Drug-eluting stents (DES) have changed contemporary interventional cardiology practice, enabling the approach of increasingly more complex clinical and angiographic scenarios. The objective of this study was to demonstrate the changes observed in the last 10 years in the indication and practice of percutaneous coronary intervention (PCI) at a tertiary private hospital in the State of São Paulo.
MethodsDESIRE is a single-center prospective registry aiming at following the acute and late outcomes of consecutive patients treated by DES.
ResultsFrom 2002 to 2011, 4,299 patients were included, with mean age of 64.3±11.2years, 23% were female and 30.5 were diabetic. The total number of lesions treated was 6,518 of which 61.5% were type B2/C. During the course of the study, DES were progressively more used, reaching a penetration of 88.4% in 2011. The complexity of PCIs has increased and in the past year 1.76 lesions per patient were treated with an average of 1.89 DES. The SYNTAX score increased from 12.3±4.4 (2002-2006) to 15.7±4.7 (2007-2011). Clinical follow-up was obtained in 98.2% of the patients, with a median of 5.2years, and during this period target-lesion revascularization rate was 5%, myocardial infarction was 6.7% and cardiovascular death was 4.1%. Stent thrombosis was observed in 2.4% of the cases.
ConclusionsOur results showed a marked increment in the complexity profile of patients treated in the last 10 years and at the same time confirm the long-term effectiveness of DES, despite the clinical and angiographic profile of patients.
Impacto do Uso Rotineiro deStents Farmacológicos na Pràtica Intervencionista Contemporànea de um Centro Terciàrio: Experiencia de uma Década do Registro DESIRE
IntroduçãoOs stents farmacológicos (SFs) modificaram a prática intervencionista contemporânea, permitindo abordar cenários clínicos e angiográficos progressivamente mais complexos. O objetivo deste estudo foi demonstrar as modificações ocorridas nos últimos 10 anos na forma de indicar e de realizar a intervenção coronária percutânea (ICP) em um hospital privado, terciário, do Estado de São Paulo.
MétodosO DESIRE é um registro unicêntrico, prospectivo, com o objetivo de acompanhar os desfechos agudos e tardios de pacientes consecutivos tratados com SFs.
ResultadosNo período de 2002 a 2011, foram incluídos 4.229 pacientes, com média de idade de 64,3±11,2 anos; 23% eram do sexo feminino, e 30,5%, diabéticos. Foram tratadas 6.518 lesões, das quais 61,5% eram do tipo B2/C. Os SFs foram utilizados em proporção crescente, alcançando penetração de 88,4% em 2011. A complexidade das ICPs aumentou, sendo tratada no último ano 1,76 lesão por paciente, com média de 1,89 SF. O escore SYNTAX, no período de 2002–2006, foi de 12,3±4,4, enquanto entre 2007–2011 elevou-se para 15,7±4,7. O seguimento clínico foi obtido em 98,2% dos pacientes, com mediana de 5,2 anos, sendo observada, nesse período, revascularização da lesão-alvo em 5%, infarto do miocárdio em 6,7% e óbito cardiovascular em 4,1% dos pacientes. A trombose do stent ocorreu em 2,4% dos casos.
ConclusõesNossos resultados demonstram marcante incremento no perfil de complexidade dos pacientes tratados nos últimos 10 anos e, ao mesmo tempo, confirmam a efetividade a longo prazo dos SFs, a despeito dos perfis clínico e angiográfico tratados.
The advent of drug-eluting stents (DES) modified contemporary interventional practice, allowing a routine and effective approach in traditionally unfavorable clinical and angiographic scenarios through percutaneous coronary intervention (PCI), for instance, lesions in the left main coronary artery.1
However, the relatively high cost of this new technology, particularly when compared to the cost of bare-metal stents (BMS), the previous primary intervention, made their incorporation into the routines of most private hospitals in Brazil a slow process, despite the striking benefits of DES, especially in reducing the need for new interventions in the target vessel.2–4 To date, this technology, which has now celebrated ten years of approval for clinical use in Brazil, has not yet been authorized by the public health system.
The present study aimed to demonstrate the modifications that have occurred over the past ten years regarding the indication and performance of myocardial revascularization procedures in patients with coronary artery disease in a private tertiary hospital in the state of São Paulo.
METHODSBeginning in May 2002, when the first DES was approved in Brazil, Drug-Eluting Stents in the Real World (DESIRE), a single-center prospective registry, was started at Hospital do Coração da Associaçao do Sanatòrio Sírio (HCor, São Paulo, SP, Brazil) in order to monitor acute outcomes (particularly late outcomes) in consecutive patients who were treated with DES. This registry has no exclusion criteria and evaluated all patients treated with at least one DES since 2002, thus representing a true picture of the interventional practice at this institution.
During this time, following the world trend, several changes occurred regarding the indications for PCI, which has become the most widespread and comprehensive treatment choice for coronary artery disease. The DESIRE registry has captured these changes and their impact on revascularization treatment outcomes throughout a ten-year period. For this purpose, a team was formed consisting of eight medical researchers, a statistician, a database manager, and two professionals dedicated to the follow-up of all patients included in the study, which was conducted through a standard questionnaire administered by telephone, e-mail, and mail.
The present study shows the impact of DES on the different types of revascularization (surgical vs. percutaneous), as well as the impact of new technology on the performance of percutaneous interventions, with data that reflects the complexity of these procedures, such as the number of treated lesions and the number of DES implanted per patient over the last decade.
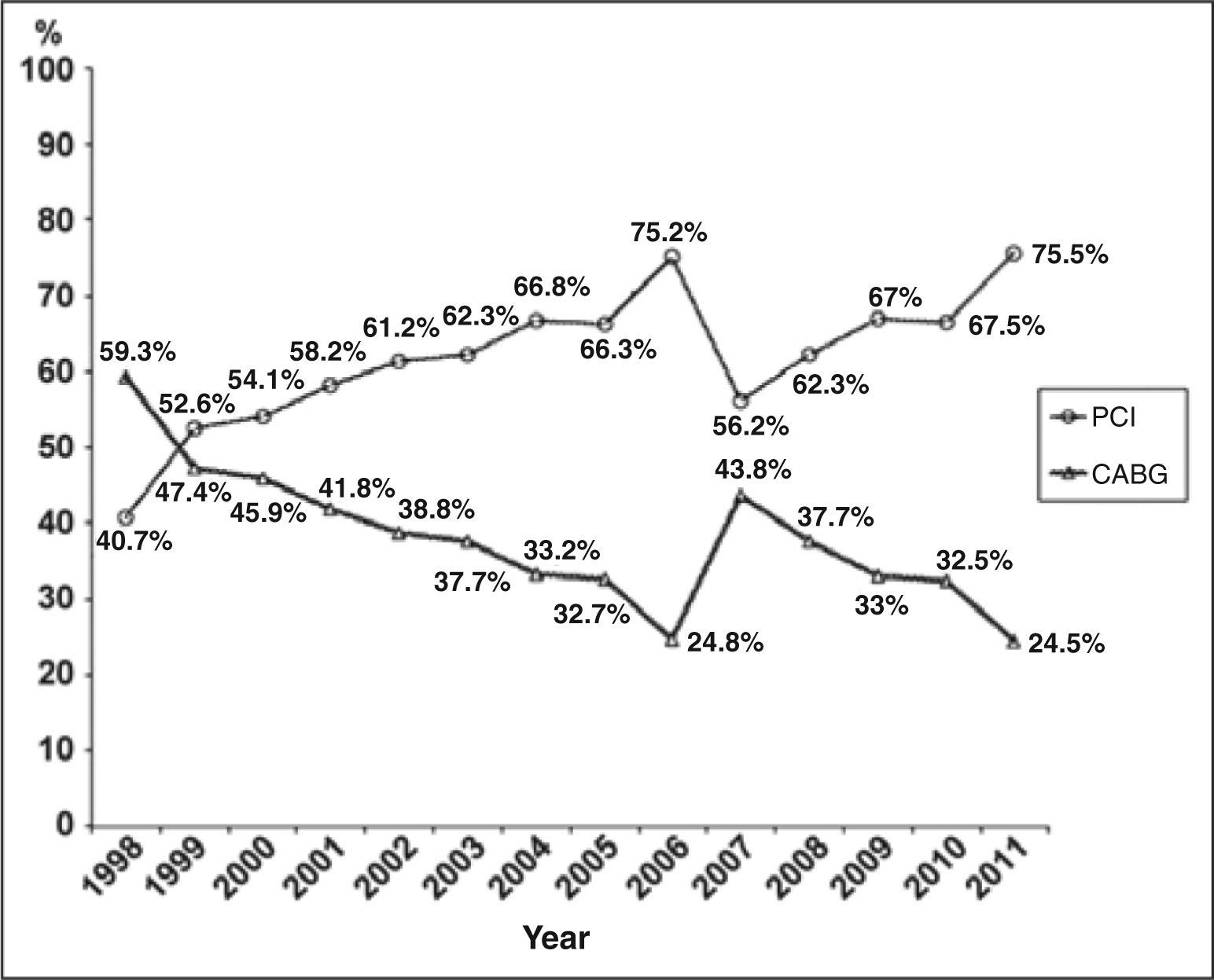
RESULTSSince 1999, PCI has become the predominantly used method of myocardial revascularization at this institution (Figure 1). Such predominance has become more pronounced since 2002, when DES were introduced, and particularly after 2008, when these devices became broadly reimbursed by most private health insurers in Brazil.
Types of revascularization procedures performed at Hospital do Coração da Associação do Sanatório Sírio for the past 13 years. Note that, since 1999, PCI has become the predominant revascularization method, a position that was consolidated with the 2002 introduction of DES. PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting.
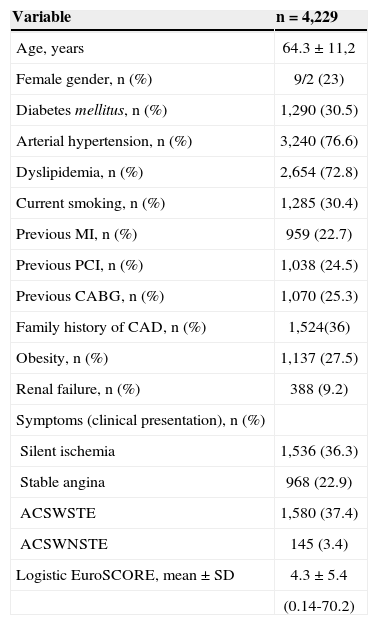
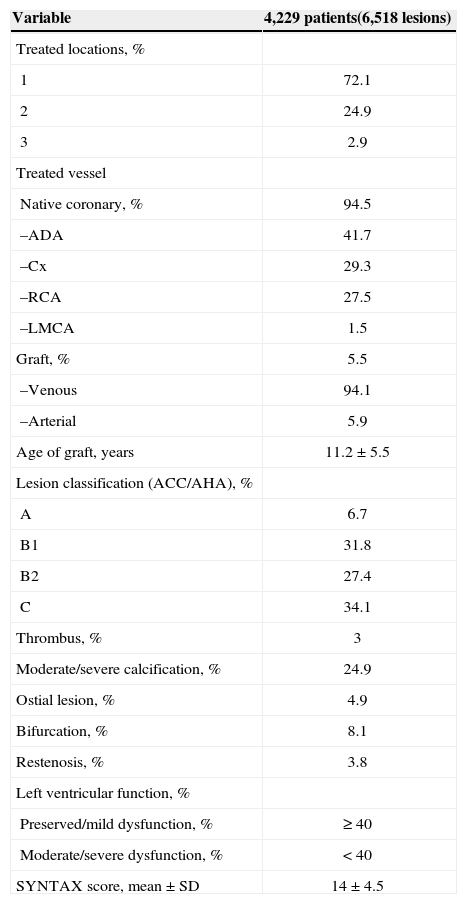
Since the formation of the DESIRE registry, 4,229 patients were treated exclusively with DES and included in the study. The clinical and angiographic characteristics of this population are shown in Tables 1 and 2. was 64.3±11.2years; 23% were females; 30.5% were diabetic, and approximately 25% of the patients had previously undergone a myocardial revascularization procedure (either percutaneous or surgical). Note the large number of individuals with previous renal dysfunction (9.2%) and acute coronary syndrome at the initial clinical presentation (40.8%).
Basal Clinical Characteristics
| Variable | n=4,229 |
|---|---|
| Age, years | 64.3±11,2 |
| Female gender, n (%) | 9/2 (23) |
| Diabetes mellitus, n (%) | 1,290 (30.5) |
| Arterial hypertension, n (%) | 3,240 (76.6) |
| Dyslipidemia, n (%) | 2,654 (72.8) |
| Current smoking, n (%) | 1,285 (30.4) |
| Previous MI, n (%) | 959 (22.7) |
| Previous PCI, n (%) | 1,038 (24.5) |
| Previous CABG, n (%) | 1,070 (25.3) |
| Family history of CAD, n (%) | 1,524(36) |
| Obesity, n (%) | 1,137 (27.5) |
| Renal failure, n (%) | 388 (9.2) |
| Symptoms (clinical presentation), n (%) | |
| Silent ischemia | 1,536 (36.3) |
| Stable angina | 968 (22.9) |
| ACSWSTE | 1,580 (37.4) |
| ACSWNSTE | 145 (3.4) |
| Logistic EuroSCORE, mean±SD | 4.3±5.4 |
| (0.14-70.2) |
MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; CAD, coronary artery disease; ACSWSTE, acute coronary syndrome with ST-segment elevation; ACSWNSTE, acute coronary syndrome with no ST-segment elevation.
Pre-procedural angiographic characteristics
| Variable | 4,229 patients(6,518 lesions) |
|---|---|
| Treated locations, % | |
| 1 | 72.1 |
| 2 | 24.9 |
| 3 | 2.9 |
| Treated vessel | |
| Native coronary, % | 94.5 |
| –ADA | 41.7 |
| –Cx | 29.3 |
| –RCA | 27.5 |
| –LMCA | 1.5 |
| Graft, % | 5.5 |
| –Venous | 94.1 |
| –Arterial | 5.9 |
| Age of graft, years | 11.2±5.5 |
| Lesion classification (ACC/AHA), % | |
| A | 6.7 |
| B1 | 31.8 |
| B2 | 27.4 |
| C | 34.1 |
| Thrombus, % | 3 |
| Moderate/severe calcification, % | 24.9 |
| Ostial lesion, % | 4.9 |
| Bifurcation, % | 8.1 |
| Restenosis, % | 3.8 |
| Left ventricular function, % | |
| Preserved/mild dysfunction, % | ≥ 40 |
| Moderate/severe dysfunction, % | < 40 |
| SYNTAX score, mean±SD | 14±4.5 |
ADA, anterior descending artery; Cx, circumflex artery; RCA, right coronary artery; LMCA, left main coronary artery; AHA/ACC, American Heart Association/American College of Cardiology.
From the angiographic viewpoint, a predominance of complex lesions was observed (61.5% of type B2/C lesions according to American Heart Association/American College of Cardiology classifications), with 5.5% of the target lesions localized in bypass grafts and 4.9% in ostial locations.
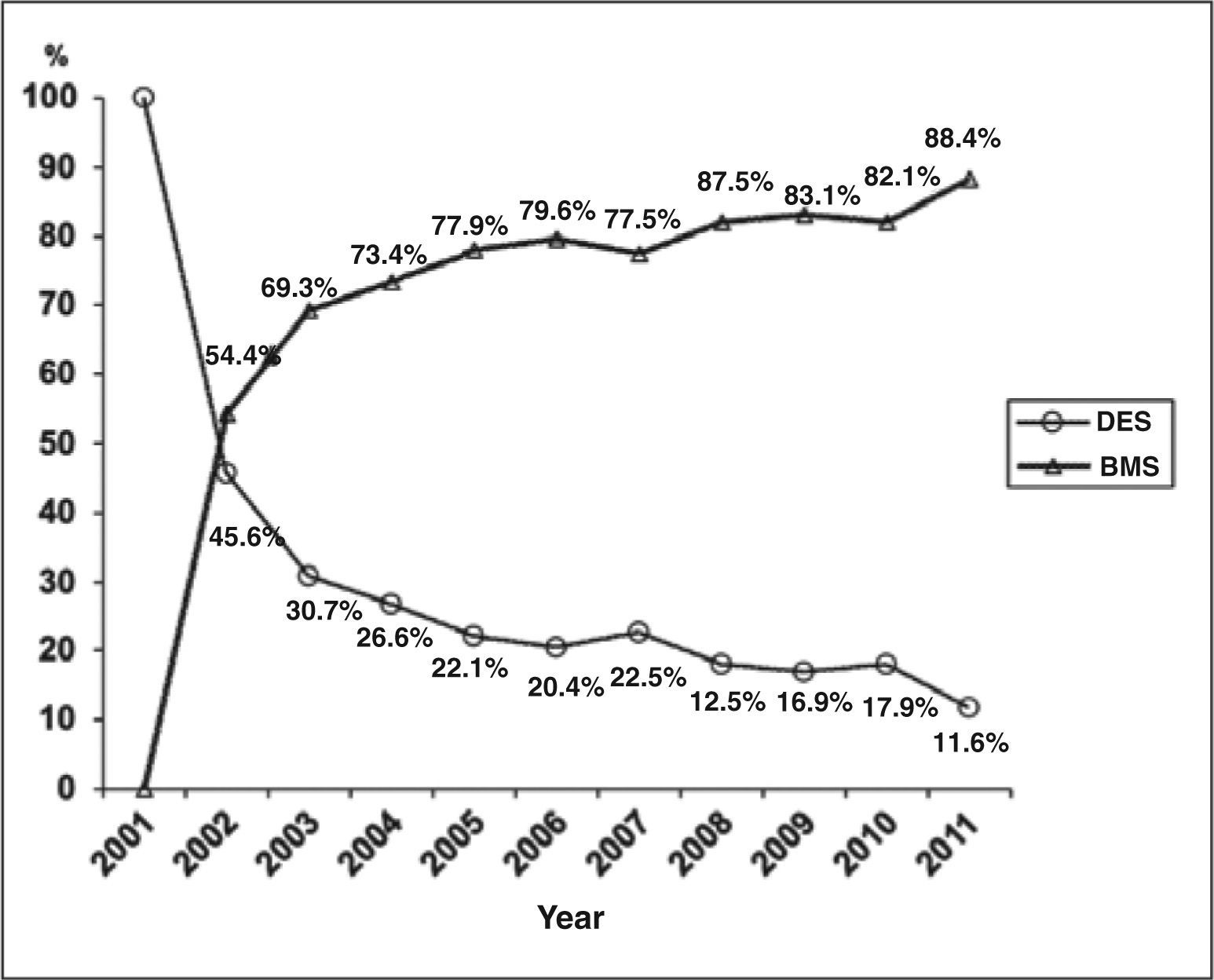
Figure 2 shows the penetration of DES in this department throughout the decade. Since the first year of its approval for clinical use, these new devices have become prevalent in the performance of PCIs, particularly since 2007, when these devices started to represent at least 70% percutaneous revascularizations, reaching close to 90% in 2011.
Dissemination of DES in interventional practice at the Hospital do Coração da Associação do Sanatório Sírio. Note that since being approved for clinical use in 2002, these new devices have become the preferred treatment choice at this institution, representing 88.4% of the stents used in 2011. BMS are restricted to patients with contraindications for the formal dual antiplatelet therapy or with surgical procedures planned within one year of the intervention. DES, drug-eluting stents; BMS, bare-metal stents.
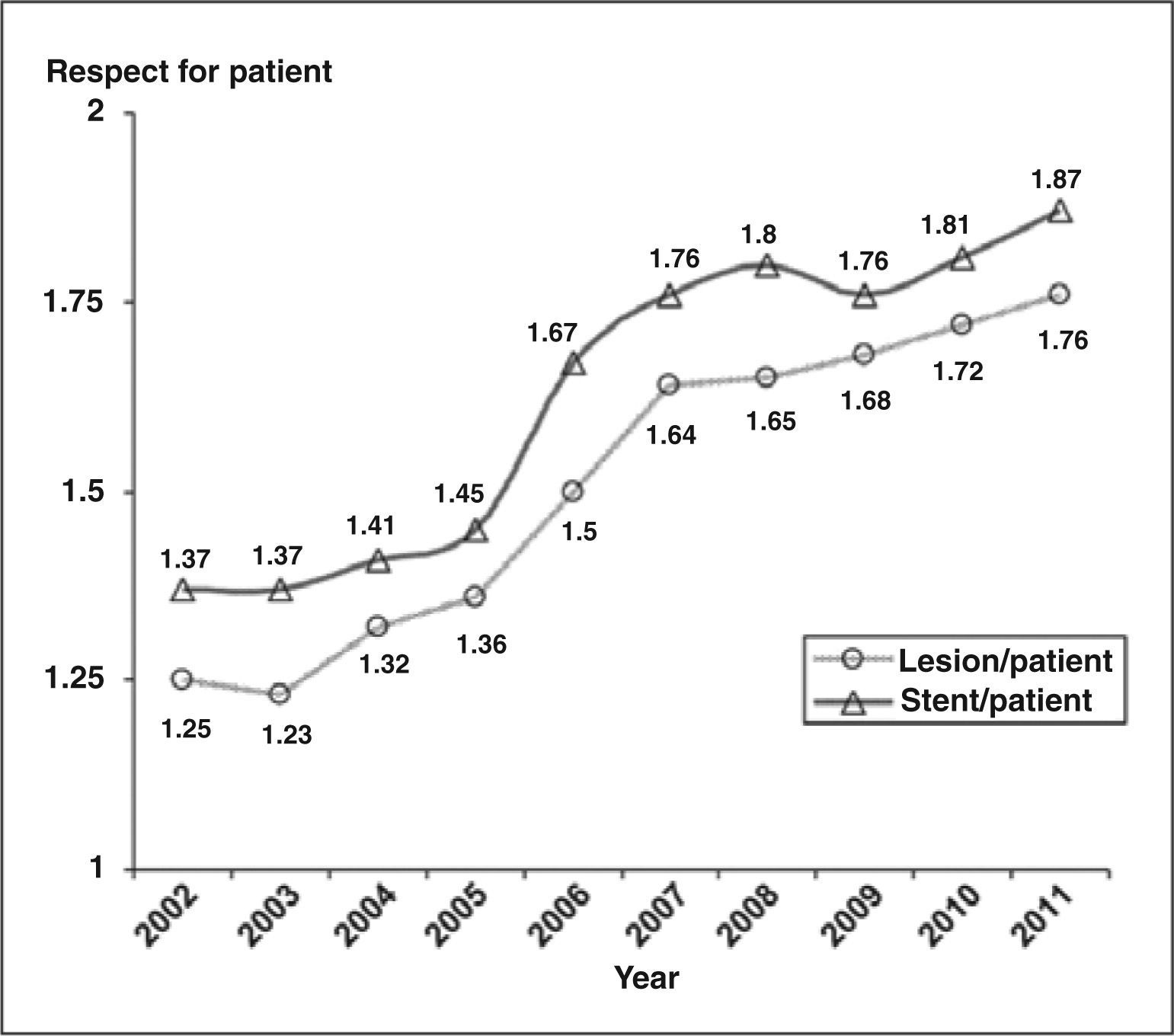
Figure 3 indirectly shows the evolution of the complexity of percutaneous procedures from 2002 to 2011. In 2002, a mean of 1.25 lesion per patient was treated, using 1.37 DES per PCI, but at the end of the decade, this service was treating 1.76 lesion per patient, using approximately two DES per intervention (1.89 DES/patient). This impact on the complexity profiles of this patient group may also be observed by assessing the SYNTAX angiographic risk scores calculated for all patients (from the DESIRE registry) with multivessel disease not previously operated upon. Overall, the mean SYNTAX in this population was 14±4.5. However, if the risk score is divided by the period, it can be observed that during the first five years of the registry (2002-2006), the mean value was 12.3±4.4, while in the last five years (2007-2011), it increased to 15.7±4.7.
An important effect of the implementation of DES in this clinical routine was the low rate of stenosis recurrence in the treated patients (i.e., the marked suppression of clinical restenosis). Among the 4,229 patients included in the study, complete clinical follow-ups were obtained in most cases (98.2% with a median follow-up of 5.2years). In 5% of cases, there was a need for further intervention in the target lesions, most of which (91%) were resolved with the implantation of another DES. The occurrence of other adverse cardiovascular events was low, particularly when considering the clinical and angiographic profiles of the assessed group (cardiovascular death, 4.1%; myocardial infarction, 6.7%; stent thrombosis, 2.4%) and the follow-up time.
DISCUSSIONUntil the advent of DES, restenosis was the main limitation of PCI, occurring in up to 30% of cases after using BMS and in 50% of cases treated with balloon catheter only.5,6
Early DES studies showed a remarkable reduction in the healing response after implanting these stents, with virtual abolition of restenosis in lower-complexity scenarios.7,8
Considering the excellent results of these initial studies, the applicability of these new devices was quickly extended to more complex scenarios in which PCI had not yet shown excellent results (e.g., diabetics, smaller vessels, restenosis, etc.) or was practiced only as an exception (e.g., left main coronary artery).9–12
However, this rapid growth in the indication of PCI and the use of these new devices did not occur homogeneously across all continents and countries. The high initial cost of these new stents represented the first barrier to their unrestricted incorporation into daily practice, particularly in countries with more constrained budgets than Brazil.
The second barrier to the broader use of these devices was related to the safety of these new tools, especially the very late types. At the end of 2006 and early 2007, several series of patients exhibited a relatively new phenomenon: thrombosis after the first month of PCI (late) and sometimes after the first year (very late), which raised the suspicion that these devices could result in higher rates of late mortality.13–20
As seen in Figures 1 and 2, the adverse global scenarios had some effect in this service’s practice as well. Between 2006 and 2007, there was a reduction of almost 20% in the PCI indication in HCor at the expense of surgical revascularization procedures (Fig. 1). However, among the patients treated with PCI, the DES maintained their hegemony as the primary tool for revascularization, with a modest reduction in their use of 2.1% compared to the previous year (79.6% in 2006 vs. 77.5% in 2007) (Figure 2).
However, this negative impact, at least in this service’s experience, was short-lived. From 2008 onward, a gradual increase in PCI indication and DES use in this service was observed, resulting in the performance of 75% of revascularizations through a catheter and the use of DES in nearly 90% of cases at this institution in 2011.
Although a definitive explanation for these observations cannot be established, it is possible to speculate on the role of the DESIRE registry in this scenario. During the study decade, data from DESIRE resulted in more than 180 studies, which were presented at national and international events and over 30 publications in national and international journals.21 The broad dissemination of this institution’s experience, with a low rate of adverse events even after a long follow-up, appears to have had an important role in the confirmation of the good results for this revolutionary technology.
In parallel, the results of several meta-analyses comparing DES and BMS that demonstrated the greater efficacy of the new devices (e.g., the safety was at least comparable to that of BMS) were published internationally.22–25
Moreover, new generations of DES appeared with structural characteristics that improved safety (e.g., decreased amounts of antiproliferative drugs, more biocompatible and/or biodegradable polymers, etc.), and without compromising the excellent effectiveness achieved by the first generation.26–28 The advent of these new stent generations, in addition to providing improved safety profiles, also stimulated competition in the DES market, which had been previously restricted to only two manufacturers. This expansion, together with the increased number of stents used, contributed to lower prices and facilitated DES use.
However, studies have shown that despite the price reduction observed in the last decade, Brazil still has the highest cost DES among the major consumer markets worldwide, which represents a paradox considering the economic environment of this country.
With the imminent implementation of these devices for use in patients treated by Unified Health System (Sistema Único de Saúde – SUS), it is expected that the last barrier (cost) will finally be removed and that it will be possible to provide more universal access to this remarkable technology.
Study limitationsThere are two main limitations related to this study: 1) the lack of detailed follow-up of the patients undergoing PCI in this hospital before 2002, when DESIRE began, and 2) the absence of a control group consisting of patients treated with BMS. The latter limitation is attributed to the fact that, from the beginning, the use of DES was defined as a standard procedure, which was not used only in the patients with a clear contraindication to prolonged dual antiplatelet therapy or in cases in which the health insurer did not authorize the use of these devices. Therefore, a control group would have been the result of an important selection bias, with limited applicability for comparisons between the instruments.
CONCLUSIONSAccording to the results of the present study, there was a significant increase in the complexity profiles of the patients treated in the last ten years and a confirmation of the long-term effectiveness of DES, notwithstanding the clinical and angiographic profiles.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.