge to surgery; however, due to the modest increase in valve area and the reasonable complication rate, there is a limitation for its use, even in these patients.9 In 2008, the updated guidelines of the American College of Cardiology/American Heart Association (ACC/AHA) for the management of valvular heart disease indicated that PBA was a class IIb recommendation as palliative care or a bridge to surgery in unstable patients or those with severe comorbidities (and class III for its use as a routine alternative to surgical valve replacement).10 With similar recommendations, the Brazilian guidelines on valve disease, from 2011, added the indication of class IIa for PBAV in hemodynamically unstable patients and momentary incapacity to undergo PAVI, maintaining the IIb indication when treatment is considered palliative. 11 In practice, PBAV has restricted use and does not modify the natural history of the disease, as well as resulting in only temporary symptom improvement thus requiring a subsequent final treatment.
In this case, PAVI bioprosthesis was considered as the most suitable alternative for definitive treatment of the patient, which has been approved for use in Brazil by the National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária – ANVISA) since 2008. According to the Placement of Aortic Transcatheter Valves Trial (PARTNER),12 an important randomized clinical trial conducted at 21 centers in the United States, Canada, and Germany, it was observed that mortality, both early and late, was dramatically reduced when patients were treated with PAVI, in comparison with medical treatment eventually associated with PBAV. Furthermore, in the cases considered to be perioperative high-risk, mortality was equivalent when PAVI was compared with surgical treatment, demonstrating that percutaneous implantation of aortic bioprosthesis is a safe therapeutic option for this population.13
To date, PAVI is a therapeutic modality that is not available in the public healthcare system in Brazil. Thus, although scarcely recommended and even discredited by many, PBAV can improve the quality of life of many patients, and it is a viable alternative in the search for health, as cardiologists wait for the regulatory authorities to approve the inclusion of PAVI in the country’s public and private health systems.
This case report illustrates the actions of the interventional cardiologist during a life-saving measure. The use of PBAV in severe AS was indicated on an emergency basis, due to cardiogenic shock, imminent risk of death, and high surgical risk.
The procedure was able to promote subsequent improvement in hemodynamics and clinical compensation. The authors believe that PBAV should be considered a valid option, whether or not associated with subsequent percutaneous or surgical aortic valve implantation, especially in unstable patients in critical condition. In the context of PAVI use, it can be stated that PBAV may be once again considered in clinical practice.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.