Spontaneous coronary dissection is a rare entity and, therefore, its etiology, pathophysiology, and treatment are not yet established. It affects mainly young women without the classic cardiovascular risk factors, commonly during the pregnancy-childbirth cycle. Several factors influence the treatment strategy, such as clinical presentation, hemodynamic status, topography, number of affected arteries, and distal coronary flow. As in the reported case, in stable patients with well-defined dissections and mainly when the coronary flow has been re-established, one can choose a conservative approach, due to the high incidence of spontaneous resolution and low incidence of long-term adverse events.
A dissecção coronária espontânea é uma entidade rara e, por conseguinte, de etiologia, fisiopatologia e tratamento ainda não estabelecidos. Acomete, em geral, mulheres jovens, sem os clássicos fatores de risco cardiovascular, comumente ao longo do ciclo gravídico-puerperal. Vários fatores influenciam na estratégia de tratamento, como quadro clínico, status hemodinâmico, topografia da dissecção, número de artérias afetadas e fluxo coronário distal. Como no caso relatado, em pacientes estáveis, com dissecções bem delimitadas e, sobremodo, quando o fluxo coronário é reestabelecido, pode-se optar por uma abordagem conservadora, em razão da alta incidência de resolução espontânea e da baixa incidência de eventos adversos a longo prazo.
Spontaneous coronary dissection is a rare, potentially underdiagnosed entity and, therefore, its etiology, pathophysiology, and optimal management are still little known. It is found in the literature almost exclusively as case reports or small case series, and it mainly affects young women without the classic cardiovascular risk factors, commonly during the pregnancy-childbirth cycle. Revascularization of the affected coronary bed, either surgical or percutaneous, is employed in most cases.1–4 However, in casual presentations with clinical and hemodynamic stability, associated with patency of the affected vessels, the conservative approach can be adopted, as in this case report.
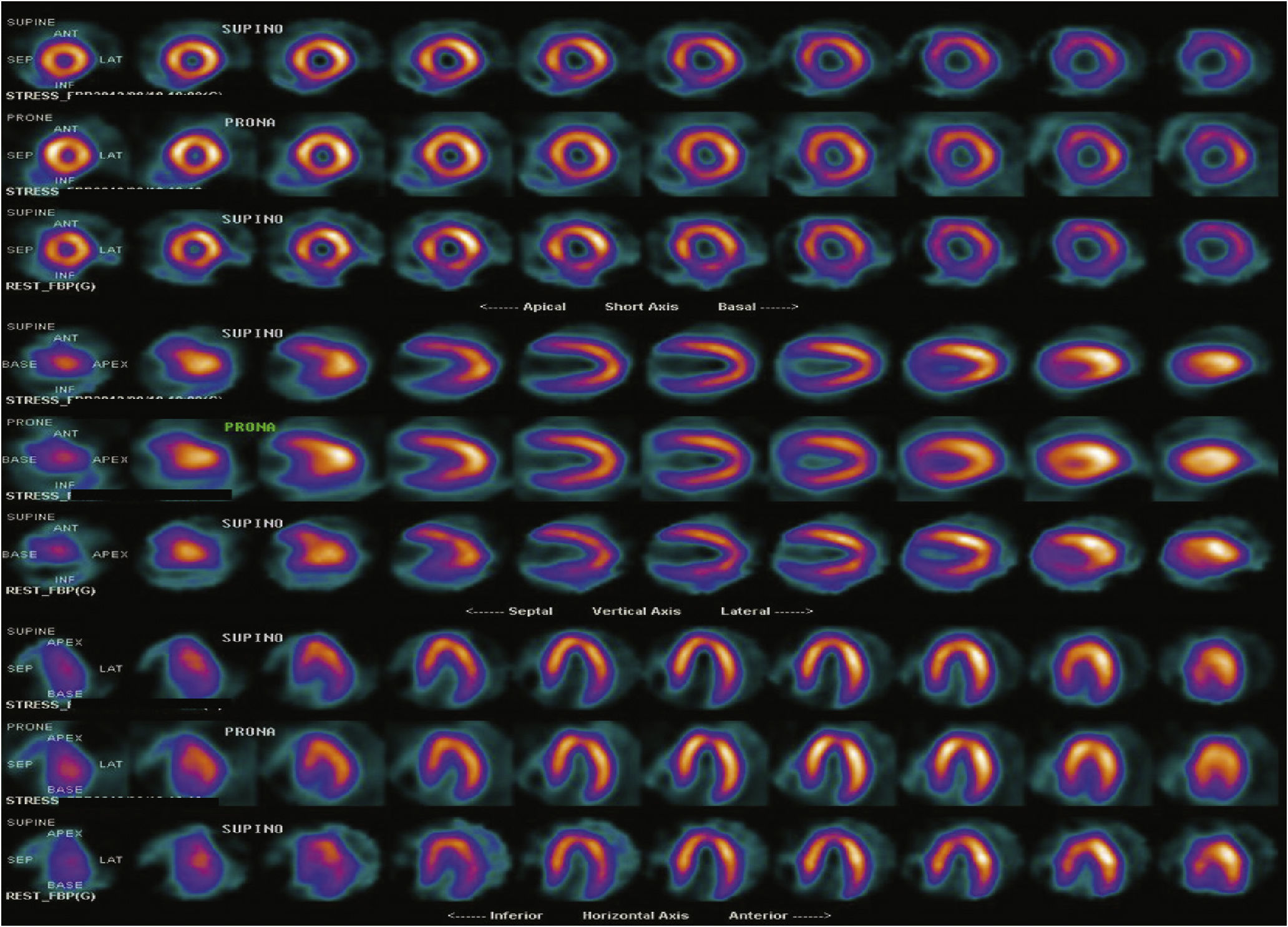
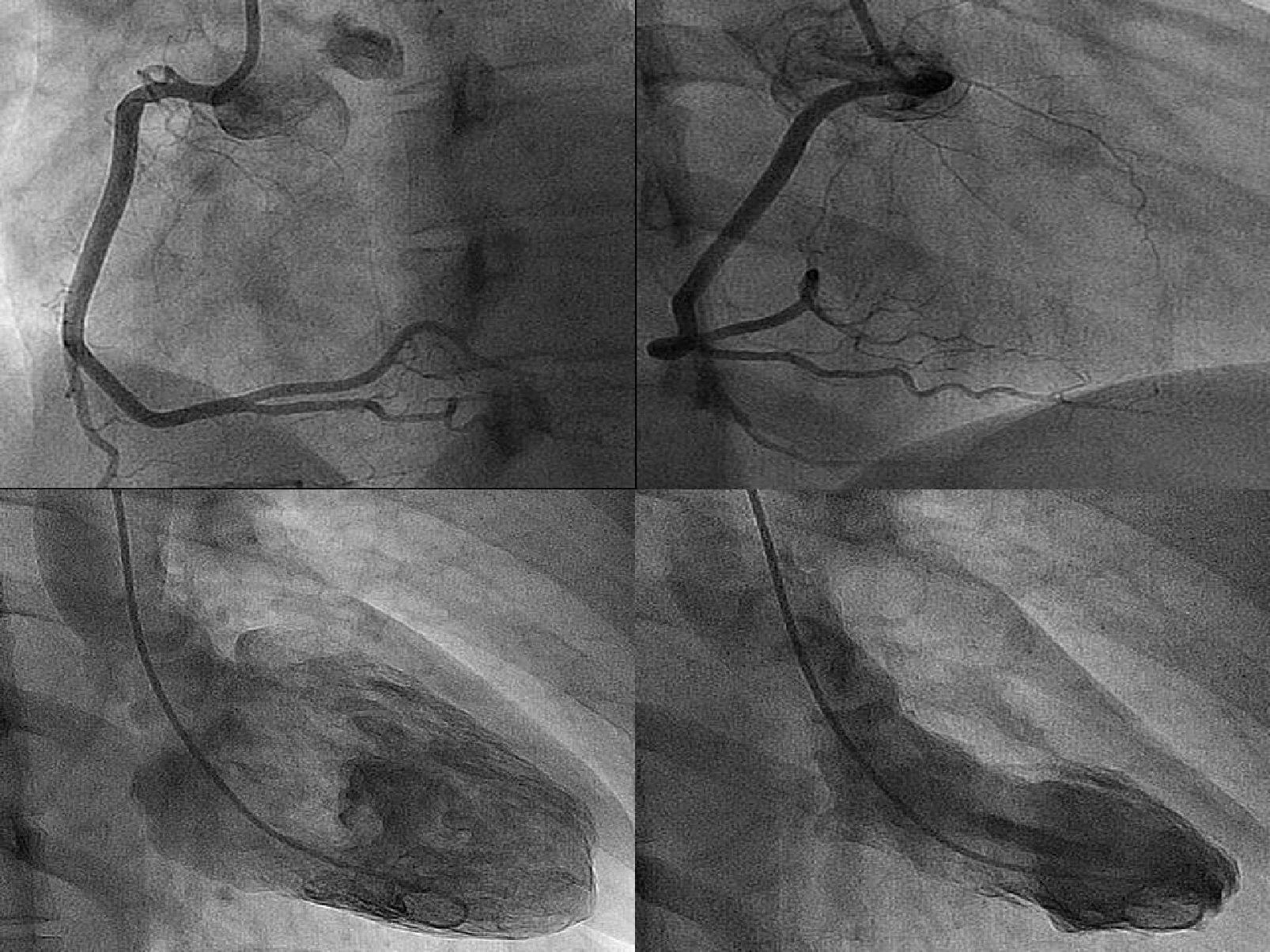
Case reportA 41-year-old married white woman, with no cardiovascular risk factors or relevant pathological history had, on the eighth day after delivery of her first child (normal delivery), oppressive chest pain at rest, which resolved 20minutes after receiving sublingual nitrate at the emergency medical service. Due to the characteristic increase in myocardial necrosis markers, a diagnosis of non-ST segment elevation myocardial infarction (electrocardiogram with no acute ischemic changes) was established, with clinical, electrical, and hemodynamic stability. She underwent a coronary angiography at another service, 24hours after symptom onset, which showed extensive spontaneous coronary dissection in the proximal and middle portions of the left anterior descending artery, with Thrombolysis in Myocardial Infarction (TIMI) 3 distal flow. Because of the stable presentation, a non-interventionist strategy was chosen, with clinical treatment based on dual antiplatelet therapy (acetylsalicylic acid and clopidogrel), beta-blocker, and statin. She was discharged after normalization of cardiac myonecrosis markers, without any recurrence of signs or symptoms of ischemia. During the follow-up, she remained asymptomatic, with no evidence of stress-induced myocardial ischemia (Fig. 1). A control coronary angiography, performed at the discretion of the attending cardiologist, carried out in this service 4 months after the acute event, confirmed the finding of extensive dissection of the left anterior descending artery, from its ostium to its middle segment, affecting the origin of a diagonal branch, both with TIMI 3 flow (Fig. 2). The dominant right coronary artery, showed no lesions; the left ventriculography disclosed normal contractile function and mitral valve competence (Fig. 3). Due to the absence of symptoms and documented ischemia, a conservative approach was chosen once again, after discussion with the Heart Team. Ten months after the index event, the patient remained asymptomatic, with no functional limitation or recurrence of similar episodes.
Left coronary angiography in different views, showing the extensive dissection layer in the left anterior descending artery, from its ostium to its middle segment, involving the origin of a large diagonal branch, sparing the left main coronary artery and the left circumflex artery.
Spontaneous coronary dissection is a rare cause of cardiovascular events and may present as acute coronary syndrome with or without ST-segment elevation, acute heart failure, or even sudden death, usually due to involvement of the left main coronary artery.1–4 First described in 1931, in a 42-year-old woman,5 the prevalence ranges from 0.1 to 1.1%, according to series of patients submitted to coronary angiography.1
It has a female:male ratio of 3:1 and up to one-third of cases are observed during pregnancy or in the postpartum period. In women, the dissections predominantly occur in the left coronary artery (87%), and usually affect young women without classic risk factors. Men, in turn, tend to be affected at a slightly older age, sometimes with concomitant presence of risk factors, and with the involvement of the right coronary artery in two-thirds of cases.3 In general, the left anterior descending artery is affected in 75% of patients, the right coronary artery in 20%, the left circumflex artery in 4%, and the left main coronary artery in less than 1%.3 There is a strong association between spontaneous coronary dissection and pregnancy, the postpartum period, and the use of oral contraceptives. During pregnancy, there may be pathological changes in the artery due to the fragmentation of reticular fibers, smooth muscle cell hypertrophy, and changes in mucopolysaccharide content and protein composition, with a consequent weakening of its the vascular wall, leading to an increased risk of intimal tears during or after labor.2,6
The clinical and angiographic diagnosis of this entity may be underestimated because intravascular imaging techniques are not used in most cases. Although suggestive, the angiographic appearance may not clearly depict the phenomenon, which should be considered when there is an intimal tear with or without a false lumen, a sudden and significant reduction in caliber, or an obstruction with smooth edges and without signs of atherosclerotic disease.2–4
Intravascular ultrasound and optical coherence tomography allow a more thorough evaluation of spontaneous coronary dissection, as they provide detailed morphological information of coronary lesions and the location of the dissection planes between the different layers of the arterial wall. Additionally, noninvasive coronary angiography has been used in clinical follow-up of patients who underwent spontaneous coronary dissection.7
Because of its rarity, the optimal management of this condition has yet to be determined. Several factors influence treatment strategy, such as clinical presentation, hemodynamic status, topography, number of affected arteries, distal coronary flow, and availability of interventional cardiology and cardiac surgery services.1–4
Percutaneous coronary intervention is the treatment of choice in cases of symptomatic single-vessel dissection and/or acute ischemia. Stent implantation aims to seal the intimal flap and re-expand the true lumen. There are no proven benefits of drug-eluting stents when compared to bare-metal stents. Moreover, it is unknown whether their use prevents recurrence of the dissection.4 Coronary artery bypass grafting surgery is an alternative in cases with multivessel involvement, in the dissection of the left main coronary artery, or when there is percutaneous treatment failure.4 As in this case, in clinically and hemodynamically stable patients, with well-defined dissections and mainly when coronary flow is re-established, a conservative approach can be chosen due to the high incidence of spontaneous resolution of the dissection, which has been verified by late angiographic studies,8 and the low incidence of long-term adverse events.1–4
In a recent review of a consecutive series of 25 cases of spontaneous coronary dissection in our service, the authors found the following: prevalence of females (56%); mean age of 48.8 ± 10 years; presentation as acute coronary syndrome in 92%; involvement of the left anterior descending artery in 48%; in-hospital and late event-free rates of 92% and 84.2%, respectively; conservative management in 56%, percutaneous in 40%, and surgical revascularization applied in only one case, with spontaneous multivessel coronary dissection.9
Overall, the survival rates after treatment range from 70% to 90%.1 There have been reports of dissection recurrence in half of the cases within a period of 2 months.10 Similar numbers are reported in other series, suggesting greater susceptibility in the acute stage of the episode, possibly explained by the overall frailty of the vascular wall. This is reinforced by the observation that more than 40% of pregnant women with spontaneous coronary dissections may have dissections in another vascular territory.1,6
Funding sourceNone.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.