Percutaneous coronary intervention (PCI) in ostial lesions is one of the major challenges in contemporary interventional cardiology. Despite the technological advances, ostial lesions still present a higher rate of immediate and late adverse events compared with non-ostial lesions. The objective of this study was to evaluate coronary ostial lesions treated with the Szabo technique.
MethodsTen patients treated by PCI using the Szabo technique to treat ostial lesions in main coronary arteries between October and November, 2011, were included. Aorto-ostial lesions were excluded.
ResultsOf the ten treated patients, seven were males, with ages ranging from 42 to 75 years, and 60% had acute coronary syndromes without ST-segment elevation. The circumflex artery was treated in six patients, and a 7F catheter was used in eight patients. In three patients, both guidewires twisted during the advancement of the stent to the lesion, which was solved by partially retrieving and repositioning the standard target-vessel wire. Procedural success was observed in 90% of the cases. There were no in-hospital deaths, (re) infarctions or emergency revascularisations.
ConclusionsIn this study, the Szabo technique successfully treated ostial lesions in main coronary arteries and provided adequate positioning of the stent in most cases.
Lesões Ostiais em Artérias CoronáriasPrincipais Tratadas com Técnica de Szabo
IntroduçãoA intervenção coronária percutânea (ICP) em lesões ostiais é um dos maiores desafios para a cardiologia intervencionista contemporânea. A despeito dos avanços tecnológicos, as lesões ostiais ainda apresentam maiores taxas de eventos adversos imediatos e tardios quando comparadas às lesões não ostiais. O objetivo deste estudo foi avaliar a ICP em lesões ostiais, utilizando a técnica de Szabo.
MétodosSérie de 10 pacientes, incluídos entre outubro e novembro de 2011, tratados por meio de ICP utilizando a técnica de Szabo em lesões ostiais em ramos coronários principais. Não foram abordadas lesões aorto-ostiais.
ResultadosDos 10 pacientes tratados, 7 eram do sexo masculino, com idade variando entre 42 anos e 75 anos, e 60% apresentavam síndrome coronária aguda sem supradesnivelamento do segmento ST. Artéria circunflexa foi tratada em 6 pacientes e cateter 7F foi utilizado em 8 pacientes. Em 3 pacientes não se observou progressão do stent em decorrência de torção das cordas-guia, que foi resolvida com o recuo parcial da corda-guia direcionada para a lesãoalvo e novo posicionamento. Houve sucesso do procedimento em 90% dos casos. Não ocorreram óbitos, (re)infartos ou revascularizações de urgência hospitalares.
ConclusõesNeste estudo, a técnica de Szabo permitiu tratar lesões ostiais em ramos principais das artérias coronárias com sucesso, posicionando o stent de maneira adequada na maioria dos casos.
Classically, ostial lesions are described as stenoses located within the first 3mm from the beginning of the coronary artery.1 Due to the peculiar distribution of the muscle layer of the vessel in the aorto-ostial regions and ostia of major coronary vessels (Medina classification 001 or 010),2 lesions present in these regions demonstrate both immediate and delayed increased elastic recoil after balloon dilation, which results in increased chances of procedural failure and coronary restenosis compared with non-ostial lesions.1 Stents are effective in neutralising the elastic vessel recoil, but the improper positioning of the prosthesis can lead to incomplete coverage of the ostium, resulting in higher chances of lesion recurrence at the treated site.3 Even with drug-eluting stents, the incidence of adverse cardiac events at 12 months is higher in patients with ostial lesions than in patients with non-ostial lesions.4
In 2005, Szabo et al.5 proposed a technique for the optimal placement of a stent in ostial lesions. This study aimed to evaluate the in-hospital results of this technique, its success, and possible complications.
METHODSPercutaneous coronary interventions (PCIs) were performed in patients with ostial lesions located in the main coronary branches using the Szabo technique between October and November, 2011. Aorto-ostial lesions were excluded.
Basal and Angiographic Characteristics of Patients
| Variables | n=10 |
|---|---|
| Male gender, n (%) | 7 (70) |
| Age, years | 42-75 |
| Smoking, n (%) | 4 (40) |
| Arterial hypertension, n (%) | 7 (70) |
| Diabetes mellitus, n (%) | 4 (40) |
| Dyslipidemia, n (%) | 5 (50) |
| Indication, n (%) | |
| Stable angina | 3 (30) |
| Unstable angina | 4 (40) |
| NSTEACS | 2 (20) |
| STEMI | 1 (10) |
| Diameter of guide-catheter, n (%) | |
| 6F | 2 (20) |
| 7F | 8 (80) |
| Target-artery, n (%) | |
| ADA | 2 (20) |
| Cx | 6 (60) |
| Marginal branch of Cx | 1 (10) |
| RCA (PVA/PDA) | 1 (10) |
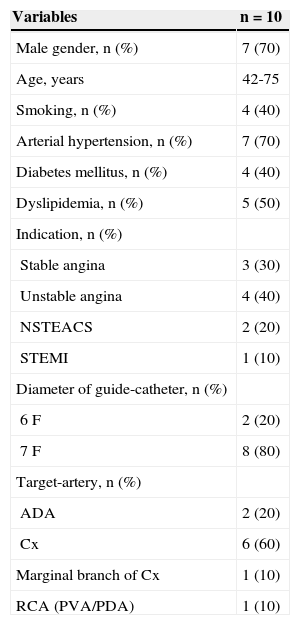
RCA=right coronary artery; Cx=circumflex artery; ADA=anterior descending artery; PDA=posterior descending artery; STEMI=ST-elevation myocardial infarction; n=number of patients; NSTEACS=non-ST elevation acute coronary syndrome; PVA=posterior ventricular artery.
The study was conducted in compliance with the Declaration of Helsinki related to research in humans and was approved by the Ethics Committee of the Hospital Beneficência Portuguesa, São Paulo, Brazil. All patients signed an informed consent prior to study enrolment.
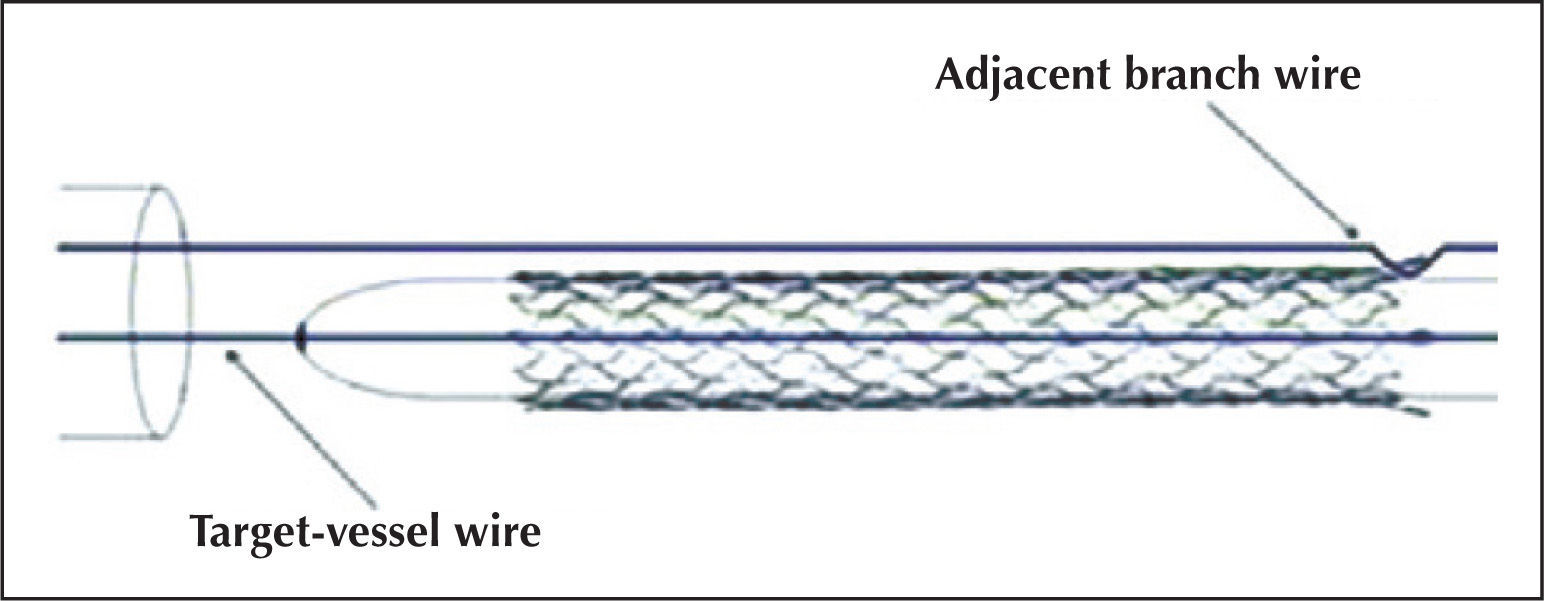
Szabo techniqueThe Szabo technique first requires preparing the stent that will be employed using two 0.014-inch guidewires. One of the guidewires is introduced into one of the proximal cells of the previously opened stent. The opening of the cells is achieved by inflating the stent at 2atm while it is still within the protective sheath, so that only the proximal cells are externalised. The enlarged proximal end of the stent is then manually adjusted while carefully observing whether it is appropriate and fixed and that there are no strut protrusions in the dilated region. The second guidewire is then introduced in the conventional manner into on the stent, which is already positioned after the coronary ostial lesion (Figure 1). Before the stent proceeds past the Y connector, the guidewire transfixed in the proximal stent cell is inserted and positioned in the coronary branch adjacent to the ostial lesion. The procedure then follows with the advancement of the stent towards the ostial lesion over the two wires until progress is prevented by the guidewire positioned in the side branch. The stent is implanted at conventional pressures, and the balloon is deflated. The guidewire of the vessel adjacent to the lesion is removed, and the stent is then post-dilated with high pressure.
– Schematic representation of stent preparation for the Szabo technique using two 0.014-inch guidewires. The first, which is directed to the adjacent side branch, crosses the first cell or proximal strut of the stent. The second, which is directed to the lesion, is positioned in the traditional manner throughout the stent.
The Liberté™ (Boston Scientific – Natik, MA, USA) bare-metal stent was used. All patients were pretreated with acetylsalicylic acid (loading dose of 200mg and a maintenance dose of 100mg/day) and clopidogrel (loading dose of 300 to 600mg and maintenance dose of 75mg/day) started on the night prior to the intervention. Unfractionated heparin (UFH) was used during the procedure at a dose of 70IU/kg to 100IU/kg. The use of glycoprotein IIb/IIIa inhibitors was at the discretion of the surgeon.
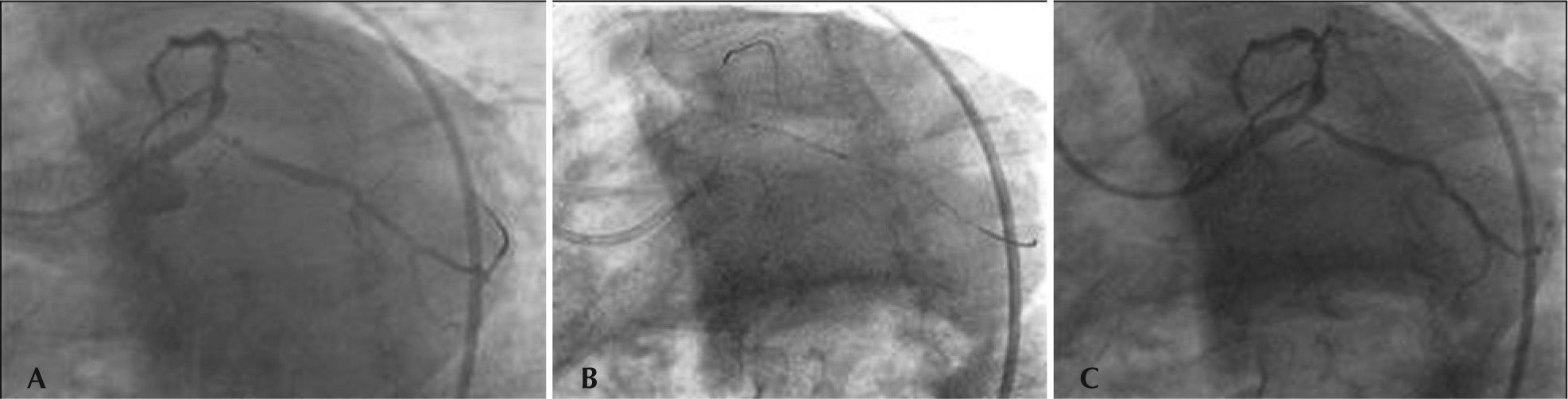
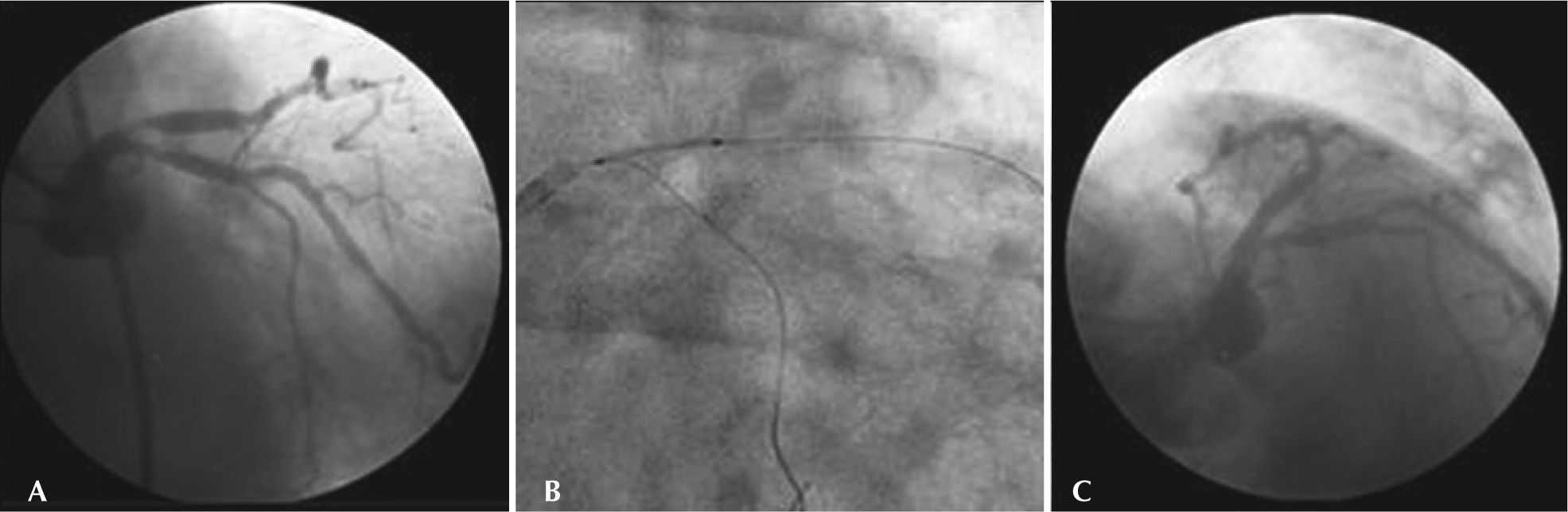
The software StentBoost™ (Philips Medical Systems – Best, the Netherlands) was used for image acquisition and processing, which consists of a fluoroscopic stent visualisation technique that creates a high-quality image of the implanted stents by superimposing frames in movement with acquisition correction, resulting in a clearer picture.6
RESULTSOf the ten treated patients, seven were males aged between 42 and 75 years, and four were diabetics. The majority of patients had acute coronary syndrome, six had unstable angina or non-ST-segment elevation acute coronary syndrome (NSTEACS), and one patient was treated in the presence of ST-segment elevation myocardial infarction (STEMI). Baseline characteristics and angiographic characteristics of patients are shown in the table.
Among the approached arteries, the circumflex artery (Figure 2) was treated in six patients, the anterior descending artery (Figure 3) in two patients, and the right coronary and the marginal branch of the circumflex artery in one patient each. The catheter diameters used were 7F in eight patients and 6F in all other cases.
Angiographic success was obtained with the proposed technique in nine patients. In the patient with STEMI, the correct positioning of the stent in the lesion was not possible due to the severe calcification and tortuosity of the left anterior descending artery, which was successfully treated with the conventional technique. In three patients, there was no stent progression due to twisting of the guidewires. This was resolved with the partial retreat of the guidewire directed to the target lesion and repositioning. Plaque shifting (snow-plough phenomenon) only occurred in one case and did not significantly affect the adjacent artery lumen.
There were no in-hospital deaths, (re)infarctions, or emergency revascularisations in this series of patients.
DISCUSSIONIn this study, it was observed that the immediate results of the Szabo technique to percutaneously treat ostial lesions of major coronary vessels were similar to those of other studies using the same technique.5,7–10
Coronary stenoses, which are located in the ostium of the main coronary branches, were already a concern of interventional cardiologists in the beginning of the last decade, including in Brazil.11–13 The use of the conventional techniques with bare-metal or drug-eluting stents in ostial lesions characteristically presents inferior results compared with those observed in non-ostial lesions, due to the difficulty of precise positioning of the stent in the target lesion.11,12
The difficulties of accurate stent placement in ostial lesions are related to problems visualising the lesion, the complex geometry with varying angles between the main and side branches, and varied plaque distribution (Medina 001 or 010).14 Several techniques have been proposed to treat ostial lesions, but all have limitations, and the best strategy remains controversial. The ideal technique would ensure complete coverage of the ostium with precise stent positioning and implantation, but also would not rely on angiography. Thus, the Szabo technique has been proposed.
Wong15 treated 41 patients with ostial lesions in main vessels with this new technique and achieved success in 97.6% of patients, which was confirmed by intracoronary ultrasound. Gutierrez-Chico et al.10 compared the results between the Szabo technique and conventional treatment guided by angiography in 156 patients with ostial lesions in main vessels (Medina 001 or 010). These authors observed a distinct advantage with the Szabo technique, with lower rates of stent malposition (6.4% vs. 41%; P<0.0001), stent protrusion in the side branch/aorta (6.4% vs. 34.6%, P<0.0003) and incomplete stent coverage of the plaque (0% vs. 7.7%).
However, Vaquerizo et al.14 not only disagreed regarding the benefits of the Szabo technique but also reported more disadvantages than advantages in 26 patients, such as asymmetric stent deformation, stent protrusion into the main branch, and risk of displacement, among others.
Two points must be stressed: the first is the learning curve required for the technique, and the second is establishing the limitations of the technique when assessing the vessel to be treated. Very calcified lesions, excessive tortuosity, and failure in pre-dilation of ostial lesions are predictors of failure with the Szabo technique. In the present study of ten cases, the only patient who was unsuccessful was the second case, due to severe tortuosity and calcification in the origin of the artery to be treated (ADA), thus characterising the lack of experience at the start of the learning curve, and consequently the indicated technique was unsuitable.
Other complications have been reported with the Szabo technique, such as decoupling of the stent from the balloon, fracture of the side branch guidewire, and stenting beyond the ostium. In this study, there were no such complications, likely because the authors systematically followed the methodological directions for the technique. For instance, according to the directions of Ferrer-Gracia et al.,16 decoupling of the stent can be prevented by using 7F guide-catheters, a technical aspect observed in 80% of the cases in this study.
Bare-metal stents were used in all cases. The patients were treated by the Brazilian Unified Health System (Sistema Único de Saúde – SUS), and and thus had no access to drug-eluting stents.
When evaluating the present results, with the aim of obtaining optimised stenting by the appropriate expansion of struts, the StentBoost technique was used.6 It was not possible to use intracoronary devices, such as intracoronary ultrasound or optical coherence tomography, which could have provided information about the proper location of the stent in the ostial position.
Study limitationsThis study had some limitations, such as the small sample size, the fact that the technique was performed in a single centre, and the absence of both clinical and angiographic follow-up after hospital discharge. However, the authors believe that, despite these limitations, the study offers the opportunity to analyse and compare data relevant to this new form of percutaneous treatment of ostial lesions. However, the need for further experience with this technique with a more robust population to assess the results is highlighted.
CONCLUSIONSIn the present study, the Szabo technique allowed the successful treatment of ostial lesions by properly positioning the stent in most cases. By carefully following the technique guidelines, the difficulties in performing the technique and the possible complications can be minimised.
However, the use of this strategy cannot be encouraged with so few treated cases. Therefore, it is necessary to reproduce these results in a larger population in other cardiac centres and to demonstrate its efficacy in randomised trials.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.