Diabetes mellitus is associated with increased mortality rates in the setting of acute myocardial infarction. The aim of this study was to evaluate whether there are peculiarities in the atherothrombotic process that might be implicated in increased risk for this outcome in patients with diabetes.
MethodsPilot study in a cohort of patients with ST-elevation acute myocardial infarction undergoing primary percutaneous coronary intervention and aspiration thrombectomy. Clinical and laboratory variables were evaluated in all of the cases. Thrombi were analyzed for histopathological features as well as immunohistochemical expression of CD34, CD61 and factor VIII.
ResultsOur sample included the first ten diabetic patients with material available for analysis, who were matched according to age, gender and time elapsed since myocardial infarction with ten patients without diabetes. There was no significant association between the immunohistochemical expression of CD34, CD61 and factor VIII with other histopathological, clinical and laboratory variables, including the presence of diabetes mellitus.
ConclusionsIn this preliminary analysis, it was not possible to demonstrate any significant difference in the expression of endothelial cell activity, platelet function and activation of the coagulation cascade between thrombi of patients with and without diabetes undergoing primary coronary intervention.
Características Imuno-Histoquímicas de Trombos Coronarianos de Pacientes com Infarto do Miocárdio com Elevação de ST e Diabetes Mellitus: Estudo Piloto
IntroduçãoNo contexto do infarto agudo do miocárdio, o diabetes mellitus está associado à maior mortalidade. O objetivo deste estudo foi avaliar se existem, entre os diabéticos, peculiaridades no processo de aterotrombose que poderiam estar implicadas em maior risco para tal desfecho.
MétodosEstudo piloto, proveniente de coorte de pacientes com diagnòstico de infarto agudo do miocárdio com elevação do segmento ST submetidos à intervenção coronária percutânea primária e à tromboaspiração. Foram estudadas variáveis clínico-laboratoriais de cada caso. Os trombos foram analisados quanto às características histopatológicas e às expressöes imuno-histoquímicas de CD34, CD61 e fator VIII.
ResultadosForam incluídos os primeiros dez pacientes portadores de diabetes mellitus com material disponível para análise, pareados por idade, sexo e tempo de evolução do infarto com dez pacientes sem diabetes mellitus. Não houve associação significativa entre as expressões imuno-histoquímicas de CD34, CD61 e fator VIII com relação às variáveis histopatológicas, laboratoriais e clínicas estudadas, inclusive com relação à presença de diabetes mellitus.
ConclusõesEm análise preliminar, não foi possível demonstrar diferença significativa quanto à expressão da atividade de células endoteliais, da função plaquetária e da ativação da cascata de coagulação entre trombos de pacientes com e sem o diagnóstico de diabetes mellitus submetidos à intervenção coronariana primária.
Coronary artery disease (CAD) is the leading cause of death worldwide, with most adverse events being associated with the occurrence of acute myocardial infarction (AMI).1 With the optimization of antithrombotic therapies and reperfusion, a decrease in mortality from acute myocardial infarction with ST-segment elevation (STEMI) has been observed.2 However, efforts are required to improve the management of this condition, as high rates of mortality have still been reported.3 In most cases, STEMI is caused by the rupture of vulnerable atherosclerotic plaques associated with inflammatory activity and a dysfunctional endothelium. The ruptured plaque is the trigger for platelet activation and aggregation, and thrombin formation, resulting in total occlusion of the coronary artery by the thrombus.4
Primary percutaneous coronary intervention (PPCI) is considered the preferred method of reperfusion in AMI.5 In recent years, the adjunct thrombo aspiration technique has been increasingly used, with improvement in angiographic results and clinical outcomes in some studies.6 Additionally, thrombus removal has allowed for a new line of research regarding the analysis of the morphology, histology, and factors associated with different types of thrombi.7–9 Variables, such as red color and thrombus chronology, have been associated with increased mortality,10,11 but the physiopathological role of the different elements that constitute the thrombus has been seldom studied.
Immunohistochemical analysis of thrombus aspirates can be an important complementary tool in the search for these answers. The expression of the endothelial cell activity, of platelet function, of and coagulation cascade activation can be estimated by the immunohistochemical expression of the antigens CD34, CD61, and factor VIII, respectively.12–15 In the scenario of STEMI, few studies have evaluated the im-munohistochemical profile of intracoronary thrombus in vivo and its correlation with clinical variables.13–16 In this context, the importance of diabetes mellitus (DM) is well-known, either by increasing the risk of CAD and thrombosis, or because it is associated with higher mortality in STEMI.17,18 However, there are doubts as to whether this risk is mediated by differences in the physiopathological processes of atherothrombosis or by the increase in comorbidities associated with DM. Thus, this study aimed to evaluate the immunohistochemical expression of the antigens CD34, CD61, and factor VIII in coronary thrombi in patients with DM and STEMI.
METHODSPatientsThis was a pilot study of sample of patients consecutively admitted to this hospital with a diagnosis of STEMI, between December 2010 and November 2012. STEMI was defined as chest pain at rest lasting more than 30 minutes, associated to ST-segment elevation of at least 1mm in two contiguous leads in the frontal plane, or at least 2mm in the horizontal plane, or associated with new left bundle branch block. Patients with evolution>12 hours, younger than 18 years, or those who refused to participate in the study were excluded.
All participants signed an informed consent. The study was approved by the Ethics Committee in Research of Instituto de Cardiologia, Fundação Universitária de Cardiologia, Porto Alegre (RS), Brazil.
Clinical characteristics and follow-upAll patients were prospectively evaluated regarding their clinical and demographic characteristics by one of the researchers. The clinical, laboratory, and angiographic variables were recorded in a dedicated database. During hospitalization, the patients were followed daily by one of the investigators for verification of in-hospital events. After hospital discharge, patients were contacted by telephone or assisted at the outpatient clinic for outcome assessment.
Percutaneous coronary intervention proceduresAt admission, all patients received 300mg of ace-tylsalicylic acid and 300 to 600mg of clopidogrel. For the performance of the PPCI procedure, 60 to 100 U/kg of unfractionated heparin were administered. PPCI procedures were performed as recommended in the literature.19,20 Decisions regarding technical aspects of the procedure, such as access route (radial or femoral), whether or not to perform thromboaspiration, type and number of stents, and use of glycoprotein 11b/111a inhibitors were left to the discretion of the surgeons. Regarding thromboaspiration, three different catheters were used: Export (Medtronic Vascular Inc, Santa Rosa, CA, United States), Diver (Invatec, Brescia, Italy), or Pronto (Vascular Solutions, Minneapolis, MN, United States). In all cases, the aspirations were performed prior to balloon inflation, passing more than once through the site of occlusion. The aspirated blood and intracoronary material were retained on a filter.
Thrombus analysisImmediately after thrombus removal from the coronary artery, the sample was embedded in 10% formalin and fixed in paraffin for 24 hours. The specimens were cut with a microtome and stained with the hematoxylin-eosin method for histopathological analyses, which were performed by a pathologist blinded to the clinical characteristics of patients. The following characteristics of the thrombi were studied: volume (cm3), color (white or red), microscopic pattern (recent, with lysis, or in formation) and the percentage of leukocytes, fibrin, and erythrocytes, as well as the immunohistochemical expression of CD34, CD61, and factor VIII. Recent thrombi were characterized by the presence of fibrin, leukocytes, and erythrocytes. Thrombi with lysis were characterized by the occurrence ofleukocyteapoptosis. As for thrombi in formation, they were characterized by the formation of loose connective tissue.7
For the immunehistochemistry analysis, 3-μm tissue sections were obtained, which were placed on silanized slides. To perform the immunehistochemistry analysis, each slide was submitted to deparaffinization, using xylene and hydration with ethanol. Antigen retrieval was performed in a microwave oven with a 10mM/pH6.0 citric acid solution, in two cycles of nine minutes each, at 750W. The blocking of endogenous peroxidase was performed with the use of 3% hydrogen peroxide (10 volumes). The primary antibody was diluted in 1% albumin and 0.1% sodium azide in PBS (phosphate-buffered saline), incubated in a moist chamber for 30 minutes at 37°C, and then the material was kept under refrigeration at 4°C for 18 hours. The biotinylated secondary antibody was incubated in a moist chamber at 37° C, for 30 minutes, as well as the streptavidin-biotin-peroxidase complex (StreptABC). The chromogenic substrate used was 60mg diaminobenzidine in PBS, and Harris hematoxylin was used as counter-stain. The following antibodies were used (Dako Corporation or Novocastra): CD34, CD61, and von Willebrand factor (factor VIII). In all cases, an immunehistochemistry panel was created. The expression obtained by blood cells and/or components of the specimen was revealed by the presence of brown staining in different areas of the sample. A strong positive expression was considered when the immunohistochemistry reaction showed strong and diffuse brown staining in several cells of the analyzed tissue. Moderate positive expression was defined when the immunohistochemistry reaction showed amoderately intense brown (light brown) staining in some cells of the analyzed tissue.
Statistical AnalysisData were analyzed using SPSS for Windows, considering significant values when p<0.05. Quantitative variables were expressed as mean±standard deviation or as median and interquartile range (25-75%). Categorical variables were expressed as absolute and relative frequency, analyzed by the chi-squared or Fisher’s exact test. The cellular infiltrate was analyzed using a semiquantitative scale.
RESULTSDuring the study period, 310 patients were successfully submitted to thromboaspiration (Thrombolysis in Myocardial Infarction [TIMI] 3 flow and thrombus-recovery). In this analysis, the first ten patients with DM with material available for analysis, which were matched for age, gender, and time of infarction with ten patients without diabetes, were included in the study. In both groups, 60% of the sample were males, aged 55±6 years and 56.5±5.8years, respectively, and with median time of AMI evolution of 3.9hours (2.0 to 9.0hours) and 3.7hours (2.8 to 9.3hours), respectively.
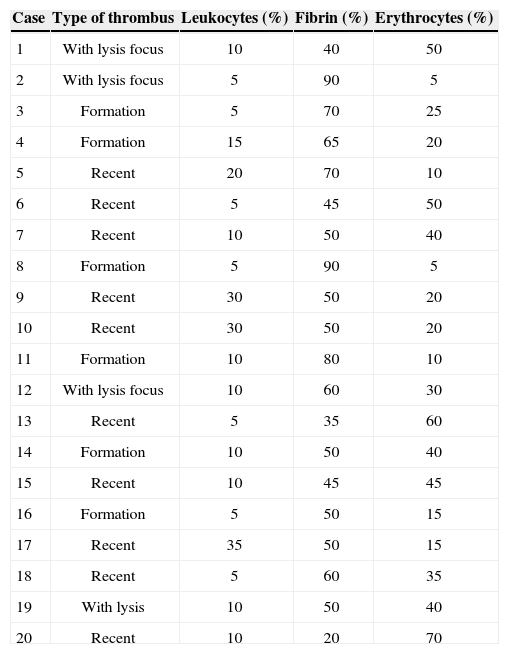
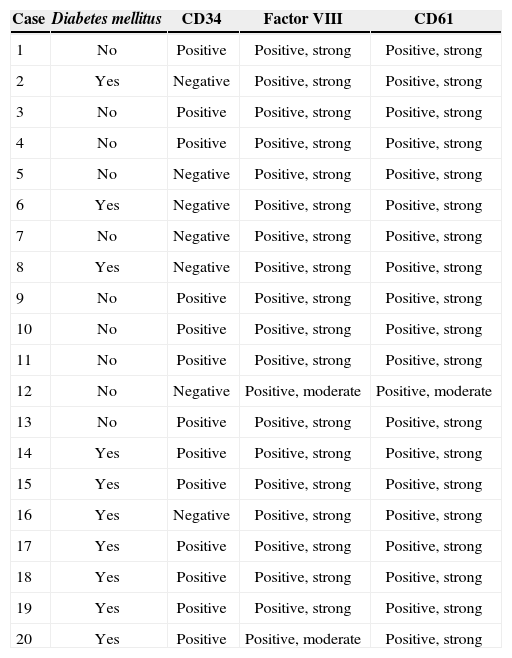
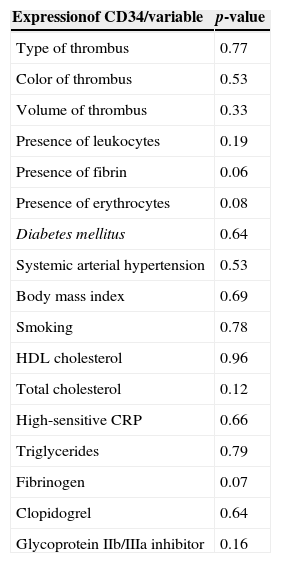
The histopathological profile is shown in Table 1, and the immunohistochemical profile in Table 2. Regarding CD34 expression, there was a trend of association with presence of fibrin in thrombus and higher serum levels of fibrinogen. There was no association with other clinical, laboratory, or histological characteristics (Table 3).
Histopathological characteristics of thrombi in the study patients
| Case | Type of thrombus | Leukocytes (%) | Fibrin (%) | Erythrocytes (%) |
|---|---|---|---|---|
| 1 | With lysis focus | 10 | 40 | 50 |
| 2 | With lysis focus | 5 | 90 | 5 |
| 3 | Formation | 5 | 70 | 25 |
| 4 | Formation | 15 | 65 | 20 |
| 5 | Recent | 20 | 70 | 10 |
| 6 | Recent | 5 | 45 | 50 |
| 7 | Recent | 10 | 50 | 40 |
| 8 | Formation | 5 | 90 | 5 |
| 9 | Recent | 30 | 50 | 20 |
| 10 | Recent | 30 | 50 | 20 |
| 11 | Formation | 10 | 80 | 10 |
| 12 | With lysis focus | 10 | 60 | 30 |
| 13 | Recent | 5 | 35 | 60 |
| 14 | Formation | 10 | 50 | 40 |
| 15 | Recent | 10 | 45 | 45 |
| 16 | Formation | 5 | 50 | 15 |
| 17 | Recent | 35 | 50 | 15 |
| 18 | Recent | 5 | 60 | 35 |
| 19 | With lysis | 10 | 50 | 40 |
| 20 | Recent | 10 | 20 | 70 |
Immunohistochemical panel
| Case | Diabetes mellitus | CD34 | Factor VIII | CD61 |
|---|---|---|---|---|
| 1 | No | Positive | Positive, strong | Positive, strong |
| 2 | Yes | Negative | Positive, strong | Positive, strong |
| 3 | No | Positive | Positive, strong | Positive, strong |
| 4 | No | Positive | Positive, strong | Positive, strong |
| 5 | No | Negative | Positive, strong | Positive, strong |
| 6 | Yes | Negative | Positive, strong | Positive, strong |
| 7 | No | Negative | Positive, strong | Positive, strong |
| 8 | Yes | Negative | Positive, strong | Positive, strong |
| 9 | No | Positive | Positive, strong | Positive, strong |
| 10 | No | Positive | Positive, strong | Positive, strong |
| 11 | No | Positive | Positive, strong | Positive, strong |
| 12 | No | Negative | Positive, moderate | Positive, moderate |
| 13 | No | Positive | Positive, strong | Positive, strong |
| 14 | Yes | Positive | Positive, strong | Positive, strong |
| 15 | Yes | Positive | Positive, strong | Positive, strong |
| 16 | Yes | Negative | Positive, strong | Positive, strong |
| 17 | Yes | Positive | Positive, strong | Positive, strong |
| 18 | Yes | Positive | Positive, strong | Positive, strong |
| 19 | Yes | Positive | Positive, strong | Positive, strong |
| 20 | Yes | Positive | Positive, moderate | Positive, strong |
Association between CD34 expression and clinical-laboratory and histological variables
| Expressionof CD34/variable | p-value |
|---|---|
| Type of thrombus | 0.77 |
| Color of thrombus | 0.53 |
| Volume of thrombus | 0.33 |
| Presence of leukocytes | 0.19 |
| Presence of fibrin | 0.06 |
| Presence of erythrocytes | 0.08 |
| Diabetes mellitus | 0.64 |
| Systemic arterial hypertension | 0.53 |
| Body mass index | 0.69 |
| Smoking | 0.78 |
| HDL cholesterol | 0.96 |
| Total cholesterol | 0.12 |
| High-sensitive CRP | 0.66 |
| Triglycerides | 0.79 |
| Fibrinogen | 0.07 |
| Clopidogrel | 0.64 |
| Glycoprotein IIb/IIIa inhibitor | 0.16 |
HDL, high-density lipoprotein
CRP, C-reactive protein.
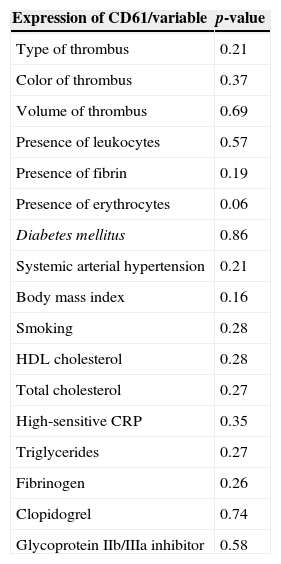
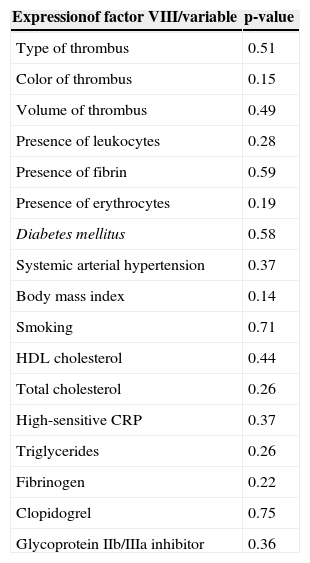
The association between the expression of CD61 antibodies and factor VIII and the analyzed variables (Tables 4 and 5) showed no statistically significant differences, except for a trend of association between the expression of CD61 antibodies and the presence of erythrocytes in the thrombus.
Association between the expression of CD61 and clinical-laboratory and histological variables
| Expression of CD61/variable | p-value |
|---|---|
| Type of thrombus | 0.21 |
| Color of thrombus | 0.37 |
| Volume of thrombus | 0.69 |
| Presence of leukocytes | 0.57 |
| Presence of fibrin | 0.19 |
| Presence of erythrocytes | 0.06 |
| Diabetes mellitus | 0.86 |
| Systemic arterial hypertension | 0.21 |
| Body mass index | 0.16 |
| Smoking | 0.28 |
| HDL cholesterol | 0.28 |
| Total cholesterol | 0.27 |
| High-sensitive CRP | 0.35 |
| Triglycerides | 0.27 |
| Fibrinogen | 0.26 |
| Clopidogrel | 0.74 |
| Glycoprotein IIb/IIIa inhibitor | 0.58 |
Association between factor VIII expression and clinical-laboratory and histological variables
| Expressionof factor VIII/variable | p-value |
|---|---|
| Type of thrombus | 0.51 |
| Color of thrombus | 0.15 |
| Volume of thrombus | 0.49 |
| Presence of leukocytes | 0.28 |
| Presence of fibrin | 0.59 |
| Presence of erythrocytes | 0.19 |
| Diabetes mellitus | 0.58 |
| Systemic arterial hypertension | 0.37 |
| Body mass index | 0.14 |
| Smoking | 0.71 |
| HDL cholesterol | 0.44 |
| Total cholesterol | 0.26 |
| High-sensitive CRP | 0.37 |
| Triglycerides | 0.26 |
| Fibrinogen | 0.22 |
| Clopidogrel | 0.75 |
| Glycoprotein IIb/IIIa inhibitor | 0.36 |
HDL, high-density lipoprotein
CRP, C-reactive protein.
In this pilot study, there was no significant association between the immunohistochemical expression of CD34, CD61, and factor VIII proteins with the analyzed histopathological, laboratory and clinical variables, including the presence of DM. There was, however, a trend of association of CD34 expression with fibrin content in the thrombus and higher levels of serum fibrinogen, as well as a trend of association between CD61 expression and the presence of erythrocytes.
Different authors have proposed immunohistochem- istry techniques as an additional tool for histopatho- logical analysis, in order to increase the sensitivity for recognition of thrombus-forming components, either at vascular or cavity level, using surgically extracted specimens or those obtained from autopsies.12,21 Such studies, when performed in patients with acute coronary syndromesin vivo, are scarce in the literature.13,15,16,22
Ikuta et al.22 compared material extracted from individuals with stable angina vs. patients with unstable angina, and found higher platelet aggregation and activation in the second group, demonstrated respectively, by increased immunoreactivity of glycoprotein IIb/IIIa (p<0.0005) and P-selectin (p<0.0001). A higher concentration of neutrophils was also identified in the plaques of unstable patients. In another study, which evaluated thrombi in the context of STEMI treated by mechanical reperfusion, a negative correlation between platelet content and the time elapsed since the onset of pain was demonstrated. Furthermore, the rate of cells expressing CD34 showed a positive correlation with restenosis in the follow-up (correlation coefficient=0.76, p=0.01).13
In a recent study, which highlighted the potential practical applicability of a greater knowledge of thrombus structure, Sambola et al.15 assessed the thrombotic burden in aspirates from ten patients undergoing PPCI, compared to ten patients undergoing rescue PCI after ineffective response to tenecteplase. In the latter group of patients, higher levels of fibrin (p=0.016), P-selectin (p=0.03), and von Willebrand factor (p=0.03) were detected.
Although evidence indicates increased platelet reactivity and coagulability, as well asimpaired fibrinolysis in patients with type 2DM,23 the immunehistochemical profile of the present diabetic patients was not different from that of non-diabetics, even after matching the groups for important confounding factors, such as age, gender, and time of STEMI evolution. These findings were also different from the results found by Yamashita et al.,16 who observed a significantly lower number of CD34 positive cells in thrombi of patients with type 2DM. It is believed that this cell grouping can inhibit the formation and facilitate thrombus organization, so that its shortage may negatively impact the prognosis. Furthermore, no associations with statistical significance were observed between the CD34, CD61, or factor VIII antigens and other clinical variables or components of the thrombus.
The main limitation of this pilot study was its small sample, which may have contributed to the lack of difference between groups. Conversely, the publication of these results can alert researchers and interventionists to the importance of immunohistochemical analysis in coronary thrombi in patients with STEMI.
CONCLUSIONSIn this preliminary analysis, it was not possible to demonstrate any significant differences regarding the expression of endothelial cell activity, platelet function, and coagulation cascade activation between thrombi of diabetic and non-diabetic patients undergoing primary coronary intervention and treatment of acute myocardial infarction with ST-segment elevation.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCEThis work was funded by Instituto de Cardiologia/Fundação Universitária de Cardiologia (IC/FUC), Porto Alegre (RS), through Fundo de Apoio do IC/FUC à Ciência e à Cultura (FAPICC).
ACKNOWLEDGMENTSThe authors would like to thank their colleagues Azmus Alexandre, André Mânica, Carlos Cardoso, Claudio Vasques de Moraes, Cláudio de Moraes Ramos, Cristiano Cardoso, Leboute Flavio Henrique Gomes, Julio Teixeira, La Hore Rodrigues, Luis Maria Yordi, Mauro Moura, and Rogerio Sarmento Leite, for their participation in the primary percutaneous coronary intervention procedures.
Instituto de Cardiologia/Fundação Universitária de Cardiologia, Porto Alegre, RS, Brazil.