There are few studies on quality of life and costs after percutaneous coronary intervention (PCI) using different vascular accesses. We have compared procedure-related discomforts and costs of PCI using the radial or femoral approaches during hospital stay.
MethodsProspective, single center registry, including patients undergoing elective PCI. Procedure-related complaints were assessed at the end of bed rest using a specific questionnaire. Costs per unit of all the materials used in PCI were taken into account.
ResultsPatients treated by the radial approach were younger, male, and stable angina was the most common clinical presentation in both groups. Procedural duration, number of vessels treated and stents per patient were similar in both groups. There were no major vascular complications after PCI. We observed greater overall discomfort associated with the procedure (60.3% vs. 81.0%; P=0.01), back pain (1.7% vs. 17.2%; P<0.01), difficult urination (1.7% vs. 12.1%; P=0.03) and patient’s dependence to carry on basic activities (70.7% vs. 98.3%; P<0.01) during the post-procedural observation period in the femoral group. No significant differences were observed between groups when costs were compared, with or without taking into account stent-related costs.
ConclusionsPCI using the radial approach demonstrated to provide greater comfort for patients when compared to the femoral approach during hospitalization. Costs of the procedure using the two accesses were similar.
Intervenção Coronária Percutânea Pelas Vias Radial e Femoral: Comparação Entre Desconfortos Relacionados ao Procedimento e Custos
IntroduçãoEscassos são os estudos a respeito da Qualidade de Vida pós-intervenção coronária percutânea (ICP), pelas vias radial e femoral, e dos gastos comparando as duas vias de acesso. Comparamos os desconfortos relacionados ao procedimento e os custos da ICP pelos acessos radial e femoral na fase hospitalar.
MétodosRegistro prospectivo, unicêntrico, que incluiu pacientes submetidos à ICP eletiva. As queixas relacionadas ao procedimento foram avaliadas ao final do período de repouso no leito, por meio de um questionário específico. Foram computados os custos por unidade de todo o material utilizado na ICP.
ResultadosOs pacientes tratados por via radial eram mais jovens, do sexo masculino e a angina estável foi o quadro clínico mais frequentemente tratado nos dois grupos. O tempo de exame, o número de vasos tratados e stents por paciente foram semelhantes entre os grupos. Não ocorreram complicações vasculares maiores após a ICP. Observamos maior desconforto geral associado ao procedimento (60,3% vs. 81,0%; P=0,01), dor nas costas (1,7% vs. 17,2%; P<0,01), dificuldade para urinar (1,7% vs. 12,1%; P=0,03) e dependência do paciente para desempenhar atividades básicas (70,7% vs. 98,3%; P<0,01) durante o período de observação no grupo femoral. Na comparação dos gastos, não foram notadas diferenças significantes entre os grupos, com ou sem a inclusão dos custos dos stents.
ConclusõesA ICP por via radial demonstrou trazer maior conforto para o paciente comparada à via femoral, durante a fase hospitalar. Os custos dos procedimentos pelas duas vias de acesso foram semelhantes.
Percutaneous coronary intervention (PCI) via transradial approach was introduced nearly 20 years ago;1 since then, randomized studies have shown results that are superior to those of the femoral approach in terms of vascular complications and the occurrence of severe bleeding.2,3 Additionally, the radial technique has shown to be superior regarding patient quality of life (QoL) in the post-procedural period and immediately after discharge, with greater patient mobility and fewer complaints.4
In Brazil, the use of the transradial approach when performing PCI has progressively increased.5,6 However, there have been few studies on the discomforts associated with the procedure and costs when comparing the two access routes.4,7,8 Cost management is an important tool to control medical institution resources, either public or private.9
The present study aimed to compare the discomforts associated with the procedure and costs of PCIs by radial and femoral access during hospital stay.
METHODSThis was a prospective single-center registry, which included patients with coronary artery disease (stable angina or acute coronary syndrome without ST-segment elevation), successfully submitted to PCI by radial or femoral approach from August 2012 to May 2013. Procedures were performed according to current guideline recommendations.10
The inclusion criteria were patients older than 18 years, of both genders, submitted to elective PCI by radial or femoral approach. Patients undergoing primary PCI and those who had adverse cardiovascular events during procedures (cardiopulmonary arrest, acute myocardial infarction, acute pulmonary edema, and cardiogenic shock) were excluded.
The study was performed at the Laboratory of Interventional Cardiology and Adult Ward II of the Instituto Dante Pazzanese de Cardiologia, after being approved by the institution’s Research Ethics Committee. Data were collected on patients scheduled for undergoing elective PCI, after examination for hospital admission and definition of puncture technique by the interventional physician in charge of the procedure. The patient was asked to participate in the study and, upon acceptance, signed the informed consent.
Review of complaints related to the procedureComplaints related to the procedure were evaluated in all patients at the end of the bed rest period through a questionnaire, which included questions assessing general discomfort after the intervention, pain during puncture, discomfort in the limb used for the access route, back pain, and difficulty urinating. The questionnaires were administered by a single investigator (MHA), after providing standardized instructions.
ProceduresThe transradial puncture was performed using the Seldinger technique, 1cm proximal to the styloid process of the radius, using a 6F Glidesheath sheath (Terumo Medical – Tokyo, Japan). Sedation was performed with a decimal solution of diazepam. Heparin was administered at a dose of 5,000IU through the sheath and supplemented to reach 70IU/kg to 100IU/ kg. Immediately after the procedure, the radial sheath was removed and hemostasis was performed with a TR Band device (Terumo Medical, Tokyo, Japan).
The transfemoral artery puncture was performed using the standard Judkins technique, using 6F sheaths. Heparin was administered at a dose of 5,000IU through the sheath and supplemented to reach 70IU/kg to 100IU/kg. The femoral sheath was removed approximately two hours after the procedure, and homeostasis was performed by manual compression.
CostsCosts were calculated per unit for all the material used during patient follow-up period: needles (40×12mm or 30×7mm), surgical apron, surgical drape, fenestrated field (small and large), operative field, balloon catheters, intravascular ultrasound catheters, diagnostic catheters, guide-catheters, alcoholic chlorhexidine solution (volume in mL), disposable electrode, contrast medium administration equipment, saline solution equipment, equipment extension (50 or 120cm), surgical tape, injector pump extension, cerebral protection filter, 0.35-inch hydrophilic guide wire, contrast medium (Hexabrix® or Telebrix®), guidewire (0.14 or 0.35 inch), Gelco (20 or 22), femoral sheath, radial sheath, scalpel blade, manometer, medications in ampoules (adenosine, distilled water, atropine, diazepam, dipyrone, ephedrine, furosemide, glucose, metoclopramide, morphine, nitroglycerine, promethazine, protamine, and saline solution), medication in tablets/capsules (beta-blockers, angiotensin II receptor blockers, clonidine, hydralazine, angiotensin-converting enzyme inhibitor, and nitrate), medication in bottles (abciximab, heparin, hydrocortisone, lidocaine, sodium nitroprusside, and saline solution), set of metallic accessory surgical instruments (surgical tray, kidney tray, cover lid, round bowl, and tweezers), package of gauze with 20 units, pair of gloves, acrylic radioprotection protective device, control panel protection, radial compression device, syringes (1, 5, 10, or 20mL), the stent (drug-eluting or bare-metal), five-way tap, tap for saline solution, pressure transducer, and saline solution transfer connector.
DefinitionsThe time for patient preparation in the catheterization lab for the procedure was calculated from the moment the patient was placed in the supine position on the examination table until the moment when the interventionist started the procedure; the puncture time was evaluated from the time of anesthetic administration at the site of vascular access until the placement of the artery sheath; the total procedure time was measured from the arterial sheath placement until the end of the procedure.
Major vascular complications were defined as hematoma >5cm; complications at the access site that required surgical or percutaneous intervention; decrease in hemoglobin >3g/dL due to bleeding at the access site; bleeding requiring transfusion; limb ischemia and/ or compartment syndrome. Minor vascular complications were defined as hematoma <5cm, decrease in hemoglobin≤3g/dL due to bleeding at the access site, or vessel occlusion without ischemia.
Statistical analysisSPSS version 17, Minitab 16, and Excel Office 2010 were used for the statistical analyses. Categorical variables were described as frequencies and percentages and compared with the chi-squared or Fisher’s exact test, when appropriate. Continuous variables were described as mean and standard deviations and compared with analysis of variance (ANOVA). The significance level was set at 0.05.
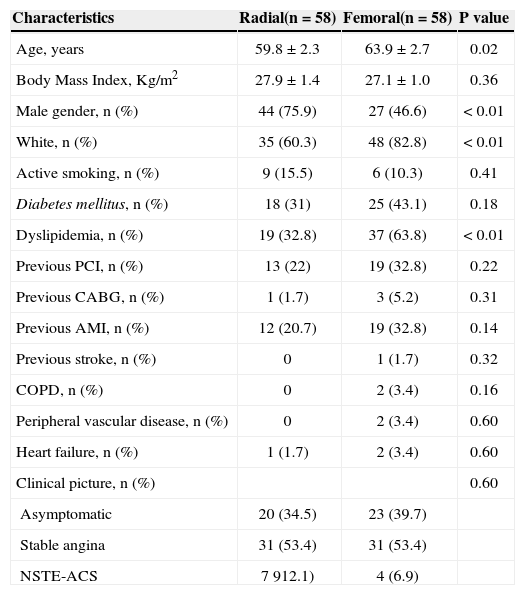
RESULTSA total of 116 patients with coronary artery disease undergoing elective PCI with stent implantation by transradial and transfemoral access routes and accepted to participate in the study protocol were included. Baseline characteristics of patients are listed in Table 1. Patients treated by the transradial approach were younger (59.8±2.3years vs. 63.9±2.7years; P=0.02), more often male (75.9% vs. 46.6%; P<0.01), and white (82.8% vs. 60.3%; P<0.01). Other clinical characteristics, except for dyslipidemia, showed no differences, and stable angina was the most common clinical picture treated in both groups.
Clinical and demographic characteristics
| Characteristics | Radial(n=58) | Femoral(n=58) | P value |
|---|---|---|---|
| Age, years | 59.8±2.3 | 63.9±2.7 | 0.02 |
| Body Mass Index, Kg/m2 | 27.9±1.4 | 27.1±1.0 | 0.36 |
| Male gender, n (%) | 44 (75.9) | 27 (46.6) | <0.01 |
| White, n (%) | 35 (60.3) | 48 (82.8) | <0.01 |
| Active smoking, n (%) | 9 (15.5) | 6 (10.3) | 0.41 |
| Diabetes mellitus, n (%) | 18 (31) | 25 (43.1) | 0.18 |
| Dyslipidemia, n (%) | 19 (32.8) | 37 (63.8) | <0.01 |
| Previous PCI, n (%) | 13 (22) | 19 (32.8) | 0.22 |
| Previous CABG, n (%) | 1 (1.7) | 3 (5.2) | 0.31 |
| Previous AMI, n (%) | 12 (20.7) | 19 (32.8) | 0.14 |
| Previous stroke, n (%) | 0 | 1 (1.7) | 0.32 |
| COPD, n (%) | 0 | 2 (3.4) | 0.16 |
| Peripheral vascular disease, n (%) | 0 | 2 (3.4) | 0.60 |
| Heart failure, n (%) | 1 (1.7) | 2 (3.4) | 0.60 |
| Clinical picture, n (%) | 0.60 | ||
| Asymptomatic | 20 (34.5) | 23 (39.7) | |
| Stable angina | 31 (53.4) | 31 (53.4) | |
| NSTE-ACS | 7 912.1) | 4 (6.9) |
PCI=percutaneous coronary intervention; CABG=coronary artery bypass grafting; AMI=acute myocardial infarction; COPD=chronic obstructive pulmonary disease; NSTE-ACS=non-ST segment elevation acute coronary syndrome.
Table 2 lists the angiographic characteristics and of the procedures. The radial group required a greater amount of diazepam for sedation (3.8±1.1mL vs. 0.4±1.1mL, P<0.01) and had longer preparation time for the procedure on the hemodynamics table (19.0±4.9min vs. 13.7±3.7min; P<0.01). The puncture and examination times did not show any differences between groups. The number of punctures, treated arteries, stents per patient, and contrast volume were also similar.
Angiographic and procedural characteristics
| Characteristics | Radial(n=58) | Femoral(n=58) | P value |
|---|---|---|---|
| Time of preparation, min. | 19.0±4.9 | 13.7±3.7 | <0.01 |
| Time of puncture, min. | 4.4±2.5 | 3.8±3.4 | 0.27 |
| Time of examination, min. | 50.6±23.6 | 47.4±23.2 | 0.46 |
| Number of punctures | 1.2±0.4 | 1.3±0.8 | 0.24 |
| Change of access route, n (%) | 4 (6.9) | 3 (5.2) | 0.70 |
| Number of treated vessels | 1.2±0.4 | 1.1±0.3 | 0.60 |
| Number of stents per patient | 1.3±0.1 | 1.3±0.2 | >0.99 |
| Amount of contrast, mL | 83.8±39.0 | 82.3±41.2 | 0.84 |
| Volume of sedatives, mL | 3.8±1.1 | 0.4±1.1 | <0.01 |
Changes in the access route were infrequent and showed no differences between groups (6.9% vs. 5.2%; P=0.70). Regarding adverse events post- procedure, there were no major vascular complications. Hematoma <5cm at the puncture site was more frequent in the radial group (6 vs. 0; P=0.03) and minor bleeding was rare, with no differences between the groups (2 vs. 1; P>0.99).
Table 3 shows the opinions of patients regarding the two techniques. A greater overall discomfort during the procedure was observed (60.3% vs. 81.0%; P=0.01), back pain (1.7% vs. 17.2%; P<0.01), difficulty urinating (1.7% vs. 12.1%; P=0.03), and dependence of the patient to perform basic activities such as eating and physiological functions (70.7% vs. 98.3%, P<0.01) in patients whose access was by femoral approach. Conversely, no differences were observed regarding pain during arterial puncture (37.9% vs. 43.1%, P=0.57) or discomfort on the access route (6.9% vs 3.4%; P=0.68) between groups. Comparing the costs between the two groups, no statistically significant differences were observed, with or without the inclusion of the cost of stents (Table 4). The authors emphasize that, in the femoral group, there was a higher use of drug-eluting stents compared to the radial group (23 vs. 32 stents) without statistical significance (P=0.09).
Patients’ opinions regarding techniques
| Opinion | Radial(n=58) | Femoral(n=58) | P value |
|---|---|---|---|
| Overall discomfort during the procedure, (%) | 35 (60.3) | 47 (81.0) | 0.01 |
| Pain during puncture, (%) | 22 (37.9) | 25 (43.1) | 0.57 |
| Discomfort at the access route, (%) | 4 (6.9) | 2 (3.4) | 0.68 |
| Back pain, (%) | 1 (1.7) | 10 (17.2) | <0.01 |
| Difficult urination, (%) | 1 (1.7) | 7 (12.1) | 0.03 |
| Patient's dependence to perform basic activities, | 41 (70.7) | 57 (98.3) | <0.01 |
Cost of procedures according to the technique
| Costs | Radial* with stent(n=58) | Femoral* with stent(n=58) | Radial** without stent(n=58) | Femoral** without stent(n=58) |
|---|---|---|---|---|
| Mean (R$) | 3.637,00 | 4.505,00 | 1.143,00 | 1.312,00 |
| Standard deviation (R$) | 3.671,00 | 4.143,00 | 274,00 | 695,00 |
| Median | 1.917,00 | 2.362,00 | 1.076,00 | 1.161,00 |
| Coefficient of variation (%) | 101 | 92 | 24 | 53 |
| Maximum value (R$) | 15.989,00 | 17.769,00 | 1.892,00 | 3.935,00 |
| Minimum value (R$) | 668,00 | 1.142,00 | 667,00 | 582,00 |
| Confidence Interval (R$) | 945,00 | 1.066,00 | 70,00 | 179,00 |
R$=Brazilian real.
The present study demonstrated that elective PCI performed through transradial approach caused less discomfort for the patient when compared to the transfemoral approach, and that both techniques had similar costs.
When access routes were compared, it was observed that use of sedatives was higher in the group of transradial approach. The radial artery is rich in adrenergic receptors, and administration of sedatives and analgesics prevents the occurrence of arterial spasm.11 At the Instituto Dante Pazzanese de Cardiologia, the use of sedation in all patients by transradial approach is routine procedure.12 In the transfemoral approach group, a lower number of patients required sedation, due to agitation during the procedure.
Regarding the characteristics of the procedures, the time required to prepare the patient for the procedure was higher in the transradial approach group, possibly explained by the routine of the institution, which recommends the concomitant preparation via femoral artery in these patients.
In the transradial group, there was a higher occurrence of hematoma <5cm when compared to the transfemoral group. In these patients, the radial compression device was used in all cases. The device requires specific skill for its adjustment and inflation, to attain perfect compression of the puncture site. The lack of expertise in the use of this device by the resident physicians in cardiology who practice in the this sector every two months may have contributed to the greater incidence of small hematomas in the radial group.
Patients from the femoral group remained in complete bed rest in the supine position, for six hours, according to institutional protocol, which explains the difficulty urinating using appropriate devices and greater dependence on the nursing team. As for the radial group, patients remained in bed for only three hours, resting only the catheterized arm, which allowed greater mobility and independence. Therefore, the transradial approach resulted in a decrease in the need for nursing care, allowing self-care by the patient.13 The transradial approach has also been associated with a higher patient quality of life and satisfaction.4 Sciahbasi et al.,14 in a comparative PCI study by transradial and transfemoral access, demonstrated that 44% of patients reported no discomfort with the radial approach. These favorable outcomes for radial access are related to the greater capacity for self-care, increased sociability during hospitalization and decreasing mental health risks due to the intervention.15
Studies on the costs of PCI have demonstrated that the transradial approach has lower costs compared to the transfemoral approach.4,7,8 The decrease in costs with the use of PCI through radial approach is related to shorter hospitalization time and lower rates of bleeding.8,16 However, when the evaluation is performed on the day of the procedure, no cost reduction is observed, similar to what was observed in the present study, which considered only the costs associated with materials and medications used on the day of PCI.16
In the present study, even though the femoral group showed a trend toward greater use of drug-eluting stents when compared to the radial group, the repeated calculation without considering the costs of used stents also showed no differences between the two techniques.
Study limitationsThe present study has limitations that should be considered. This was a single center and observational study. Patients were selected for either route of access by the interventionist physician, and neither the duration nor the total cost of hospitalization was included in the analysis.
CONCLUSIONSPercutaneous coronary intervention via transradial approach showed to be more comfortable for the patient. The procedure costs by transradial and transfemoral approaches were similar.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.