Primary percutaneous coronary intervention (primary PCI) is the preferred reperfusion method in patients with ST-segment elevation myocardial infarction (STEMI). Manual aspiration thrombectomy has been increasingly used and enables the analysis of thrombus aspirates.
MethodsConsecutive patients undergoing primary PCI were enrolled from December 2009 to June 2011. Clinical, laboratory and angiographic data were prospectively collected and entered in a dedicated database. The decision to perform thromboaspiration was left to the discretion of the operators. One hundred and twelve samples of thrombi were collected, stored in 10% formalin-fixed paraffin, stained with hematoxylin-eosin and analyzed by light microscopy. On histopathological evaluation, the thrombi were classified as recent thrombi or lysed/organized thrombi.
ResultsRecent thrombi were identified in 68 patients (61%) and lysed/organized thrombi in 44 patients (39%). Patients with recent thrombi had higher red blood cell infiltration (P=0.03). There were no other statistically significant differences identified for clinical, angiographic, laboratory or clinical outcomes between the two study groups.
ConclusionsIn patients with STEMI undergoing primary PCI, two-thirds of thrombus aspirates showed histopathological features of recent thrombi. There were no significant associations between these characteristics and clinical, laboratory and angiographic data in this contemporary sample representative of the real world.
Avaliação Histopatológica deTrombos Coronários em Pacientes com Infarto Agudo do Miocárdio e Elevação do Segmento ST
IntroduçãoA intervenção coronária percutânea (ICP) primária é o principal método de reperfusão em pacientes com infarto do miocárdio com supradesnivelamento do segmento ST (IAMCSST). A trombectomia por aspiração manual tem sido cada vez mais utilizada e possibilita a análise dos trombos aspirados.
MétodosPacientes consecutivos submetidos a ICP primária foram incluídos no período de dezembro de 2009 a junho de 2011. As características clínicas e laboratoriais e os dados angiográficos foram coletados prospectivamente e incluídos em banco de dados dedicado. A decisão de realizar tromboaspiração ficou a cargo dos operadores. Foram coletadas 112 amostras de trombos, armazenadas em formalina 10%, fixadas em parafina, coradas com hematoxilina-eosina, e analisadas por microscopia óptica. Na avaliação histopatológica, os trombos foram classificados em trombos recentes ou lisados/organizados.
ResultadosForam identificados trombos recentes em 68 pacientes (61%) e trombos lisados/organizados em 44 pacientes (39%). Os pacientes com trombos recentes apresentaram maior infiltração de glóbulos vermelhos (P=0,03). Não foram identificadas outras diferenças estatisticamente significantes em relação às características clínicas, angiográficas e laboratoriais ou aos desfechos clínicos entre os dois grupos estudados.
ConclusõesEm pacientes com IAMCSST submetidos a ICP primária, dois terços dos trombos aspirados apresentaram características histopatológicas de trombos recentes. Não foram observadas associações significativas entre essas características e aspectos clínicos, laboratoriais e angiográficos nesta amostra contemporânea e representativa do mundo real.
Acute ST-segment elevation myocardial infarction (STEMI) is a leading cause of death in Brazil. Manual aspiration thrombectomy is often used because it improves reperfusion and decreases mortality.1−6
In over 95% of cases, STEMI is related to a thrombus overlying an atherosclerotic plaque. Several studies have evaluated the characteristics of thrombi in patients with STEMI. The thrombi vary in size and colour, may be occlusive or non-occlusive, can spread in an antegrade or retrograde manner from the area of rupture, and often show different degrees of organization.
Studies have demonstrated an association among the histopathological characteristics, angioplasty results, and clinical outcomes of the thrombus. 6−12 The avai lable analyses, however, are limited by the length of the inclusion of patients (since the year 2000) and the use of several different mechanical aspiration devices. These characteristics, together with changes in the pharmacological treatment and technical performance of primary percutaneous coronary intervention (PCI) in the last decade, may have influenced these findings.
This study evaluated the association between the histopathological characteristics of thrombus aspirates and the clinical data of patients undergoing primary PCI in the treatment of STEMI in contemporary clinical practice.
METHODSStudy design and Patient PopulationA prospective cohort study with clinical data collected in accordance with the STEMI protocol of a tertiary cardiology hospital began in December of 2009. Thrombi collection occurred from April of 2010 to June of 2011.
The study included consecutive patients treated at the emergency department of the Instituto de Cardiologia do Rio Grande do Sul, Brazil, diagnosed with STEMI, who wished to participate in the study, and who underwent thrombus collection during the primary PCI performed at the discretion of the physician responsible for the procedure. Patients aged < 18 years were excluded.
The project was approved by the Ethics Committee in Research of the Instituto de Cardiologia do Rio Grande do Sul.
All patients were instructed about the study, and those who were enrolled signed an informed consent. Data collection was performed through paper forms prepared by the researchers involved in the study, and the data were stored in a dedicated database using Access software. Data entry was verified by a second researcher.
Thrombus collection and histopathological analysisThe thrombi were collected, stored in formaldehyde and analysed by three pathologists blinded to their clinical characteristics. Among the devices used for aspiration were the Export (Medtronic Vascular Inc. – Santa Rosa, USA), Pronto (Vascular Solutions – Minneapolis, USA), Diver (Invatec – Brescia, Italy), and Thrombuster ® (Kaneka Medix Corporation – Osaka, Japan) catheters. Blood collection was performed at the emergency department and was analysed by the laboratory of the Instituto de Cardiologia.
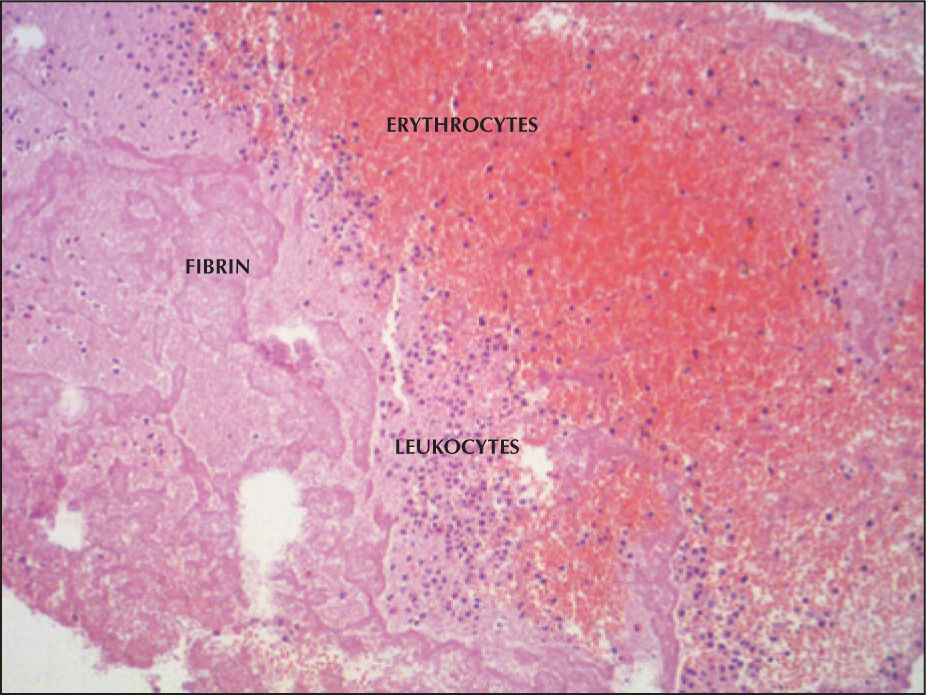
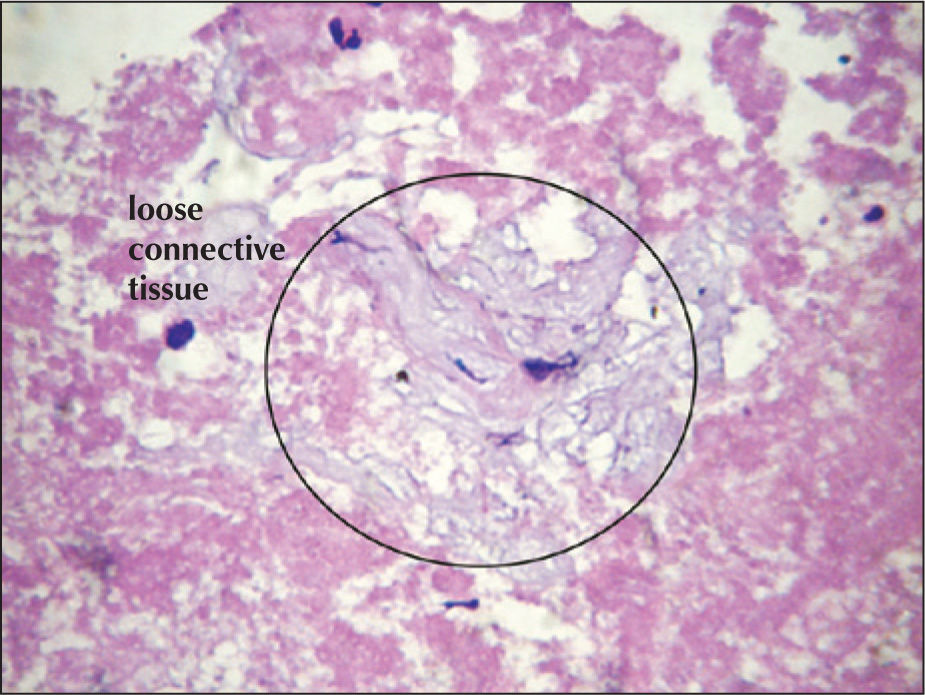
Immediately after thrombus aspiration, the filter device was placed in 10% formalin, aspirated, and fixed for 24 hours. The number of fragments from each aspirated thrombus was recorded. The sample was then embedded in paraffin, submitted to serial histological sections with a thickness of 8 microns, and stained with hematoxylin-eosin. In the histopathological analysis, the thrombi were classified into three groups according to the following previously reported criteria: 3,12 recent thrombi (< one day) composed of patterns of layers of platelets, fibrin, red cells and granulocytes; thrombus lysates (one to five days), characterised by areas of apoptosis, necrosis and leukocytes; and organised thrombi (> five days), showing internal growth of smooth muscle cells and/or connective tissue deposition. The composition of a recent and a non-recent thrombus at the optical microscopy is shown in Figures 1 and 2, respectively. The thrombotic material was classified according to age. In each case, the number of leukocytes, erythrocytes, and fibrin in percentages is also described.
The patients were divided into two groups according to the histological age of the thrombus: recent and lysate/organised. Quantitative variables were expressed as the means±standard deviation or medians (interquartile range). Categorical variables were expressed as absolute and relative frequencies and analysed by chi-squared test or Fisher’s exact test. The significance was set at P < 0.05. The data were analysed using the Statistical Package for Social Sciences (SPSS) software, release 17.0.
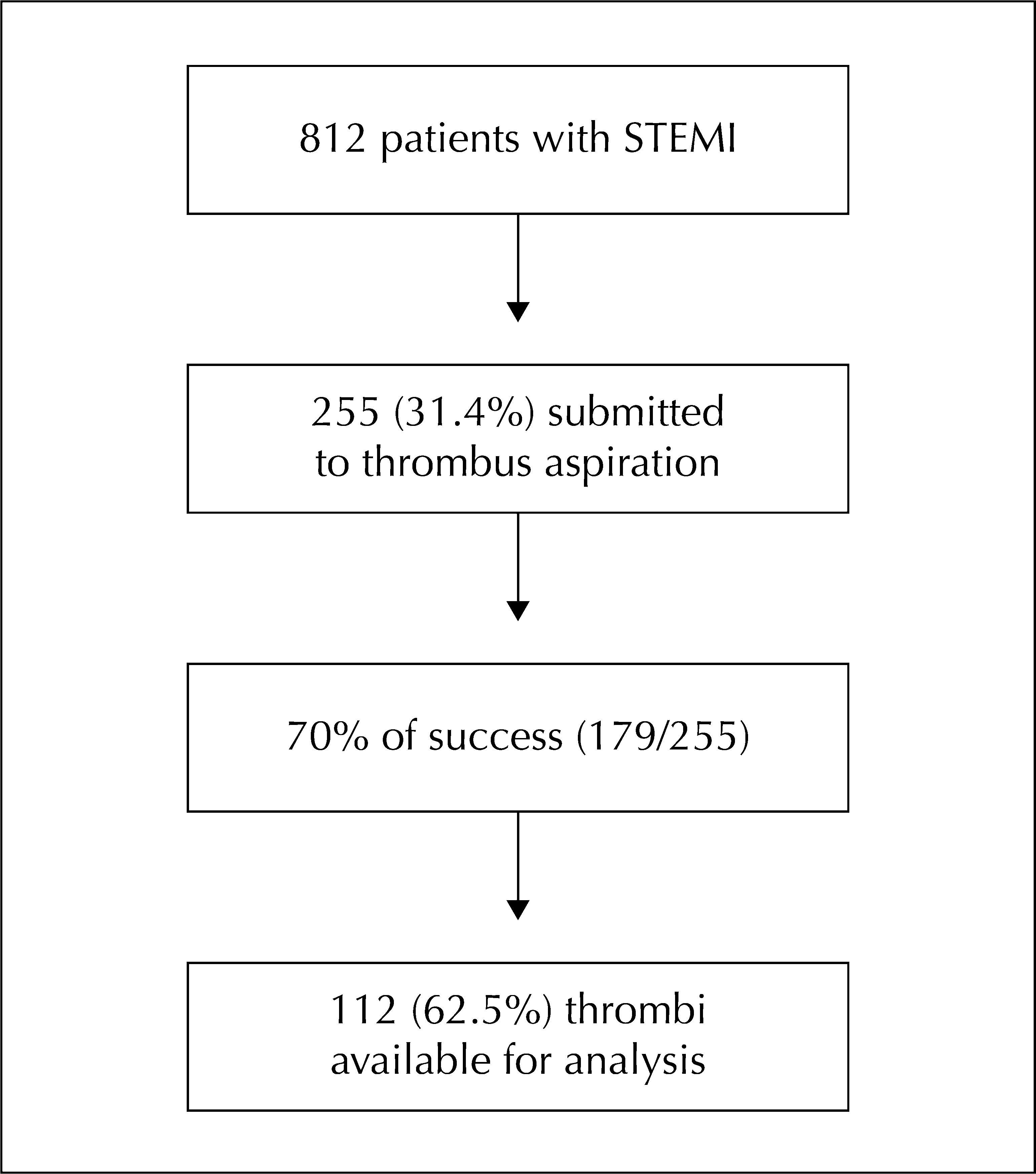
RESULTSDuring the study period, 812 patients with STEMI were evaluated, of whom 255 (31.4%) underwent thrombus aspiration. The success rate was 70% (179/255), and information about the thrombi was available foanalysis in 112 patients (62.5%). The flow chart of thstudy is shown in Figure 3.
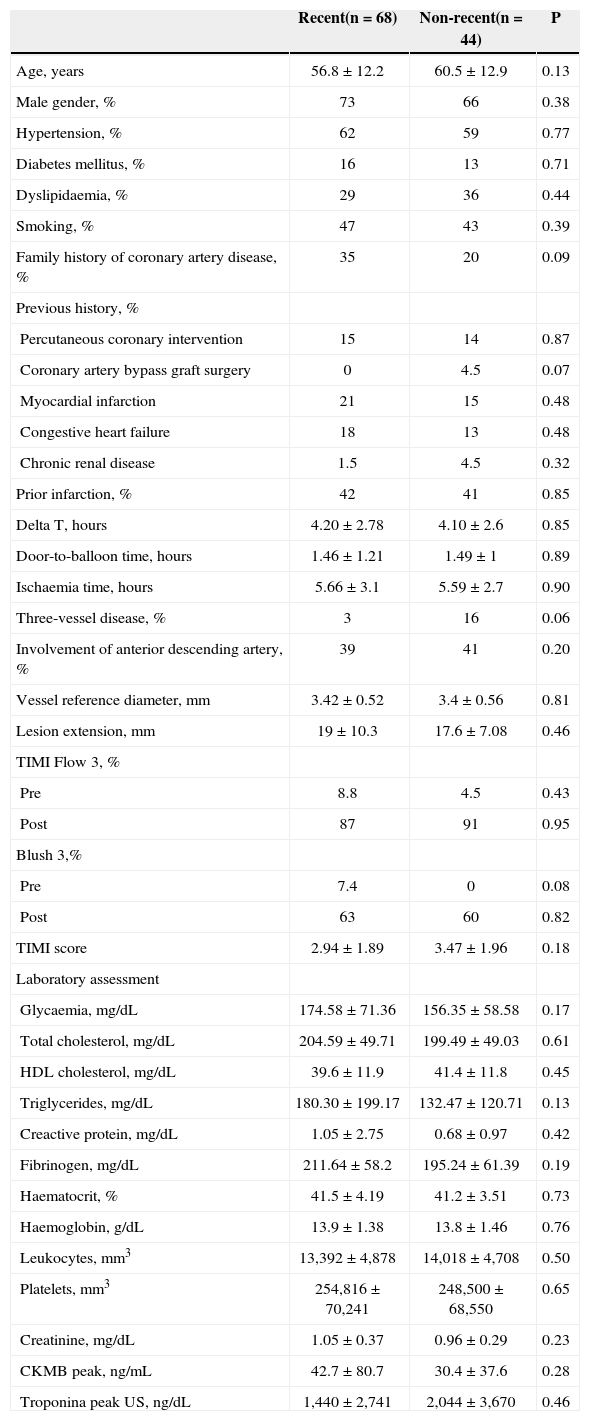
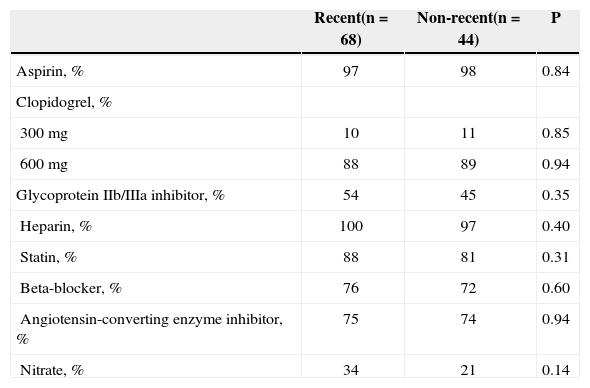
Recent thrombi were identified in 68 patients (61%), and lysed/organised thrombi were found in 44 patient (39%). The angiographic and clinical laboratory results are shown in Table 1, and an associative trend was observed in the recent thrombus groups with a family history of coronary artery disease (P=0.09) and with blush grade 3 pre-PCI (P=0.08). In the group of patients with lysed/organised thrombi, an associative trend was observed with prior coronary artery bypass graft (P=0.07) and with triple vessel coronary artery disease (P=0.06). Regarding the laboratory characteristics, there were no statistically significant differences between the groups. In relation to the medications used during the hospitalisation of both groups of patients, there was no statistically significant difference (Table 2).
Clinical, angiographic and laboratory characteristics
| Recent(n=68) | Non-recent(n=44) | P | |
|---|---|---|---|
| Age, years | 56.8±12.2 | 60.5±12.9 | 0.13 |
| Male gender, % | 73 | 66 | 0.38 |
| Hypertension, % | 62 | 59 | 0.77 |
| Diabetes mellitus, % | 16 | 13 | 0.71 |
| Dyslipidaemia, % | 29 | 36 | 0.44 |
| Smoking, % | 47 | 43 | 0.39 |
| Family history of coronary artery disease, % | 35 | 20 | 0.09 |
| Previous history, % | |||
| Percutaneous coronary intervention | 15 | 14 | 0.87 |
| Coronary artery bypass graft surgery | 0 | 4.5 | 0.07 |
| Myocardial infarction | 21 | 15 | 0.48 |
| Congestive heart failure | 18 | 13 | 0.48 |
| Chronic renal disease | 1.5 | 4.5 | 0.32 |
| Prior infarction, % | 42 | 41 | 0.85 |
| Delta T, hours | 4.20±2.78 | 4.10±2.6 | 0.85 |
| Door-to-balloon time, hours | 1.46±1.21 | 1.49±1 | 0.89 |
| Ischaemia time, hours | 5.66±3.1 | 5.59±2.7 | 0.90 |
| Three-vessel disease, % | 3 | 16 | 0.06 |
| Involvement of anterior descending artery, % | 39 | 41 | 0.20 |
| Vessel reference diameter, mm | 3.42±0.52 | 3.4±0.56 | 0.81 |
| Lesion extension, mm | 19±10.3 | 17.6±7.08 | 0.46 |
| TIMI Flow 3, % | |||
| Pre | 8.8 | 4.5 | 0.43 |
| Post | 87 | 91 | 0.95 |
| Blush 3,% | |||
| Pre | 7.4 | 0 | 0.08 |
| Post | 63 | 60 | 0.82 |
| TIMI score | 2.94±1.89 | 3.47±1.96 | 0.18 |
| Laboratory assessment | |||
| Glycaemia, mg/dL | 174.58±71.36 | 156.35±58.58 | 0.17 |
| Total cholesterol, mg/dL | 204.59±49.71 | 199.49±49.03 | 0.61 |
| HDL cholesterol, mg/dL | 39.6±11.9 | 41.4±11.8 | 0.45 |
| Triglycerides, mg/dL | 180.30±199.17 | 132.47±120.71 | 0.13 |
| Creactive protein, mg/dL | 1.05±2.75 | 0.68±0.97 | 0.42 |
| Fibrinogen, mg/dL | 211.64±58.2 | 195.24±61.39 | 0.19 |
| Haematocrit, % | 41.5±4.19 | 41.2±3.51 | 0.73 |
| Haemoglobin, g/dL | 13.9±1.38 | 13.8±1.46 | 0.76 |
| Leukocytes, mm3 | 13,392±4,878 | 14,018±4,708 | 0.50 |
| Platelets, mm3 | 254,816±70,241 | 248,500±68,550 | 0.65 |
| Creatinine, mg/dL | 1.05±0.37 | 0.96±0.29 | 0.23 |
| CKMB peak, ng/mL | 42.7±80.7 | 30.4±37.6 | 0.28 |
| Troponina peak US, ng/dL | 1,440±2,741 | 2,044±3,670 | 0.46 |
CKMB=creatine-kinase MB fraction; HDL=high-density lipoprotein; TIMI=Thrombolisys In Myocardial Infarction.
Medications administered within the first 24 hours of hospital admission
| Recent(n=68) | Non-recent(n=44) | P | |
|---|---|---|---|
| Aspirin, % | 97 | 98 | 0.84 |
| Clopidogrel, % | |||
| 300mg | 10 | 11 | 0.85 |
| 600mg | 88 | 89 | 0.94 |
| Glycoprotein IIb/IIIa inhibitor, % | 54 | 45 | 0.35 |
| Heparin, % | 100 | 97 | 0.40 |
| Statin, % | 88 | 81 | 0.31 |
| Beta-blocker, % | 76 | 72 | 0.60 |
| Angiotensin-converting enzyme inhibitor, % | 75 | 74 | 0.94 |
| Nitrate, % | 34 | 21 | 0.14 |
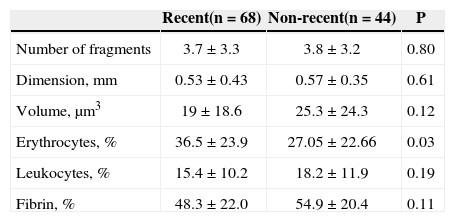
Regarding the histopathological data, a greater erythrocyte infiltration was observed in patients with recent thrombi (P=0.03). There were no statistically significant differences in the number of aspirated fragments, size and volume of the thrombi, and infiltration of the leukocytes and fibrin (Table 3).
Histopathological Characteristics
| Recent(n=68) | Non-recent(n=44) | P | |
|---|---|---|---|
| Number of fragments | 3.7±3.3 | 3.8±3.2 | 0.80 |
| Dimension, mm | 0.53±0.43 | 0.57±0.35 | 0.61 |
| Volume, μm3 | 19±18.6 | 25.3±24.3 | 0.12 |
| Erythrocytes, % | 36.5±23.9 | 27.05±22.66 | 0.03 |
| Leukocytes, % | 15.4±10.2 | 18.2±11.9 | 0.19 |
| Fibrin, % | 48.3±22.0 | 54.9±20.4 | 0.11 |
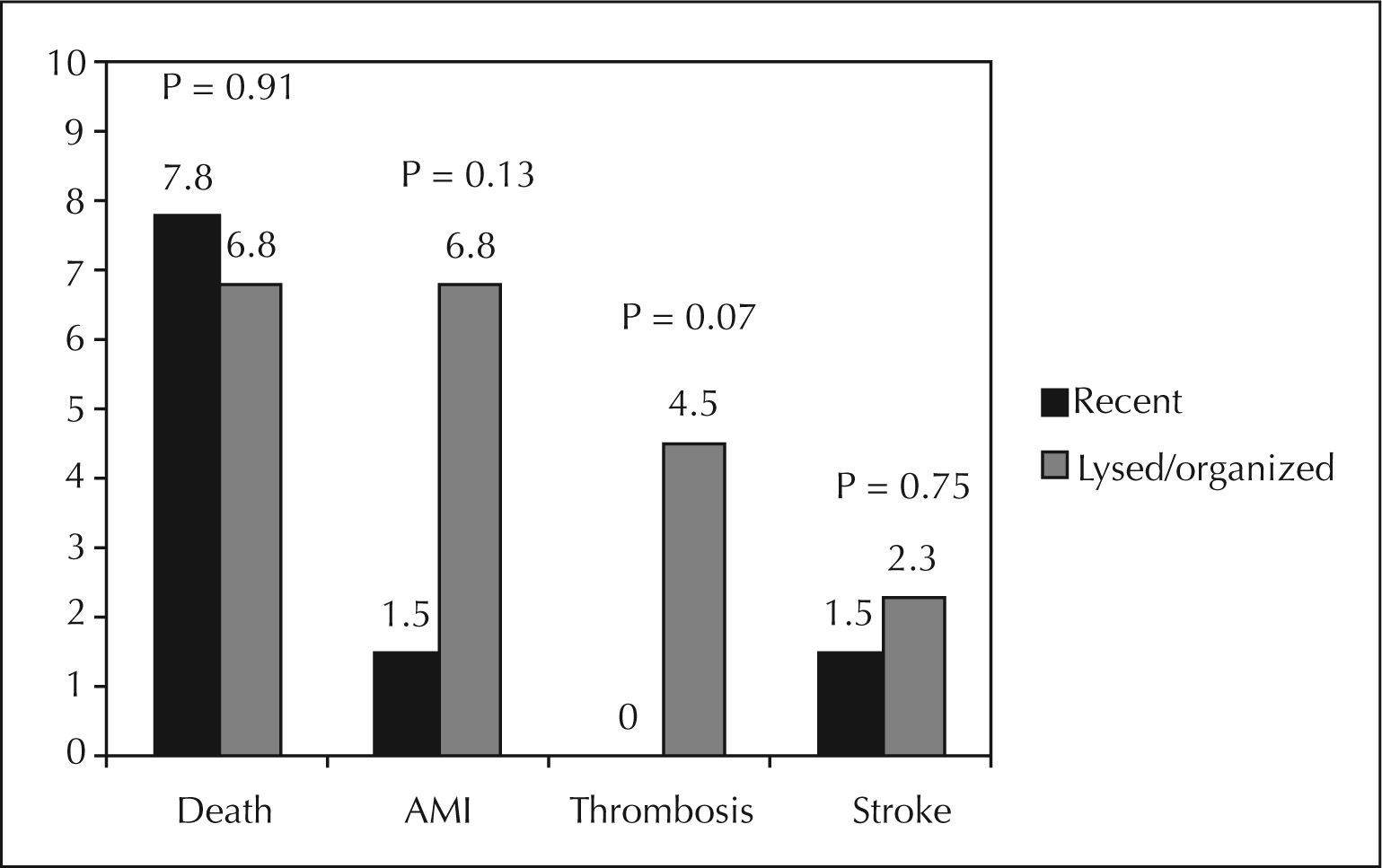
The major cardiovascular outcomes over the 30-day follow-up are shown in Figure 4. There were no statistically significant differences, but patients with recent thrombi tended to have higher rates of postimplant stent thrombosis.
DISCUSSIONIn the present study, the histopathological findings of coronary thrombi in patients undergoing primary PCI for artery recanalisation related to STEMI are described, as well as their correlations with clinical and laboratory data, aspects related to treatment and clinical outcomes. Although the study predominantly included patients with a time of pain onset < 12 hours, old thrombi were identified in approximately one-third of the cases, demonstrating that the process of thrombosis may begin hours before the onset of symptoms and complete vessel occlusion, as had been previously reported in other studies.3,13−17 Moreover, no statistically significant associations were identified among the histopathological characterizations of the thrombus age and outcomes, time of symptom onset or other clinical and angiographic variables. To the authors’ knowledge, this is the first study in Brazil to evaluate the histopathological characteristics of patients with STEMI undergoing primary PCI.
Previous studies have evaluated the associations between the age of thrombi through histopathological evaluation and clinical, laboratory, or angiographic findings. 3,7,8 In a report on 959 patients with STEMI undergoing primary PCI, recent thrombi were present in 60% of the cases, and lysed or arranged thrombi were present in 40%, which is consistent with the findings of the present study. The distal embolization in this study was the only clinical aspect that had a statistically significant association with the presence of recent thrombi. 13
In another report with 99 samples of thrombus aspirates, there were 31 cases of organized thrombi (16%), 70 cases of lysed thrombi (35%), and 98 cases of recent thrombi (49%); the age of the thrombus was related to the patient’s age, male gender, and the extent of the lesion. 3 In a study with electrocardiographic correlation, an association was demonstrated between the incomplete recovery of the ST-segment and the presence of old thrombi, and this electrocardiographic alteration was a strong predictor of long-term mortality, regardless of the histopathology of the thrombi aspirates. 7 Finally, in an analysis with a long follow-up, there was an increase in mortality at four years in patients with old thrombi, compared to those with recent thrombi. 13
While each study had a significant number of patients, the aforementioned studies are limited by the length of time that they included patients (since the year 2000) and the use of different mechanical aspiration devices. These characteristics might have influenced the results due to changes in pharmacological treatment and primary PCI techniques over the last decade. The use of mechanical aspiration devices could alter the histopathological characteristics of the thrombi, thereby influencing these analyses when compared to those performed with manual aspiration devices. In the present study, no association was observed between the thrombus age according to the proposed histopathological classification and clinical, angiographic or laboratory data. Although the present study had a smaller population than that of the Dutch group studies, it used only manual aspiration, which is currently the most commonly used technique; furthermore, the present data were recently collected, through a method representative of the real world.
During the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS), the histopathological analysis confirmed successful aspiration in 73% of patients. These thrombi were predominantly composed of platelets (recent thrombi), which is common in patients with STEMI. In that study, platelet thrombi were mainly small or moderate in size, whereas erythrocyte-rich thrombi were of moderate to large size. 16
The acute arterial occlusion that determines STEMI is one of the final events in the progression of atherosclerotic plaques before the rupture or erosion phases, and these morphological alterations can occur days to weeks before the symptoms. 18,20 It is possible that the continued inflammatory activity in atheromatous plaques is closely related to the rate of formation or propagation of coronary thrombi. In the present study, no association was found between C-reactive protein, a validated marker of inflammatory activity, and the histopathological characteristics of the thrombi.
The length of the thrombus may be another important factor in determining thrombotic burden. Maturation occurs more rapidly at the end segments through the formation of granulation tissue, while the medial segments remain platelet- and fibrin-rich. 1,12,21 The authors reported that the largest dimension and greatest volume of samples evaluated were related to the age of the thrombus (P=0.01 and P=0.04, respectively). Kraemer et al. 13 and Rittersma et al. 3 reported that older thrombi were identified in 79 of 115 (69%) patients, as well as that women more often showed erosion and had a higher prevalence of non-recent thrombi (44 of 50, 88%) that ruptured (35 of 65, 54%, P < 0.001).
CONCLUSIONSIn patients with STEMI undergoing primary PCI, two-thirds of thrombus aspirates presented histopathological features consistent with recent thrombi. However, there were no significant associations between these characteristics and clinical, laboratory, or angiographic aspects in this contemporary, representative sample from the real world.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.