ST-segment resolution is an important predictor of infarct-related artery patency and effective microcirculatory perfusion. The aim of this study was to compare patients with and without ST-segment elevation resolution and identify variables that are associated with failure of ST-segment resolution.
MethodsBetween March 2012 and July 2013, 61 patients with ST-segment elevation acute myocardial infarction underwent primary percutaneous coronary intervention (PCI) and were included in a prospective registry. To compare the groups with and without ST-segment resolution, the chi-square test or Fisher’s exact test were used for qualitative variables and Student’s t test or Mann-Whitney’s test for quantitative variables. Simple and multiple logistic regression models were used to identify variables associated with failure of ST-segment resolution.
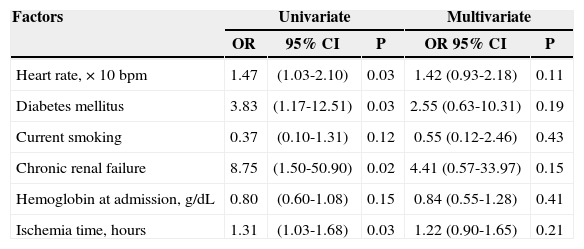
ResultsThe group of patients without ST-segment resolution had higher heart rate, higher prevalence of diabetes mellitus, chronic renal failure and a trend towards longer ischemia time. There was a higher mortality rate in patients who did not achieve ST-segment elevation resolution. In the univariate analysis, heart rate, diabetes mellitus, chronic renal failure and ischemia time were associated with increased odds of not obtaining ST-segment resolution, losing significance in the multivariate model.
ConclusionsFailure of ST-segment resolution is observed in up to one-third of patients undergoing primary PCI and requires new pharmacologic strategies or interventions to minimize it.
Resolução do Segmento ST após Intervenção Coronária PercutâneaPrimária: Características, Preditores de Insucesso e Impacto na Mortalidade
IntroduçãoA resolução do segmento ST é um importante preditor de patência da artéria relacionada ao infarto e de perfusão efetiva da microcirculação. O objetivo deste trabalho foi comparar pacientes com e sem resolução do segmento ST e identificar variáveis que se associam à não resolução do ST.
MétodosEntre março de 2012 e julho de 2013, 61 pacientes com infarto agudo do miocárdio com elevação do segmento ST foram submetidos à intervenção coronária percutânea (ICP) primária e incluídos em um registro prospectivo. Para comparar os grupos com e sem resolução do segmento ST, foi utilizado o teste qui-quadrado ou exato de Fisher, para as variáveis qualitativas, e o teste t de Student ou de Mann-Whitney, para variáveis quantitativas. Para identificar variáveis associadas à não resolução do ST, foram ajustados modelos de regressão logística simples e múltipla.
ResultadosO grupo de pacientes sem resolução do segmento ST apresentou maior frequência cardíaca, maior prevalência de diabetes mellitus, de insuficiência renal crônica e tendência a maior tempo de isquemia. Observou-se maior mortalidade hospitalar entre pacientes que não obtiveram resolução do ST. Pela análise univariada, as variáveis frequência cardíaca, diabetes mellitus, insuficiência renal crônica e tempo de isquemia associaram-se à maior chance de não resolução do ST, perdendo significância no modelo multivariado.
ConclusõesA não resolução do segmento ST pode ocorrer em até um terço dos pacientes submetidos à ICP primária, requerendo o advento de novas estratégias farmacológicas ou de intervenção capazes de minimizá-la.
Compared to fibrinolysis, percutaneous coronary intervention (PCI) promotes a more early and sustained restoration of epicardial flow in the target vessel, and is widely accepted as the preferred strategy in the treatment of acute myocardial infarction (AMI).1,2 The resolution of the ST-segment after the institution of reperfusion therapy is an important predictor of patency of the artery related to the event and of effective microcirculatory perfusion.3
The analysis of ST-segment resolution on the electrocardiogram (ECG) consists of a simple tool, of easy use and low cost, able to document success of the epicardial reperfusion and tissue reperfusion after primary PCI.4 The persistence of ST-segment elevation on the ECG, despite the restoration of a normal epicardial flow, signifies a poor prognosis; such persistence is known to be associated with larger infarct size and higher combined rate of severe cardiovascular adverse events.5
In a contemporary context for the application of primary PCI, characterized by an aggressive antithrombotic therapy, manual aspiration thrombectomy, intracoronary adenosine, and ample use of the radial access, this study aimed to determine the percentage of failure in ST-segment resolution, its predictors, and the impact on in-hospital and late mortality.
METHODSBetween March 2012 and July 2013, patients with AMI with ST-segment elevation≥1mm in two contiguous leads of the frontal plane or≥2mm in precordial leads, with symptoms duration<12 hours, underwent primary PCI and were included in a local controlled prospective registry. A 12-lead ECG, plus leads V3R, V4R, V7, and V8 in the case of lower AMI, was performed at admission and 30 to 60 minutes after the conclusion of the procedure. Patients with left branch block or pacemaker rhythm, surgical myocardial revascularization, cardiogenic shock, or life expectation<six months were excluded. The electrocardiographic analysis followed the prevalent normative guidelines,6 considering complete a ST-segment resolution>70%.
This study aimed to compare demographic and procedure-related characteristics of patients with and without complete ST-segment resolution after performing primary PCI, and to identify the variables that were associated to non-ST-resolution. The secondary objective was to determine its impact on infarct size, measured by maximum peak of CK-MB, length of stay, and in-hospital mortality after 30 days, six months and one year of follow-up.
Ischemia time was defined as the interval between the onset of symptoms and the crossing of the lesion with a pre-dilation balloon, manual thrombus aspiration catheter, or stent. Door-to-balloon time was defined as the interval between hospital admission and the crossing of the lesion with a pre-dilation balloon catheter, manual thrombus aspiration catheter, or stent. A CK-MB analysis was performed every six hours until the occurrence of a reduction in the levels of this biomarker. The choice of antiplatelet therapy, use of prophylactic intracoronary adenosine, manual aspiration thrombectomy, and the access route were left to the discretion of the surgeon.
Statistical AnalysisQualitative variables were summarized as absolute frequencies and percentages. The quantitative data were expressed as means±standard deviation or medians and interquartile ranges (25th percentile –75th percentile) according to distribution for each variable. To compare the groups with and without resolution of the ST-segment, the chi-squared test or Fisher’s exact test were used for qualitative variables, and Student’s t-test or the Mann-Whitney test were used for quantitative variables.
To identify variables associated with ST-segment resolution, simple (univariate approach) and multiple (multivariate analysis) logistic regression models were adjusted. The results were expressed as odds ratios (OR) and 95% confidence intervals (95% CI). The level of significance was 0.05. The statistical program used to perform the calculations was the SPSS for Windows, version 19.0.
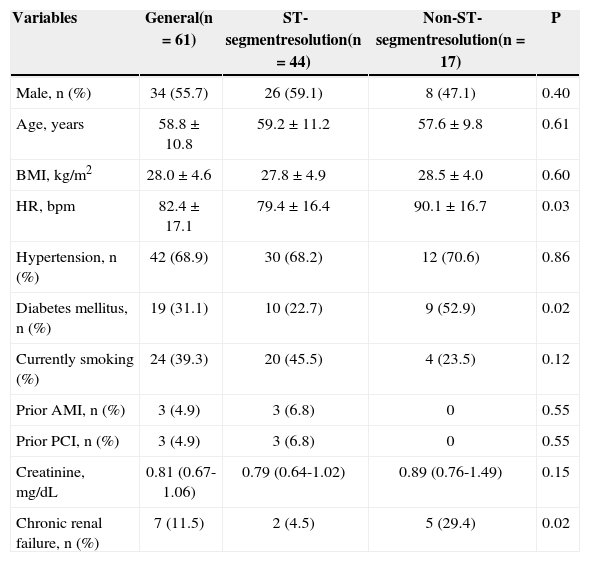
RESULTSComparisons among patients with and without ST-segment resolutionTable 1 shows a comparison among patients with and without ST-segment resolution regarding baseline clinical characteristics. It was observed that the group of patients without ST-segment resolution had, on average, a higher heart rate and higher prevalence of diabetes mellitus and of chronic renal failure.
Baseline clinical characteristics
| Variables | General(n=61) | ST-segmentresolution(n=44) | Non-ST-segmentresolution(n=17) | P |
|---|---|---|---|---|
| Male, n (%) | 34 (55.7) | 26 (59.1) | 8 (47.1) | 0.40 |
| Age, years | 58.8±10.8 | 59.2±11.2 | 57.6±9.8 | 0.61 |
| BMI, kg/m2 | 28.0±4.6 | 27.8±4.9 | 28.5±4.0 | 0.60 |
| HR, bpm | 82.4±17.1 | 79.4±16.4 | 90.1±16.7 | 0.03 |
| Hypertension, n (%) | 42 (68.9) | 30 (68.2) | 12 (70.6) | 0.86 |
| Diabetes mellitus, n (%) | 19 (31.1) | 10 (22.7) | 9 (52.9) | 0.02 |
| Currently smoking (%) | 24 (39.3) | 20 (45.5) | 4 (23.5) | 0.12 |
| Prior AMI, n (%) | 3 (4.9) | 3 (6.8) | 0 | 0.55 |
| Prior PCI, n (%) | 3 (4.9) | 3 (6.8) | 0 | 0.55 |
| Creatinine, mg/dL | 0.81 (0.67-1.06) | 0.79 (0.64-1.02) | 0.89 (0.76-1.49) | 0.15 |
| Chronic renal failure, n (%) | 7 (11.5) | 2 (4.5) | 5 (29.4) | 0.02 |
BMI=body mass index; HR=heart rate; bpm=beats per minute; AMI=acute myocardial infarction; PCI=percutaneous coronary intervention.
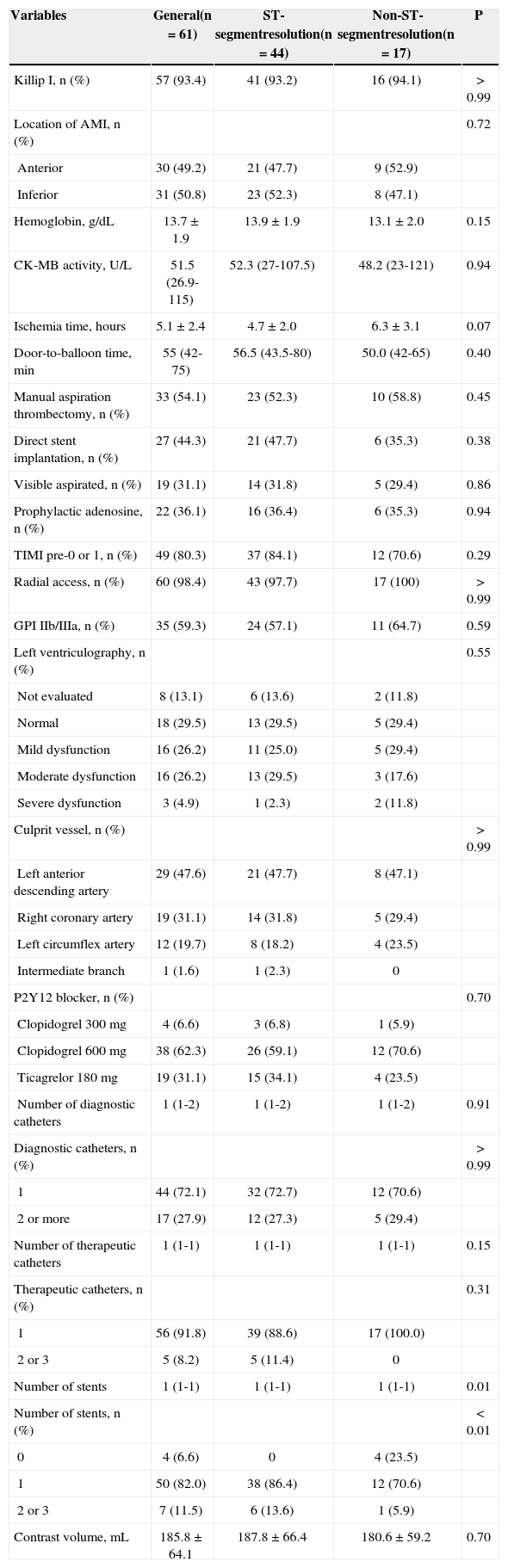
With respect to the procedure and angiographic characteristics (Table 2), a statistically significant difference was observed only in the number of stents used. A trend of longer ischemia time among patients without ST-segment resolution (4.7±2.0hours vs. 6.3±3.1hours; P=0.07) was detected.
Angiographic and procedure characteristics
| Variables | General(n=61) | ST-segmentresolution(n=44) | Non-ST-segmentresolution(n=17) | P |
|---|---|---|---|---|
| Killip I, n (%) | 57 (93.4) | 41 (93.2) | 16 (94.1) | > 0.99 |
| Location of AMI, n (%) | 0.72 | |||
| Anterior | 30 (49.2) | 21 (47.7) | 9 (52.9) | |
| Inferior | 31 (50.8) | 23 (52.3) | 8 (47.1) | |
| Hemoglobin, g/dL | 13.7±1.9 | 13.9±1.9 | 13.1±2.0 | 0.15 |
| CK-MB activity, U/L | 51.5 (26.9-115) | 52.3 (27-107.5) | 48.2 (23-121) | 0.94 |
| Ischemia time, hours | 5.1±2.4 | 4.7±2.0 | 6.3±3.1 | 0.07 |
| Door-to-balloon time, min | 55 (42-75) | 56.5 (43.5-80) | 50.0 (42-65) | 0.40 |
| Manual aspiration thrombectomy, n (%) | 33 (54.1) | 23 (52.3) | 10 (58.8) | 0.45 |
| Direct stent implantation, n (%) | 27 (44.3) | 21 (47.7) | 6 (35.3) | 0.38 |
| Visible aspirated, n (%) | 19 (31.1) | 14 (31.8) | 5 (29.4) | 0.86 |
| Prophylactic adenosine, n (%) | 22 (36.1) | 16 (36.4) | 6 (35.3) | 0.94 |
| TIMI pre-0 or 1, n (%) | 49 (80.3) | 37 (84.1) | 12 (70.6) | 0.29 |
| Radial access, n (%) | 60 (98.4) | 43 (97.7) | 17 (100) | > 0.99 |
| GPI IIb/IIIa, n (%) | 35 (59.3) | 24 (57.1) | 11 (64.7) | 0.59 |
| Left ventriculography, n (%) | 0.55 | |||
| Not evaluated | 8 (13.1) | 6 (13.6) | 2 (11.8) | |
| Normal | 18 (29.5) | 13 (29.5) | 5 (29.4) | |
| Mild dysfunction | 16 (26.2) | 11 (25.0) | 5 (29.4) | |
| Moderate dysfunction | 16 (26.2) | 13 (29.5) | 3 (17.6) | |
| Severe dysfunction | 3 (4.9) | 1 (2.3) | 2 (11.8) | |
| Culprit vessel, n (%) | > 0.99 | |||
| Left anterior descending artery | 29 (47.6) | 21 (47.7) | 8 (47.1) | |
| Right coronary artery | 19 (31.1) | 14 (31.8) | 5 (29.4) | |
| Left circumflex artery | 12 (19.7) | 8 (18.2) | 4 (23.5) | |
| Intermediate branch | 1 (1.6) | 1 (2.3) | 0 | |
| P2Y12 blocker, n (%) | 0.70 | |||
| Clopidogrel 300mg | 4 (6.6) | 3 (6.8) | 1 (5.9) | |
| Clopidogrel 600mg | 38 (62.3) | 26 (59.1) | 12 (70.6) | |
| Ticagrelor 180mg | 19 (31.1) | 15 (34.1) | 4 (23.5) | |
| Number of diagnostic catheters | 1 (1-2) | 1 (1-2) | 1 (1-2) | 0.91 |
| Diagnostic catheters, n (%) | > 0.99 | |||
| 1 | 44 (72.1) | 32 (72.7) | 12 (70.6) | |
| 2 or more | 17 (27.9) | 12 (27.3) | 5 (29.4) | |
| Number of therapeutic catheters | 1 (1-1) | 1 (1-1) | 1 (1-1) | 0.15 |
| Therapeutic catheters, n (%) | 0.31 | |||
| 1 | 56 (91.8) | 39 (88.6) | 17 (100.0) | |
| 2 or 3 | 5 (8.2) | 5 (11.4) | 0 | |
| Number of stents | 1 (1-1) | 1 (1-1) | 1 (1-1) | 0.01 |
| Number of stents, n (%) | < 0.01 | |||
| 0 | 4 (6.6) | 0 | 4 (23.5) | |
| 1 | 50 (82.0) | 38 (86.4) | 12 (70.6) | |
| 2 or 3 | 7 (11.5) | 6 (13.6) | 1 (5.9) | |
| Contrast volume, mL | 185.8±64.1 | 187.8±66.4 | 180.6±59.2 | 0.70 |
AMI=acute myocardial infarction; GPI=glycoprotein inhibitor.
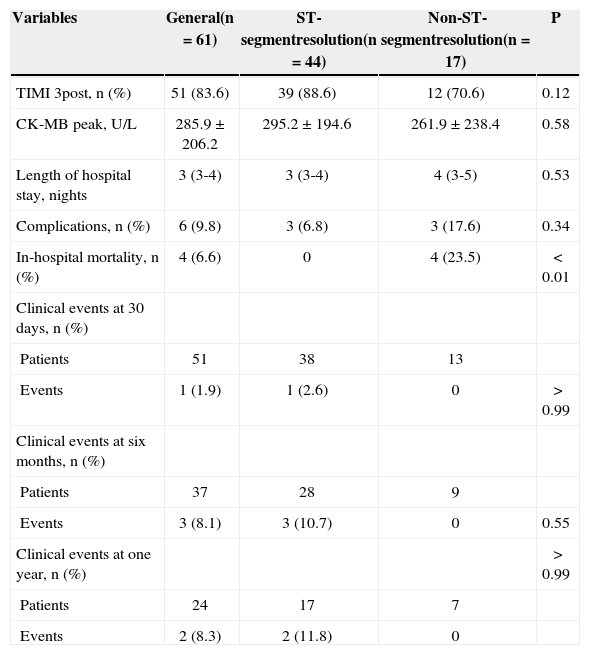
Regarding the results and the clinical outcome, a higher in-hospital mortality rate among patients who did not achieve ST-segment resolution was observed (Table 3).
Outcomes of efficacy, safety, and evolution
| Variables | General(n=61) | ST-segmentresolution(n=44) | Non-ST-segmentresolution(n=17) | P |
|---|---|---|---|---|
| TIMI 3post, n (%) | 51 (83.6) | 39 (88.6) | 12 (70.6) | 0.12 |
| CK-MB peak, U/L | 285.9±206.2 | 295.2±194.6 | 261.9±238.4 | 0.58 |
| Length of hospital stay, nights | 3 (3-4) | 3 (3-4) | 4 (3-5) | 0.53 |
| Complications, n (%) | 6 (9.8) | 3 (6.8) | 3 (17.6) | 0.34 |
| In-hospital mortality, n (%) | 4 (6.6) | 0 | 4 (23.5) | < 0.01 |
| Clinical events at 30 days, n (%) | ||||
| Patients | 51 | 38 | 13 | |
| Events | 1 (1.9) | 1 (2.6) | 0 | > 0.99 |
| Clinical events at six months, n (%) | ||||
| Patients | 37 | 28 | 9 | |
| Events | 3 (8.1) | 3 (10.7) | 0 | 0.55 |
| Clinical events at one year, n (%) | > 0.99 | |||
| Patients | 24 | 17 | 7 | |
| Events | 2 (8.3) | 2 (11.8) | 0 |
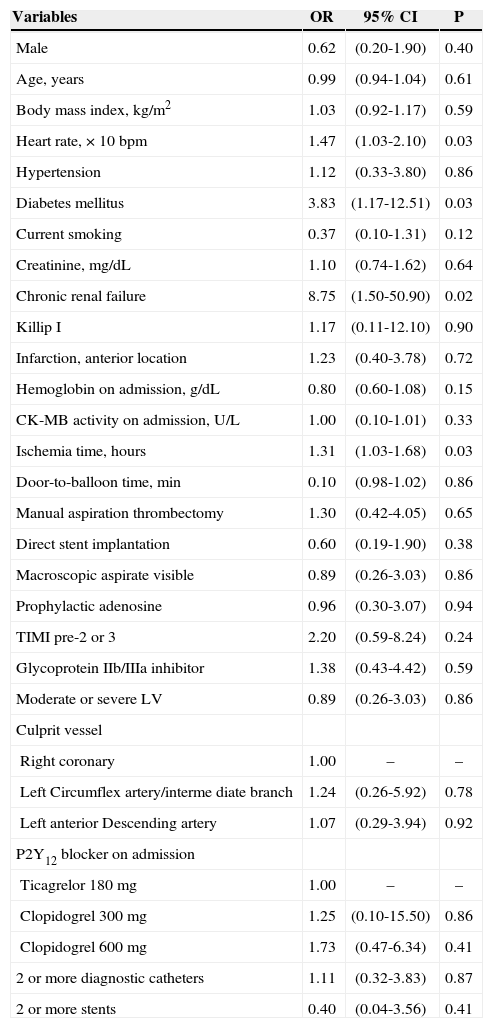
This part of the analysis sought to identify, among the clinical, angiographic and procedural characteristics, the factors associated with the increased probability of non-ST-segment resolution. Initially, the isolated effect of each variable were investigated by simple logistic regression models (univariate analysis), considering as dependent variable the non-ST-segment resolution. The results are shown in Table 4.
Factors associated with non-ST-segment resolution (univariate analysis)
| Variables | OR | 95% CI | P |
|---|---|---|---|
| Male | 0.62 | (0.20-1.90) | 0.40 |
| Age, years | 0.99 | (0.94-1.04) | 0.61 |
| Body mass index, kg/m2 | 1.03 | (0.92-1.17) | 0.59 |
| Heart rate, × 10bpm | 1.47 | (1.03-2.10) | 0.03 |
| Hypertension | 1.12 | (0.33-3.80) | 0.86 |
| Diabetes mellitus | 3.83 | (1.17-12.51) | 0.03 |
| Current smoking | 0.37 | (0.10-1.31) | 0.12 |
| Creatinine, mg/dL | 1.10 | (0.74-1.62) | 0.64 |
| Chronic renal failure | 8.75 | (1.50-50.90) | 0.02 |
| Killip I | 1.17 | (0.11-12.10) | 0.90 |
| Infarction, anterior location | 1.23 | (0.40-3.78) | 0.72 |
| Hemoglobin on admission, g/dL | 0.80 | (0.60-1.08) | 0.15 |
| CK-MB activity on admission, U/L | 1.00 | (0.10-1.01) | 0.33 |
| Ischemia time, hours | 1.31 | (1.03-1.68) | 0.03 |
| Door-to-balloon time, min | 0.10 | (0.98-1.02) | 0.86 |
| Manual aspiration thrombectomy | 1.30 | (0.42-4.05) | 0.65 |
| Direct stent implantation | 0.60 | (0.19-1.90) | 0.38 |
| Macroscopic aspirate visible | 0.89 | (0.26-3.03) | 0.86 |
| Prophylactic adenosine | 0.96 | (0.30-3.07) | 0.94 |
| TIMI pre-2 or 3 | 2.20 | (0.59-8.24) | 0.24 |
| Glycoprotein IIb/IIIa inhibitor | 1.38 | (0.43-4.42) | 0.59 |
| Moderate or severe LV | 0.89 | (0.26-3.03) | 0.86 |
| Culprit vessel | |||
| Right coronary | 1.00 | – | – |
| Left Circumflex artery/interme diate branch | 1.24 | (0.26-5.92) | 0.78 |
| Left anterior Descending artery | 1.07 | (0.29-3.94) | 0.92 |
| P2Y12 blocker on admission | |||
| Ticagrelor 180mg | 1.00 | – | – |
| Clopidogrel 300mg | 1.25 | (0.10-15.50) | 0.86 |
| Clopidogrel 600mg | 1.73 | (0.47-6.34) | 0.41 |
| 2 or more diagnostic catheters | 1.11 | (0.32-3.83) | 0.87 |
| 2 or more stents | 0.40 | (0.04-3.56) | 0.41 |
OR=odds ratio; IC 95%=confidence interval of 95%; bpm=beats per minute.
As expected, according to the comparison between groups, the variables heart rate, diabetes mellitus, and chronic renal failure were associated with increased probability of non ST-segment resolution. In addition, the ischemia time was also significant. The variables prior AMI, prior PCI, route of access, and therapeutic catheters could not be analyzed due to the low frequency in some of their categories.
Variables with P<0.20 in the univariate analysis were selected for the multivariate model, in which the effects were analyzed simultaneously (Table 5). In this model, all variables lost their importance and ceased to be significant according to the usual significance level of 0.05. This can be explained by the low statistical power to detect differences, caused by the increase in the number of parameters in the model.
Factors associated with non-ST-segment resolution. Results of simple (univariate analysis) and multiple (multivariate analysis) logistic regression models
| Factors | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| OR | 95% CI | P | OR 95% CI | P | |
| Heart rate, × 10bpm | 1.47 | (1.03-2.10) | 0.03 | 1.42 (0.93-2.18) | 0.11 |
| Diabetes mellitus | 3.83 | (1.17-12.51) | 0.03 | 2.55 (0.63-10.31) | 0.19 |
| Current smoking | 0.37 | (0.10-1.31) | 0.12 | 0.55 (0.12-2.46) | 0.43 |
| Chronic renal failure | 8.75 | (1.50-50.90) | 0.02 | 4.41 (0.57-33.97) | 0.15 |
| Hemoglobin at admission, g/dL | 0.80 | (0.60-1.08) | 0.15 | 0.84 (0.55-1.28) | 0.41 |
| Ischemia time, hours | 1.31 | (1.03-1.68) | 0.03 | 1.22 (0.90-1.65) | 0.21 |
OR=odds ratio; IC 95%=confidence interval of 95%.
In order to obtain a more consistent model, the non-significant variables were excluded, step-by-step, until the achievement of a reduced model. In this model, only diabetes (OR=3.83, 95% CI, 1.17 to 12.51, P=0.19) and chronic renal failure (OR=8.75, 95% CI, 1.50 to 50.90, P=0.15) remained significant. Importantly, although they were significant, the estimates were not very accurate (very wide CIs), and the ORs may be overestimated. Still, it is clear that diabetes mellitus and chronic renal failure are factors associated with non-ST-segment resolution.
DISCUSSIONIncomplete ST-segment resolution after primary PCI correlates strongly with mortality and reinfarction, regardless of the degree of patency of the target vessel.5 In a series from real-world practice, characterized by a mean age of 59 years, 31% diabetics, 11% with chronic renal failure, ischemia time of 5 hours, and median door-to-balloon time of 55 minutes, the rate of obtaining a final Thrombolysis in Myocardial Infarction (TIMI) flow 3 was 84%, with ST-segment resolution>70% in 72% of the sample. Diabetes mellitus, chronic renal failure, elevated heart rate, longer ischemic time, and fewer implanted stents were the characteristics most commonly observed in patients who did not achieve ST-segment resolution; the first two factors are important predictors of failure.
In pre-specified analysis of the randomized trial “Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction” (HORIZONS-AMI), comprising 2,484 of 3,345 patients undergoing primary PCI, the rate of resolution of ST-segment>70% was 50.5%, with a lower incidence of death, reinfarction, target vessel revascularization, and stent thrombosis at three years in this group.7 In the same clinical trial, final TIMI flow 3 was achieved in 87.1% of the sample, and age, anterior wall AMI, TIMI pre-0/1, and extent of injury were independent predictors of final TIMI flow<3 by multivariate analysis.8 In an Argentinean multicenter registry, despite obtaining a final TIMI flow 3 in 90% of the sample, the rate of complete ST-segment resolution was 48.5%.9
The present series displays characteristics that differ from those previously mentioned, which could explain the high percentage of complete ST-segment resolution. Initially, the sample of patients undergoing the procedure was restricted to within 12 hours after onset of symptoms. The mean ischemia time was 5.1hours and the median door-to-balloon time was only 55 minutes, favored by the logistical conditions set forth in a previous publication.10 Moreover, manual aspiration thrombectomy was used in 54% of the sample, and glycoprotein IIb/IIIa inhibitors and adenosine were administered prophylactically to 59% and 36% of cases, respectively.
In fact, in the electrocardiographic sub-analysis of the trial Platelet Inhibition and Patient Outcomes (PLATO),11 70% of patients randomized in the interval of 3-6 hours from the onset of symptoms exhibited ST-segment resolution, compared to 51% of those randomized after 6 hours. Meanwhile, a meta-analysis including 18 randomised trials and 3,936 patients showed that manual thrombus aspiration, compared to conventional primary PCI, promotes higher TIMI 3 final myocardial blush (63.6% vs. 48.5%; P<0.0001) and higher complete ST-segment resolution (55.8% vs. 44.3%; P<0.0001).12
Glycoprotein IIb/IIIa inhibitors, despite lack of consistent evidence to justify their routine indication, find an application niche in patients classified as high risk.13,14 Finally, in the “Intracoronary Nitroprusside Versus Adenosine in Acute Myocardial Infarction”(REOPEN-AMI) randomized trial, 71% of patients who received intracoronary adenosine after thrombus aspiration exhibited ST-segment resolution>70%, compared to 54% in the group receiving sodium nitroprusside and to 51% of the saline group (P=0.009), limiting the reperfusion injury, as measured by the occurrence of angiographic microvascular obstruction (TIMI flow≤2 or 3 with TIMI myocardial blush<2).15
Limitations of the studyApart from the non-random sampling, the main limitation of this study resided in the small size of their sample, making it impossible to identify potential determinant variables for failure of complete ST-segment resolution after primary PCI.
CONCLUSIONSIncomplete resolution of ST-segment may occur in up to one-third of patients undergoing primary percutaneous coronary intervention, regardless of the restoration of TIMI 3 final epicardial flow. The predictor variables diabetes mellitus, chronic renal failure, heart rate, and ischemia time are associated with incomplete resolution of ST-segment elevation, requiring new pharmacological or interventional strategies to minimize this condition.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.