Percutaneous coronary interventions (PCIs) in complex lesions are increasingly common in daily practice. The objective of this study was to determine the impact of complex lesions on radiological exposure during PCI.
MethodsProspective cohort study including patients undergoing PCI between August 2010 and December 2011. Clinical, angiographic and radiation exposure characteristics were recorded in a dedicated database. Patterns of radiation exposure (total dose received, fluoroscopy time and dose-area product) were determined in patients undergoing PCI for noncomplex (A/B1) and complex (B2/C) lesions. Data were analyzed by the SPSS 18.0 program. Independent radiation exposure predictors were determined by multiple logistic regression.
ResultsWe analyzed 413 PCIs, 83 lesions in group A/B1 and 330 in group B2/C. There were no clinically significant differences between groups. The median radiation dose received by patients was significantly higher in group B2/C (1,103.9mGy vs 866.6mGy; P < 0.01). The dose-area product (43,484mGy.cm2 vs 58,327mGy.cm2; P < 0.001) and fluoroscopy time (9±6 minutes vs 12.1±9.5minutes; P=0.001) were also significantly higher in group B2/C. Predictors of increased radiation exposure were weight [odds ratio (OR) 1.02 for each increase of 1kg, confidence interval (CI) 1.01-1.036; P=0.004], type B2/C lesion (OR 1.9, CI 1.002-4.96; P=0.002).
ConclusionsPatients undergoing PCI in complex lesions are significantly more exposed to radiation. Weight and lesion type (B2/C) are predictors of increased radiation exposure.
Impacto das Lesões Complexas na Exposição RadiológicaDurante Intervenção Coronária Percutânea
IntroduçãoIntervenções coronárias percutâneas (ICPs) em lesões complexas são cada vez mais comuns na prática diária. O objetivo deste estudo foi determinar o impacto das lesões complexas na exposição radiológica durante ICP.
MétodosEstudo de coorte prospectiva incluindo pacientes submetidos a ICP entre agosto de 2010 e dezembro de 2011. Características clínicas, angiográficas e de exposição à radiação foram registradas em banco de dados específico. Os padrões de exposição à radiação (dose total recebida, tempo de fluoroscopia e produto dose-área) foram determinados em pacientes submetidos a ICP de lesões não-complexas (A/B1) e complexas (B2/C). Os dados foram analisados em programa SPSS 18.0. Preditores independentes de exposição à radiação foram determinados por regressão logística múltipla.
ResultadosForam analisadas 413 ICPs, sendo 83 lesões no grupo A/B1 e 330 no grupo B2/C. Não ocorreram diferenças clínicas significativas entre os grupos. A mediana de radiação recebida pelos pacientes foi significativamente maior no grupo B2/C (1.103,9mGy vs. 866,6mGy; P < 0,01). O produto doseárea (43.484mGy.cm2 vs. 58.327mGy.cm2; P < 0,001) e o tempo de fluoroscopia (9±6 minutos vs. 12,1±9,5 minutos; P=0,001) também foram significativamente maiores no grupo B2/C. Os preditores de exposição radiológica aumentada foram peso [razão de chance (RC) 1,02 para cada aumento de 1kg, intervalo de confiança (IC) 1,01-1,036; P=0,004] e lesão tipo B2/C (RC 1,9, IC 1,002-4,96; P=0,002).
ConclusõesPacientes submetidos a ICP em lesões complexas são significativamente mais expostos à radiação. Peso e tipo de lesão (B2/C) são preditores de exposição radiológica aumentada.
Fluoroscopy-guided interventional procedures are performed in large numbers around the world, with increasing frequency over the past 20 years.1 In addition to the progressive increase in the number of interventions, procedure complexity has also increased.2,3
Interventions in complex lesions4 involve greater technical difficulty, which results in higher costs, contrast volume, procedure time, and radiation exposure.5-7 Recent studies have demonstrated that many percutaneous coronary interventions (PCIs) exceed the dose of 2Gy, the threshold for development of skin lesions. However, the literature has no specific studies focusing on lesion complexity.
Therefore, the objective of this study was to determine the impact of complex lesions on radiological exposure during PCI.
METHODSDesignThis was a prospective cohort study including patients undergoing PCI between August 2010 and December 2011.
SampleAfter signing the informed consent form approved by the local ethics and research committee, patients requiring PCI had their procedures monitored in order to record the patterns of radiological exposure. Technical details of the PCIs were prospectively recorded and entered into a specific database.
Analysed characteristicsData on age, gender, risk factors for cardiovascular disease, clinical presentation and procedure indications, ventricular function, number of affected vessels, treated vessels, characteristics of lesions, and success rate were collected and analyzed. Specific data on radiological exposure (dose received, dose-area product, and fluoroscopy time) were also collected.
Radiological exposure parametersThe radiological exposure of patients was measured by the amount of incoming radiation on the skin (cumulative air KERMA [Kinetic Energy Released per unit MAss]). The fluoroscopy time and dose-area product were also measured to determine the time of radiological exposure and the irradiated area, respectively.
The procedures were performed in equipment with Philips Allura Xper FD10 monoplane detectors (Philips=Einthoven, Netherlands) with three magnification fields (15cm, 20cm, and 25cm), double filter (copper and aluminium), and standard programming with image acquisition rate of 15 frames/second.
Statistical AnalysisThe patients were divided into two groups for comparison, according to the classification of the type of lesion proposed by the American College of Cardiology/American Heart Association (ACC/AHA):8 patients undergoing PCI of noncomplex (type A/B1) and complex lesions (type B2/C). Data were prospectively collected and stored in a database using ACCESS software. For analysis, SPSS for Windows version 18.0 was used. The chi-squared test, Student’s t-test, and the Mann–Whitney test were used for comparison. Independent predictors of increased radiation exposure (dose < 2Gy) were determined by multiple logistic regression. Two-tailed p-value < 0.05 was considered statistically significant.
RESULTSDuring the study period, 413 PCIs were analyzed: 83 in the group of A/B1 lesions and 330 in the group of B2/C lesions.
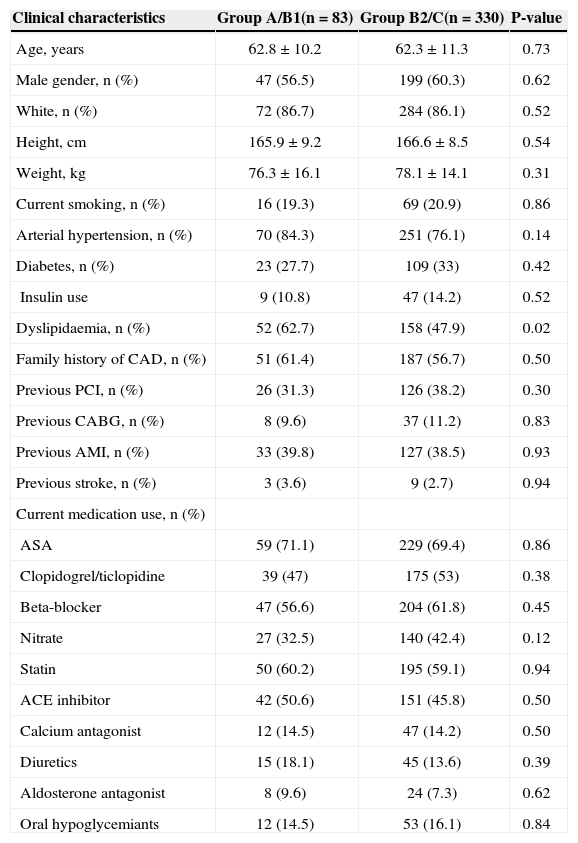
Patients in both groups had similar clinical profiles, except for the higher prevalence of dyslipidaemia in the group A/B1. Regarding medications, the clinical treatment was similar between groups (Table 1).
Clinical characteristics and administered drug treatment
| Clinical characteristics | Group A/B1(n=83) | Group B2/C(n=330) | P-value |
|---|---|---|---|
| Age, years | 62.8±10.2 | 62.3±11.3 | 0.73 |
| Male gender, n (%) | 47 (56.5) | 199 (60.3) | 0.62 |
| White, n (%) | 72 (86.7) | 284 (86.1) | 0.52 |
| Height, cm | 165.9±9.2 | 166.6±8.5 | 0.54 |
| Weight, kg | 76.3±16.1 | 78.1±14.1 | 0.31 |
| Current smoking, n (%) | 16 (19.3) | 69 (20.9) | 0.86 |
| Arterial hypertension, n (%) | 70 (84.3) | 251 (76.1) | 0.14 |
| Diabetes, n (%) | 23 (27.7) | 109 (33) | 0.42 |
| Insulin use | 9 (10.8) | 47 (14.2) | 0.52 |
| Dyslipidaemia, n (%) | 52 (62.7) | 158 (47.9) | 0.02 |
| Family history of CAD, n (%) | 51 (61.4) | 187 (56.7) | 0.50 |
| Previous PCI, n (%) | 26 (31.3) | 126 (38.2) | 0.30 |
| Previous CABG, n (%) | 8 (9.6) | 37 (11.2) | 0.83 |
| Previous AMI, n (%) | 33 (39.8) | 127 (38.5) | 0.93 |
| Previous stroke, n (%) | 3 (3.6) | 9 (2.7) | 0.94 |
| Current medication use, n (%) | |||
| ASA | 59 (71.1) | 229 (69.4) | 0.86 |
| Clopidogrel/ticlopidine | 39 (47) | 175 (53) | 0.38 |
| Beta-blocker | 47 (56.6) | 204 (61.8) | 0.45 |
| Nitrate | 27 (32.5) | 140 (42.4) | 0.12 |
| Statin | 50 (60.2) | 195 (59.1) | 0.94 |
| ACE inhibitor | 42 (50.6) | 151 (45.8) | 0.50 |
| Calcium antagonist | 12 (14.5) | 47 (14.2) | 0.50 |
| Diuretics | 15 (18.1) | 45 (13.6) | 0.39 |
| Aldosterone antagonist | 8 (9.6) | 24 (7.3) | 0.62 |
| Oral hypoglycemiants | 12 (14.5) | 53 (16.1) | 0.84 |
CAD, coronary artery disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; AMI, acute myocardial infarction; ASA, acetyl salicylic acid; ACE, Angiotensin-converting enzyme.
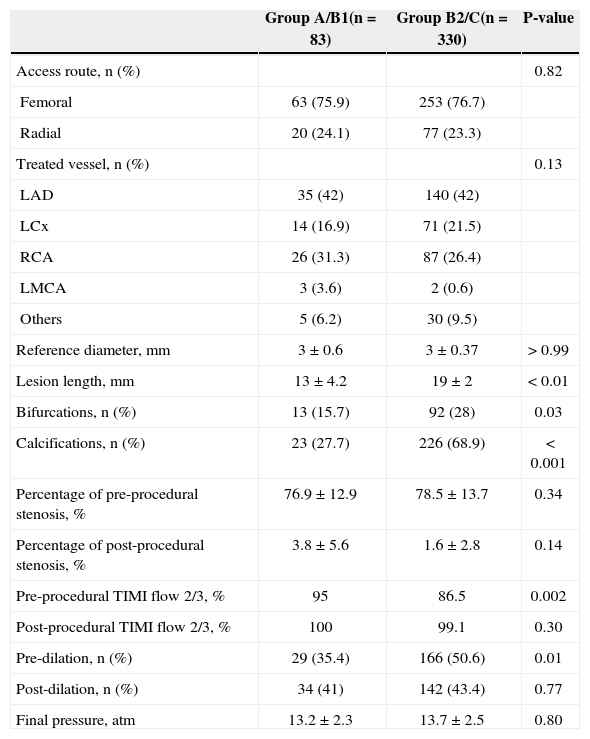
It can be observed that the patients in group B2/C had higher angiographic complexity (Table 2). The percentage of stenosis pre- (76.9±12.9% vs. 78.5±13.7%; P=0.34) and post-procedure (3.8±5.6% vs. 1.6±12.8%; P=0.14) was similar between groups. Pre-procedure Thrombosis in Myocardial Infarction (TIMI) 2/3 coronary flow was more frequent in the A/B1 group (95% vs. 86.5%; P=0.002), but it became similar in both groups after the PCI (100% vs. 99.1%; P=0.30).
Angiographic and procedural characteristics
| Group A/B1(n=83) | Group B2/C(n=330) | P-value | |
|---|---|---|---|
| Access route, n (%) | 0.82 | ||
| Femoral | 63 (75.9) | 253 (76.7) | |
| Radial | 20 (24.1) | 77 (23.3) | |
| Treated vessel, n (%) | 0.13 | ||
| LAD | 35 (42) | 140 (42) | |
| LCx | 14 (16.9) | 71 (21.5) | |
| RCA | 26 (31.3) | 87 (26.4) | |
| LMCA | 3 (3.6) | 2 (0.6) | |
| Others | 5 (6.2) | 30 (9.5) | |
| Reference diameter, mm | 3±0.6 | 3±0.37 | > 0.99 |
| Lesion length, mm | 13±4.2 | 19±2 | < 0.01 |
| Bifurcations, n (%) | 13 (15.7) | 92 (28) | 0.03 |
| Calcifications, n (%) | 23 (27.7) | 226 (68.9) | < 0.001 |
| Percentage of pre-procedural stenosis, % | 76.9±12.9 | 78.5±13.7 | 0.34 |
| Percentage of post-procedural stenosis, % | 3.8±5.6 | 1.6±2.8 | 0.14 |
| Pre-procedural TIMI flow 2/3, % | 95 | 86.5 | 0.002 |
| Post-procedural TIMI flow 2/3, % | 100 | 99.1 | 0.30 |
| Pre-dilation, n (%) | 29 (35.4) | 166 (50.6) | 0.01 |
| Post-dilation, n (%) | 34 (41) | 142 (43.4) | 0.77 |
| Final pressure, atm | 13.2±2.3 | 13.7±2.5 | 0.80 |
LAD, left anterior descending artery; LCx, left circumflex artery; RCA, right coronary artery; LMCA, left main coronary artery; TIMI, Thrombolysis in Myocardial Infarction.
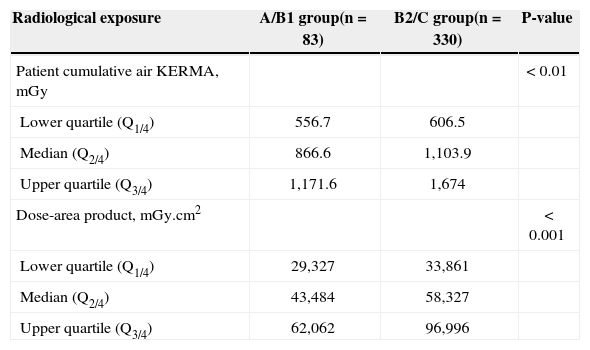
The median radiation dose received by patients was significantly higher in group B2/C (Table 3). The fluoroscopy times (9±6 minutes vs. 12.1±9.5minutes; P=0.001), the number of radiographies (17.8±7.1 vs. 21.2±9.3; P=0.002), and the total number of frames (986±423 vs. 1,166±540; P=0.005) were also higher in the B2/C group.
Radiological exposure parameters
| Radiological exposure | A/B1 group(n=83) | B2/C group(n=330) | P-value |
|---|---|---|---|
| Patient cumulative air KERMA, mGy | < 0.01 | ||
| Lower quartile (Q1/4) | 556.7 | 606.5 | |
| Median (Q2/4) | 866.6 | 1,103.9 | |
| Upper quartile (Q3/4) | 1,171.6 | 1,674 | |
| Dose-area product, mGy.cm2 | < 0.001 | ||
| Lower quartile (Q1/4) | 29,327 | 33,861 | |
| Median (Q2/4) | 43,484 | 58,327 | |
| Upper quartile (Q3/4) | 62,062 | 96,996 |
KERMA, kinetic energy released per unit mass.
In four (4.8%) PCIs in A/B1 the group and in 48 (14.5%) in the B2/C group (P < 0.01) the 2Gy dose was exceeded.
The following predictors of increased radiation exposure were determined by multiple logistic regression: weight (odds ratio [OR], 1.02 per 1kg increase; confidence interval [CI] of 1.01 to 1.036; P=0.004), and lesion type B2/C (OR 1.9; CI 1.002 to 4.96; P=0.002).
DISCUSSIONThe present study determined that the radiological exposure is higher in patients submitted to PCI in complex lesions. The harmful effects of radiation, mainly dosedependent (deterministic), have been widely reported in procedures involving ionising radiation.9-12 However, physicians’ knowledge about the harmful effects of radiation is not proportional to their exposure.13
Along with the growing number of more complex procedures, hemodynamics equipment has also developed. The more modern flat panel technology is very attractive because it allows for higher quality and better image resolution.14 However, clinical studies have demonstrated that the incorporation of this technology causes higher radiation exposure.15,16 For this reason, scientific societies have published recommendations and guidelines aiming to reduce radiation levels during procedures.1,17
Since the publication of the SYNergy between Percutaneous Coronary Intervention and Cardiac Surgery Study (SYNTAX),18 which demonstrated that patients with low angiographic and anatomical complexity (score < 22) have a favourable clinical outcome when submitted to PCI with drug-eluting stents, interventions in multiple vessels have become common in hemodynamics laboratories. However, little has been discussed about radiological exposure. Although this study does not refer to the type of intervention (single or multivessel), the simple fact that PCI was performed in complex lesions promoted a 27% increase in radiation exposure for the patient. This fact is relevant, as increasingly more cases of radiation-related lesions have been reported in patients and health professionals.12 In practice, health professionals can minimize occupational radiation by using individual lead protection clothing associated with physical shields. However, patients do not have this protection.
According to the International Atomic Energy Agency (IAEA), the radiation exposure during cardiac diagnostic and therapeutic procedures should not exceed 2Gy. However, that dose was exceeded in 14% of patients undergoing complex interventions in the present study. This fact is relevant, as most PCIs were performed in type B2/C lesions, as in the real world.4 Considering that many patients were obese,19 a known predictor of increased exposure, overexposure can be even greater. It is therefore essential that professionals take that into consideration and minimize radiation exposure during radiological assessment.
Study limitationsThe main limitation of the present study is the small number of patients included. Moreover, the dose received by the interventional physician could not be measured.
CONCLUSIONSPatients submitted to PCI in complex lesions are significantly more exposed to radiation. Weight and complex lesions (B2/C type) are predictors of increased radiation exposure.
CONFLICT OF INTERESTThe authors declare no conflicts of interests.