Invasive cardiac procedures expose patients and physicians to the risks of ionizing radiation. The aim of this study is to determine the impact of body weight on radiation exposure during cardiac procedures.
METHODSProspective cohort study including patients undergoing cardiac catheterization or percutaneous coronary intervention (PCI) between August 2010 and December 2011. Clinical, angiographic and radiation exposure characteristics were recorded in a dedicated database. Patterns of radiation exposure were established in three groups: A (≤79kg), B (80–99kg) and C (≥100kg). Data were analyzed by SPSS version 18.0 and results were shown as mean, standard deviation, percentage, percentile and interquartile interval. Independent predictors of increased radiation exposure were identified by multiple logistic regression analysis.
RESULTSSample included 671 patients, of which 363 in group A, 252 in group B and 56 in group C. Mean dose of radiation exposure was 484.29mGy, 735.69mGy and 900.36mGy for groups A, B and C, respectively (P<0.001). The median dose area product was 29.327mGy.cm2, 43.319mGy.cm2 and 57.987mGy.cm2 for groups A, B and C, respectively (P<0.001). Predictors of increased radiation exposure were weight [odds ratio (OR) 1.03, confidence interval (CI) 1.01−1.05; P=0.003], elective PCI (OR 11.9, CI 4.26−33.24; P<0.001) and ad hoc PCI (OR 15.46, CI 5.44−43.87; P<0.001).
CONCLUSIONSPatient weight has a significant impact on radiation exposure during invasive cardiac procedures. Overweight patients are significantly more exposed to higher doses of ionizing radiation.
Impacto do Peso Corporal dosPacientes na Exposição Radiológica Durante Procedimentos Cardiológicos Invasivos
IntroduçãoProcedimentos cardiológicos invasivos expõem pacientes e médicos aos riscos da radiação ionizante. É objetivo deste estudo determinar o impacto do peso do paciente na exposição radiológica durante procedimentos cardiológicos.
MétodosEstudo de coorte prospectivo incluindo pacientes submetidos a cateterismo cardíaco ou intervenção coronária percutânea (ICP) entre agosto de 2010 e dezembro de 2011. Características clínicas, angiográficas e de exposição à radiação foram registradas em banco de dados específico. Os padrões de exposição à radiação foram determinados em três grupos: A (≤79 kg), B (80–99 kg) e C (≥100 kg). Os dados foram analisados em programa SPSS 18.0, sendo os resultados apresentados em média, desvio padrão, porcentual, percentil e intervalo interquartil. Preditores independentes de exposição à radiação aumentada foram identificados por análise de regressão logística múltipla.
ResultadosA amostra incluiu 671 pacientes, sendo 363 no grupo A, 252 no B e 56 no C. A dose média de radiação recebida pelos pacientes foi de 484,29mGy, 735,69mGy e 900,36mGy para os grupos A, B e C, respectivamente (P < 0,001). A mediana do produto dose área foi de 29.327mGy.cm2, 43.319mGy.cm2 e 57.987mGy.cm2 para os grupos A, B e C, respectivamente (P < 0,001). Os preditores de exposição radiológica aumentada foram peso [razão de chance (RC) 1,03, intervalo de confiança (IC) 1,01-1,05; P = 0,003], ICP eletiva (RC 11,9, IC 4,26-33,24; P < 0,001) e ICP ad hoc (RC 15,46, IC 5,44-43,87; P < 0,001).
ConclusõesO peso exerce impacto significativo na exposição radiológica em procedimentos cardiológicos invasivos. Pacientes com peso elevado são significativamente mais expostos à radiação ionizante.
Haemodynamic monitoring procedures have been widely used to evaluate coronary artery disease. Concurrently, the number of diagnostic and therapeutic procedures in modern cardiology has increased the exposure to ionising radiation for patients, physicians, and nurses.1,2 Together with increasing technological advances and more potent haemodynamic monitoring equipment,3,4 reports on the harmful effects of ionising radiation have increased.5,6
It is known that patient weight is directly related to unfavourable outcomes, such as vascular complications, in interventional cardiology.7 Nevertheless, few reports exist in the Brazilian national literature about the relation between weight and radiation exposure.
The aim of this study was to determine the impact of body weight on the radiation exposure of patients undergoing invasive cardiac procedures.
METHODSDesignThis was an observational study with prospective data collection.
RADIAÇÃO RegistryThe RADIAÇÃO registry8 is an institutional registry aimed at documenting the diagnostic and therapeutic procedures performed with the help of flat detectors in the field of interventional cardiology. Information regarding radiation exposure and technical details of the procedures are prospectively registered.
SamplePatients underwent, diagnostic cardiac catheterisation or coronary intervention were followed to register the radiation exposure patterns. All patients signed an informed consent, and the protocol was approved by the local research ethics committee.
Analysed characteristicsFor the RADIAÇÃO registry, data regarding patient age, gender, risk factors for cardiovascular disease (diabetes, arterial hypertension, tobacco smoking, dyslipidemia, and family history), clinical presentation and procedure indication, ventricular function, number of vessels affected, treated vessels, lesion characteristics, and success index were collected and analysed. Specific data concerning radiation exposure (received dose, dose area product, and fluoroscopy time) were also collected.
Parameters of radiation exposureThe radiation exposures of the patients were measured with the entrance skin radiation dose (cumulative air KERMA – Kinetic Energy Released per unit MAss).
The fluoroscopy times and dose area product were also measured to determine the radiation exposure time and the irradiated area, respectively.
The procedures were performed in the Allura Xper FD10 monoplane flat detector (Philips – Einthoven, Netherlands), with three magnetic fields (15cm, 20cm, and 25cm), double filter (copper+aluminium) and a standard image acquisition program at 15 frames per second.
Statistical analysisThree groups were compared. Group A comprised patients weighing≤79kg; group B, patients weighed 80–99kg; and group C, patients weighed≥100kg. Data were prospectively collected and stored in a dedicated database within the ACCESS program. The Statistical Package for Social Sciences (SPSS) version 18.0 for Windows was used for the analyses. The results were shown as mean, standard deviation, median, and interquartile interval. The chi-squared tests, the Kruskal-Wallis test, and the Bonferroni post-hoc test of ANOVA were used for the group comparisons. A multiple logistic regression model was applied to identify the possible predictors of increased radiation exposure (total dose≥2Gy). In this analysis, statistically significant variables were used in the univariate analysis. A two-tailed P-value of < 0.05 was considered statistically significant.
RESULTSBetween August of 2010 and December of 2011, 671 invasive cardiac procedures were performed: 363 in group A, 252 in group B, and 56 in group C.
The total number of procedures corresponded to 420 diagnostic catheterisations and 251 coronary angioplasties. There was no significant difference between the groups regarding the proportion of diagnostic cardiac catheterisations (61.2%, 63.5%, and 67.9% in groups A, B, and C, respectively) and coronary angioplasty (38.8%, 36.5%, and 32.1% in groups A, B, and C, respectively).
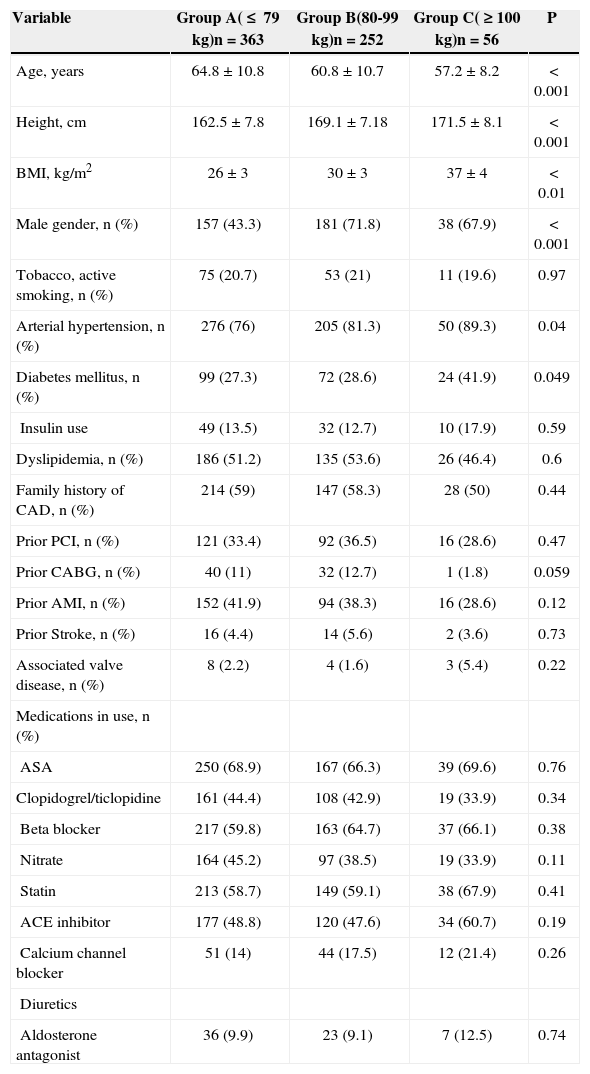
Demographic characteristicsIn general, it was observed that the patients in group C presented significantly greater prevalences of systemic arterial hypertension and diabetes mellitus. Regarding the other risk factors for cardiovascular disease and the prescribed patient medications, there was no significant difference between the groups. Table 1 details the clinical characteristics of the three groups.
Patient Clinical Characteristics
| Variable | Group A(≤ 79kg)n=363 | Group B(80-99kg)n=252 | Group C(≥100kg)n=56 | P |
|---|---|---|---|---|
| Age, years | 64.8±10.8 | 60.8±10.7 | 57.2±8.2 | < 0.001 |
| Height, cm | 162.5±7.8 | 169.1±7.18 | 171.5±8.1 | < 0.001 |
| BMI, kg/m2 | 26±3 | 30±3 | 37±4 | < 0.01 |
| Male gender, n (%) | 157 (43.3) | 181 (71.8) | 38 (67.9) | < 0.001 |
| Tobacco, active smoking, n (%) | 75 (20.7) | 53 (21) | 11 (19.6) | 0.97 |
| Arterial hypertension, n (%) | 276 (76) | 205 (81.3) | 50 (89.3) | 0.04 |
| Diabetes mellitus, n (%) | 99 (27.3) | 72 (28.6) | 24 (41.9) | 0.049 |
| Insulin use | 49 (13.5) | 32 (12.7) | 10 (17.9) | 0.59 |
| Dyslipidemia, n (%) | 186 (51.2) | 135 (53.6) | 26 (46.4) | 0.6 |
| Family history of CAD, n (%) | 214 (59) | 147 (58.3) | 28 (50) | 0.44 |
| Prior PCI, n (%) | 121 (33.4) | 92 (36.5) | 16 (28.6) | 0.47 |
| Prior CABG, n (%) | 40 (11) | 32 (12.7) | 1 (1.8) | 0.059 |
| Prior AMI, n (%) | 152 (41.9) | 94 (38.3) | 16 (28.6) | 0.12 |
| Prior Stroke, n (%) | 16 (4.4) | 14 (5.6) | 2 (3.6) | 0.73 |
| Associated valve disease, n (%) | 8 (2.2) | 4 (1.6) | 3 (5.4) | 0.22 |
| Medications in use, n (%) | ||||
| ASA | 250 (68.9) | 167 (66.3) | 39 (69.6) | 0.76 |
| Clopidogrel/ticlopidine | 161 (44.4) | 108 (42.9) | 19 (33.9) | 0.34 |
| Beta blocker | 217 (59.8) | 163 (64.7) | 37 (66.1) | 0.38 |
| Nitrate | 164 (45.2) | 97 (38.5) | 19 (33.9) | 0.11 |
| Statin | 213 (58.7) | 149 (59.1) | 38 (67.9) | 0.41 |
| ACE inhibitor | 177 (48.8) | 120 (47.6) | 34 (60.7) | 0.19 |
| Calcium channel blocker | 51 (14) | 44 (17.5) | 12 (21.4) | 0.26 |
| Diuretics | ||||
| Aldosterone antagonist | 36 (9.9) | 23 (9.1) | 7 (12.5) | 0.74 |
ASA=acetylsalicylic acid, CAD=coronary arterial disease, ACE=angiotensin-converting enzyme, AMI=acute myocardial infarction, PCI=percutaneous coronary intervention, BMI=body mass index, CABG=coronary artery bypass graft.
The majority of the diagnostic procedures were performed through femoral access (78.8%, 69.8%, and 44% in groups A, B, and C, respectively, P=0.16). The severity of the coronary artery disease was similar in groups A, B, and C: one vessel (78%, 74.6%, and 85.7%; P=0.16), two vessels (14%, 17.5%, and 10.7%; P=0.85), and three or more vessels (8%, 7.9%, and 3.6%; P=0.9). In all groups, the left anterior descending artery was most affected (group A, 39.7%; group B, 37.3%; and group C, 30.4%; P=0.76), while the left main coronary artery presented significant lesions in 1.1%, 2.8% and 3.6% of the patients in groups A, B, and C, respectively (P=0.21).
In coronary angioplasties, the preferred access site was the femoral artery (80%, 77.4%, and 55% in groups A, B, and C, respectively, P=0.67). The success rates (group A, 95%; group B, 93.1%; and group C, 92.9%; P=0.76), type B2/C lesions (group A, 65%; group B, 71%; and group C, 73.1%; P=0.68), diameter (group A, 3.04mm; group B, 3.16mm; and group C, 3.2mm; P=0.45), and stent length (group A, 17.88mm; group B, 18.56mm; and group C, 16.57mm; P=0.34) were similar among the groups. The presence of chronic occlusion and bifurcation lesion was not different among the groups.
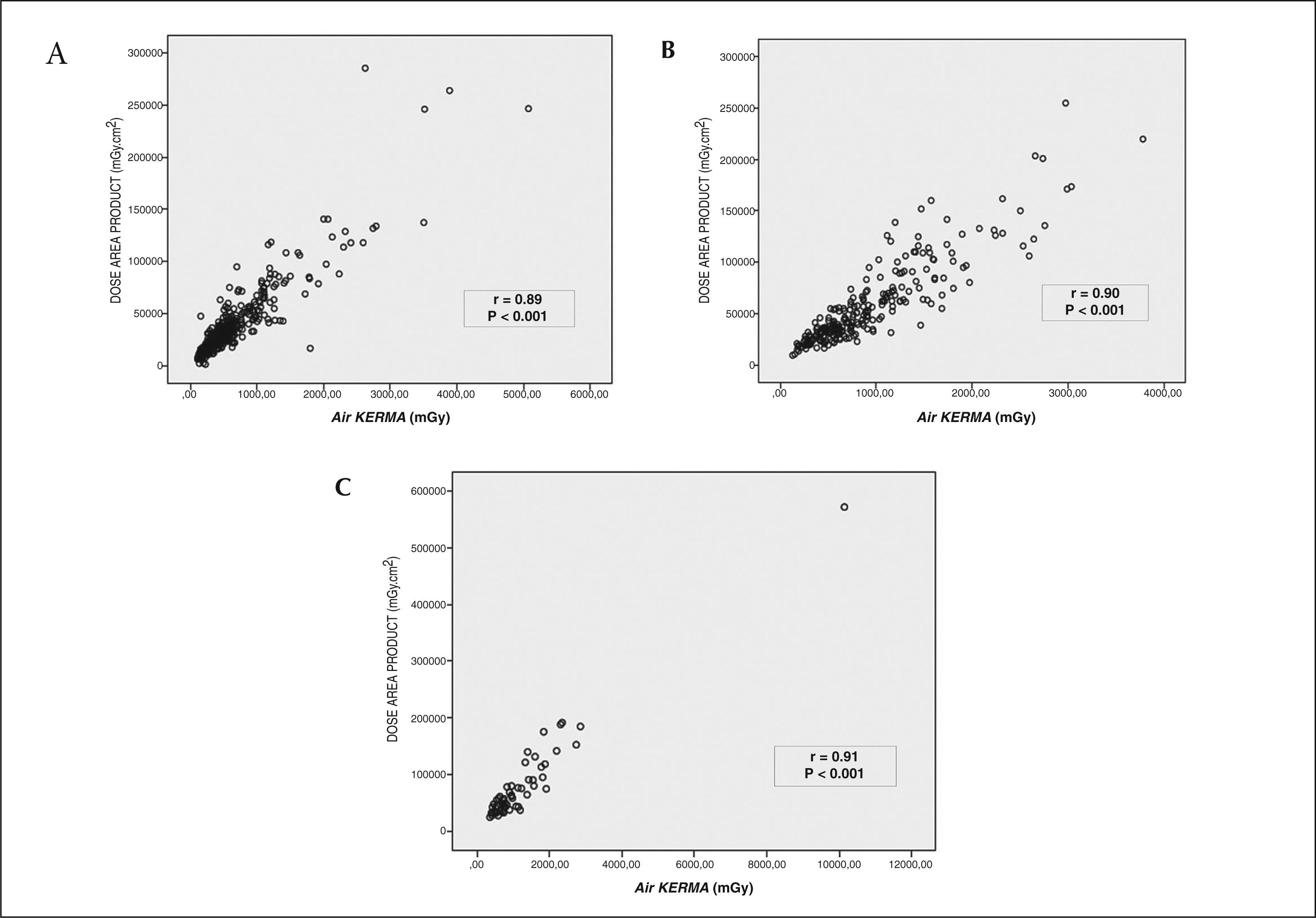
Parameters of radiology exposureIt was observed that patients with higher weight were significantly more exposed to ionising radiation. Both the entrance skin radiation (air KERMA) and the dose area product were progressively increased in the heavier patients. Table 2 presents the values for radiation exposure in each group. The correlation between the total dose received and the irradiated area was significant in the three groups studied, as shown by Figure 1.
Radiology Exposure Parameters among the Groups
| Variable | Group A(≤79kg)n=363 | Group B(80–99kg)n=252 | Group C(≥100kg)n=56 | P |
|---|---|---|---|---|
| Fluoroscopy time, minutes | 4.35 | 4.53 | 4.41 | 0.60 |
| Number of graphs per exam | 11 | 11 | 11 | >0.9 |
| Total number of frames | 779 | 811 | 739 | 0.45 |
| Total number of frames/graphs | 67.5 | 69.5 | 69.25 | 0.83 |
| Radiation exposure | ||||
| Air KERMA for patients, mGy | < 0.001 | |||
| - Inferior quartile (Q1/4) | 276.2 | 476.94 | 606.34 | |
| - Median (Q2/4) | 484.29 | 735.69 | 900.36 | |
| - Superior quartile (Q3/4) | 766.19 | 1,191.93 | 1,517.48 | |
| Dose area product, mGycm2 | < 0.001 | |||
| - Inferior quartile (Q1/4) | 17,239 | 30,401 | 38,782 | |
| - Median (Q2/4) | 29,327 | 43,319 | 57,987 | |
| - Superior quartile (Q3/4) | 46,210 | 71,287 | 90,856 |
In the present sample, radiation exposure > 2Gy occurred in 3.6% (13/363) of the procedures in group A, in 16.3% (41/252) of the group B procedures, and in 10.7% (6/56) of the group C procedures. Using the uni- and multivariate analyses, patient’s weight, elective angioplasty and ad hoc angioplasty were determined to be predictors of increased radiation exposure. Table 3 presents the odds ratio and its confidence interval.
DISCUSSIONThe present study is the first in this institution to examine the impact of body weight on the radiation exposure of patients undergoing invasive cardiac procedures. The results demonstrated that obese patients were more exposed to radiation than non-obese individuals.
Currently available equipment for haemodynamic monitoring has an automatic dose and image quality control (Automatic Bright Control – ABC).3,9,10 Although the operation system is complex, in practice, every time the equipment detects low-resolution image or great brightness variation, the dose is increased to compensate. In overweight patients, the thickness and density of the chest are increased; therefore, the equipment automatically releases a higher dose to maintain quality standards. Studies using an ionisation chamber have shown that for every 1-cm of thickness, radiation exposure increased by 25%.3 For this reason, obese patients receive higher dose of radiation during the procedures.
Obesity has been proven to interfere in some cardiovascular outcomes, such as vascular complications 7,11 and the incidence of atrial fibrillation.12 Data from electrophysiological studies have shown that obese patients, when undergoing pulmonary vein ablation, received a dose that was two times higher than non-obese patients.13 The present results show that the patients weighing over 100kg received 1.8 and 1.2 times more radiation than the patients weighing up to 79kg and up to 99kg, respectively. Therefore, obesity has a significant impact on radiation exposure.
Concerns related to ionising radiation are completely reasonable and pertinent to all individuals who are exposed to this type of biological effect. Radiation reduction methods are outdated, and new proposals have been presented.14–18 It has been stipulated that ionising radiation exposure should be as low as possible when it is inevitable. The “as low as reasonably achievable” (ALARA) principle,19,20 established in 1977, essentially states that radiation exposure should be kept as low as reasonably achievable. Although the ALARA principle is widely known, Mavrikou et al.21 called attention to the fact that many radiation and protection concepts are neglected by interventional physicians. Critical exposure doses (2Gy) are frequently surpassed in the procedures; therefore, the principle is not being respected.8
Radiation over-exposure is becoming more frequent in daily practice. This group has demonstrated that flat detector equipment can add 65% more radiation compared to image intensifier devices,22 and has also demonstrated that up to 12% of the invasive cardiac procedures surpassed the critical dose of 2Gy.8 Nowadays, skin lesions, which were previously rare, have been reported during interventional cardiology procedures.5 More recently, six alarming cases of brain tumors6 in interventional cardiology patients have again raised concerns about occupational risks. Therefore, medical societies are encouraging more training programs and education measures to reduce the biological risks.1,16,17
The area exposed to biological radiation effects and the potential stochastic risks of neoplasia are as important as the total radiation dose. The present study demonstrated that there is a strong relation between the total received dose and the irradiated area, regardless of the patient’s weight. Patients weighing over 100kg received approximately 57,987mGy.cm2 during the procedures. This measure is higher than the 50,000 mGycm 2 dose recommended by the International Atomic Energy Agency (IAEA).23 In obese patients, the irradiated area is greater than the recommended dose. This finding is important because larger irradiated areas have increased risks for stochastic effects and neoplasia.
Although it has not been demonstrated in the present study, other authors have determined that the risk of radiation exposure was attributable to cancer incidence. Using the Biological Effects of Ionising Radiation (BEIR VII)24,25 risk model, it can be concluded that risk of developing a solid tumour after radiation exposure is low. Nevertheless, continuing exposure and higher doses can promote a higher risk that may still be unknown.26,27
Limitations of the studyThe present study had several limitations that must be considered. This analysis was conducted in only one centre with a small patient sample. Radiation exposure is only related to the radiation dose received by the patient; therefore, any inference regarding the dose received by the haemodynamicists could not be determined.
CONCLUSIONSBody weight has a significant impact on radiation exposure in invasive cardiac procedures. Overweight patients are significantly more exposed to higher doses of ionising radiation.
ACKNOWLEDGMENTSThe authors would like to thank the haemodynamicists Drs. Alexandre Damiani Azmus, André Manica, Carlos Roberto Cardoso, Henrique Basso Gomes, Flávio Celso Leboute, Luis Maria Yordi, Mauro Régis Moura, and Rogério Sarmento-Leite for collaborating in this study.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.