The first report of an intravascular catheter fragmentation was published in 1954 and ever since we have observed a remarkable evolution in the techniques of intravascular foreign body removal. The pioneer description of non-surgical foreign body removal dates back to 1964, with the report of a guidewire fragment withdrawal using a bronchoscopy biopsy forceps. Despite the availability of several dedicated devices, materials may have to be adapted at times to achieve technical success. We report the case of a patient with a Port-a-Cath catheter in the left subclavian vein, which had been placed 5 years before and whose intravascular portion was broken during withdrawal. It was successfully removed using the percutaneous approach.
Remoção Percutânea de Fragmento de Cateter Intravascular– uma Adaptação da Caixa de Ferramentas
A fragmentação de um cateter intravascular foi primeiramente publicada em 1954 e, desde então, observamos notável evolução das técnicas de retirada de corpo estranho intravascular. A descrição pioneira de remoção não cirúrgica de corpo estranho data de 1964, com o relato da retirada de fragmento de fioguia com auxílio de um fórceps de biópsia para broncoscópio. Apesar da disponibilidade de variados dispositivos dedicados, por vezes, para se ter sucesso, é necessária a adaptação de materiais. Relatamos aqui o caso de uma portadora de cateter Port-a-Cath em veia subclávia esquerda, implantado 5 anos antes, que rompeu a porção intravascular durante sua retirada, tendo sido removido com sucesso por via percutânea.
Since the first description of catheter fragmentation in 19541 and the pioneering nonsurgical removal of a foreign body in 1964,2 a remarkable evolution of materials has occurred in the context of interventional cardiology and endovascular procedures. However, sometimes creativity and adaptation of materials are still needed in order to achieve technical success.
The incidence of intravascular embolization of venous catheter accounts for approximately 1% of complications associated to the central venous access and may present with significant mortality rates. Among the several causes of catheter and endovascular guide wire fragmentation, Tateishi and Tomizawa3 mention: (1) improper use and handling of the device; (2) tool manufacturing defect; and (3) other causes, such as patient anatomical factors.
Catheter fractures occur most commonly when they are introduced by venous access, with fractures resulting from catheter compression by the clavicle and the first rib, known as pinch-off syndrome.4 This complication can be reduced using the jugular access or the more lateral portion of the subclavian vein. A systematic review of 215 cases demonstrated that the most common sites of embolization are the pulmonary arteries (35%), the right atrium (27.6%), and the right ventricle (22%). The occurrence of foreign bodies resulting from fragmentation of devices used for arterial access is less frequent.
There is evidence that the removal of the foreign body as early as possible is necessary to prevent complications, such as thromboembolism, mechanical myocardial injury, arrhythmias, endocarditis, sepsis, and death.5,6 Mortality, in the case of foreign body embolization, ranges between 24% and 60%.7
Thus, the benefit of foreign body removal appears to be a consensus, and percutaneous removal is considered the first alternative due to its minimally invasive nature and low rate of complications.8
CASE REPORTFemale patient, 41 years old, diagnosed with non-Hodgkin’s lymphoma, was submitted to Port-a-Cath F6 catheter implantation in the left subclavian vein for chemotherapy administration in August 2007.After eight months of treatment, there was complete disease remission. However, the catheter was maintained for further infusion in case of recurrence, until the end of 2012.
In December 2012, an attempt was made to remove the Port-a-Cath system, and it broke in the intravascular portion during the procedure, which prevented its removal, even after local surgical incision. Non-invasive assessment was performed by radiography and computed tomography, which showed the fragment in venous territory, extending from a tributary of the left subclavian vein to the supra-hepatic vein system, passing through the right atrium.
The percutaneous procedure was the team’s consensus option, with the alternative of surgical treatment in case of failure or complications. The percutaneous intervention was initiated by venous access with an 8F sheath (Input TS; Medtronic, Minneapolis, USA) in the common right femoral vein, followed by the administration of 5,000 units of unfractionated heparin.
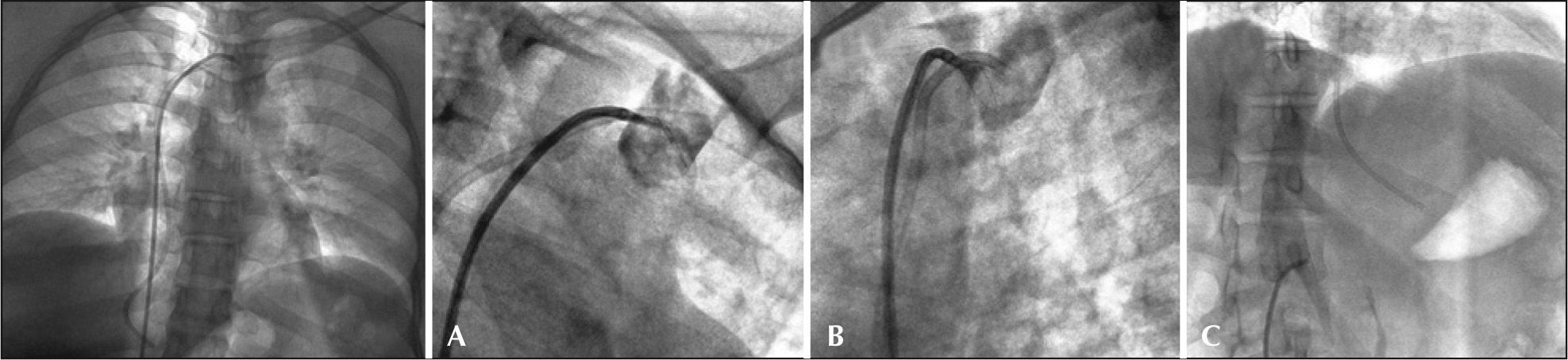
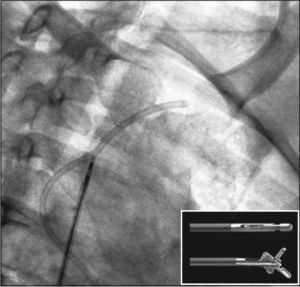
After obtaining vascular access, an 8F Judkins catheter guidewire, 4 curve (Launcher, Medtronic, Minneapolis, USA) was passed through the venous system, and contrast was administered in order to delineate the vascular anatomy (Figure 1). The location of the fragment ends was confirmed in a tributary of the subclavian vein and in the supra-hepatic venous system, preventing the capture of the ends by a loop catheter.
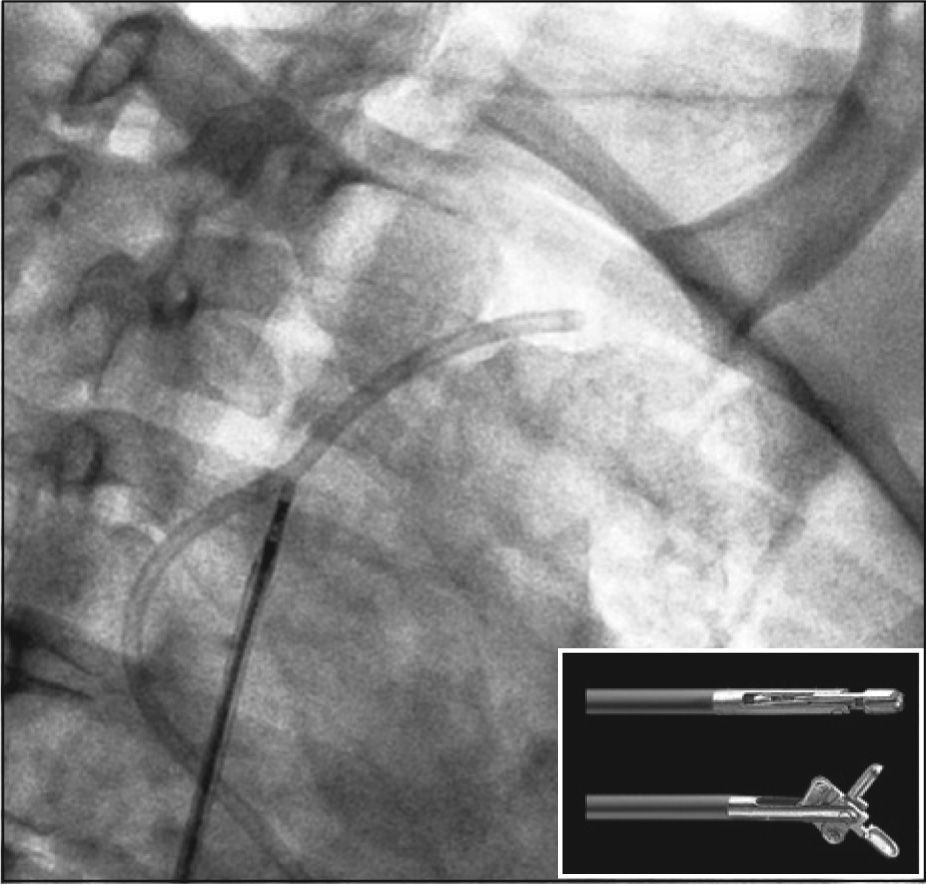
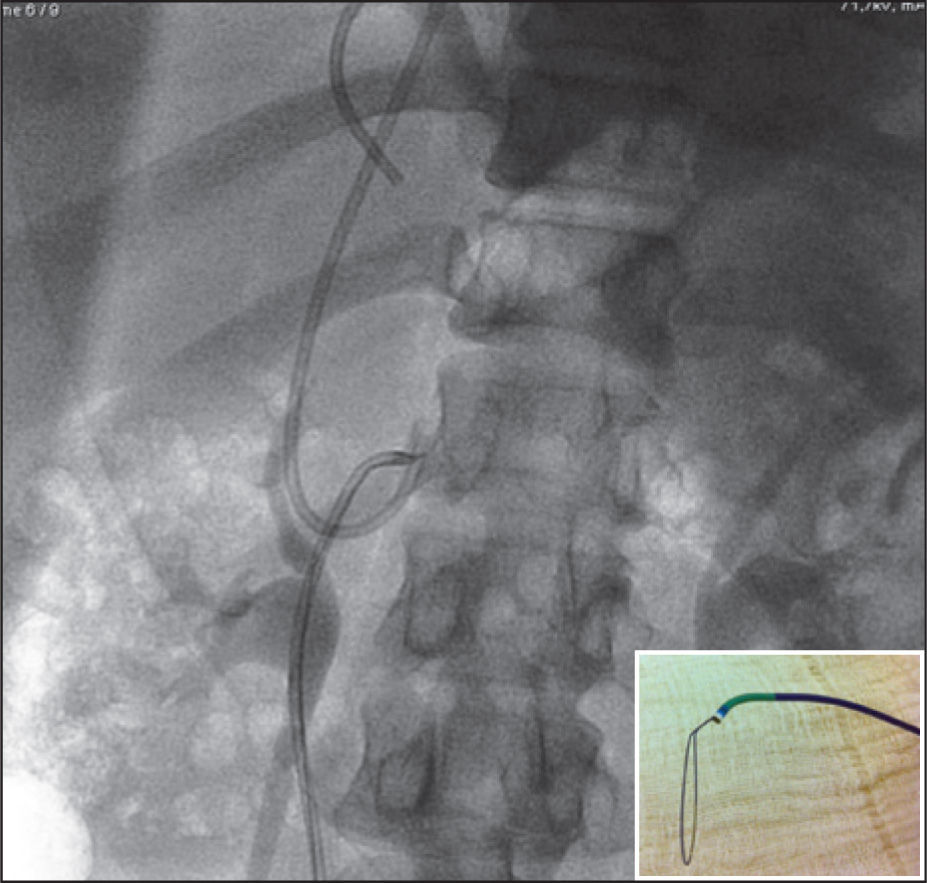
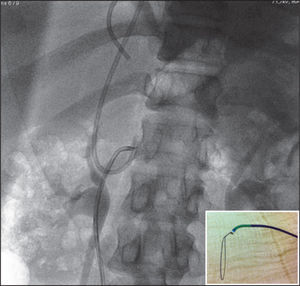
A 5.2F percutaneous myocardial bioptome (Cook; Cook Medical Inc.,USA) was used to bring the piece to a higher-calibre territory, so that it would be possible to clamp the catheter fragment in its upper portion (Figure 2) and pull this extremity to the inferior vena cava. After mobilization of the foreign body, the capture of the extremity using the loop technique was carried out with a 0.014 “ × 300cm guide wire (Zinger; Medtronic-Minneapolis). This technique consists of gently bending the guide wire into two equal parts; the formed curve is inserted into a catheter and exteriorized in its distal extremity, shaping it at a 45° angulations (Figure 3) and forming a loop, which can be manipulated by the extremities of the guide catheter.
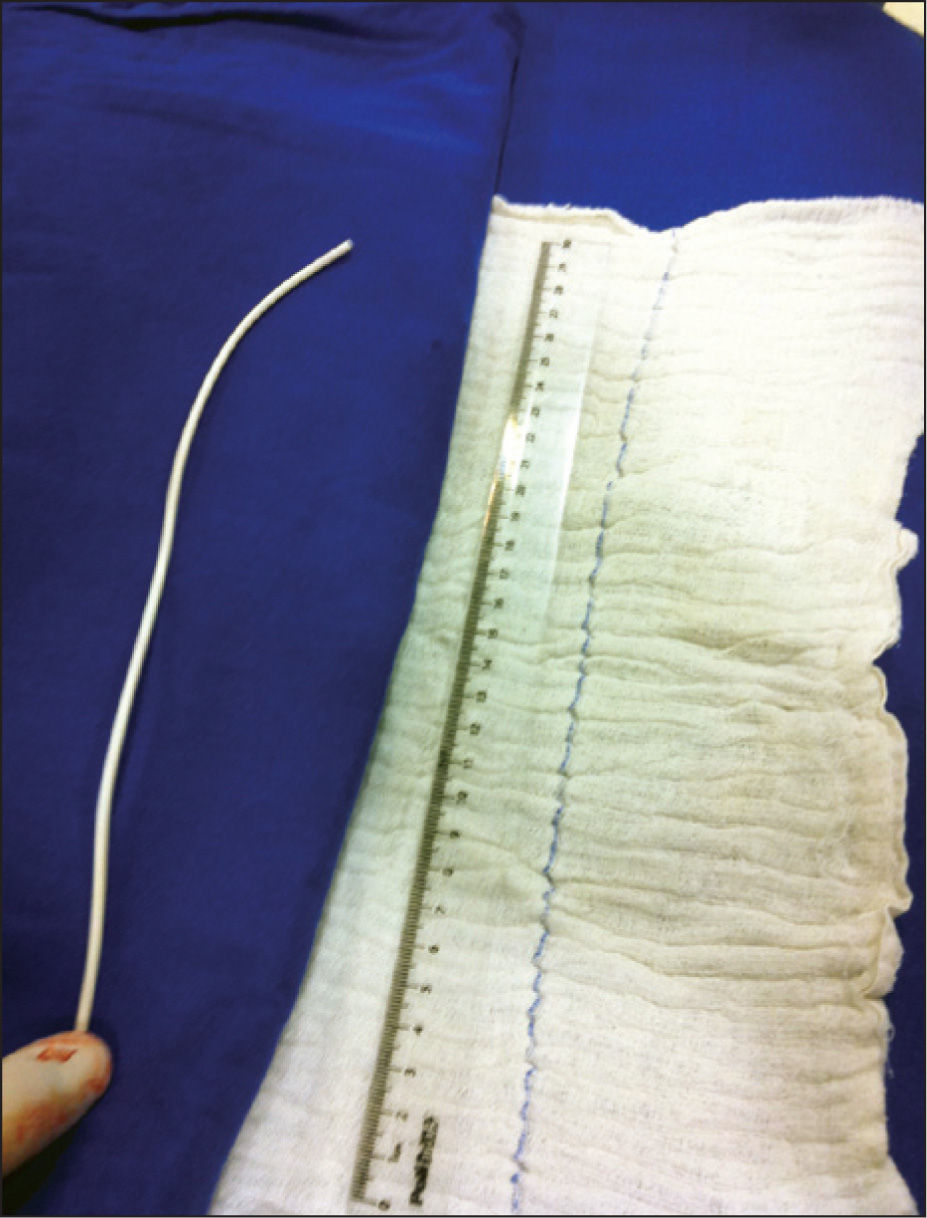
After the capture, the removal was performed through the introducer sheath, followed by the externalization of the catheter Port-a-Cath fragment, which measured 28cm (Figure 4). After the sheath was removed, local compression was performed for 15 minutes. The patient was discharged after resting for six hours and had an uneventful recovery; she was revaluated after 48 hours and 30 days.
DISCUSSIONRecent publications focusing on venous catheters have shown success rates of fragment removal with the percutaneous technique of 80% to 100%, with zero mortality and low complication rates,8,9 even in neonates.10 The most often described access route in literature is the common femoral vein, preferably the right, due to advantages such as convenience in handling material, access to main sites of venous foreign body migration, the possibility of using larger-calibre sheaths, easier puncture procedure, and safety of effective compression after the end of the procedure.
Most interventionists will have the opportunity to find a vascular foreign body during their clinical practice. Although there is a significant complication rate in cases of non-removal of fragment, the incidental finding in other imaging tests is not uncommon, and is reported in approximately 40% of cases referred for assessment.11
From the earliest techniques to the development of dedicated devices, such as the Amplatz GooseNeck® loops, there are several available tools to remove foreign bodies from the vascular system, and loops are currently considered the most versatile. In this present case, the authors would use as an alternative, after the initial traction, the GooseNeck® catheter; however, this device was not available at the time of procedure. There is also the possibility of capturing a foreign body with inaccessible extremities with a hook and loop formed by the guide wire and a pigtail-type catheter, which could be used in case of failure of the performed technique.12
Although cases reports certainly do not allow an adequate level of evidence for generalizations, in the present case, the use of a bioptome showed to be a safe and effective technique. Among the list of options including loops of different sizes and angles, baskets, balloons, magnets, and forceps, it is important for the professional to become acquainted with the available options, aiming at their adequate use and, sometimes, adapting the tools to achieve success in challenging cases.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.