Aspiration thrombectomy is recommended as an adjunctive method in patients undergoing primary percutaneous coronary intervention (PCI), however, thrombus aspiration failure is relatively frequent. The objective of this study was to evaluate the rate and identify predictors of failed thrombus aspiration in a contemporaneous series of patients.
MethodsProspective cohort study including consecutive patients with acute ST-segment elevation myocardial infarction undergoing primary PCI with thrombus aspiration from December 2009 to December 2011. Aspiration thrombectomy was performed at the operator’s discretion and success was defined as effective thrombus aspiration by a dedicated catheter with the achievement of a final TIMI flow > 0.
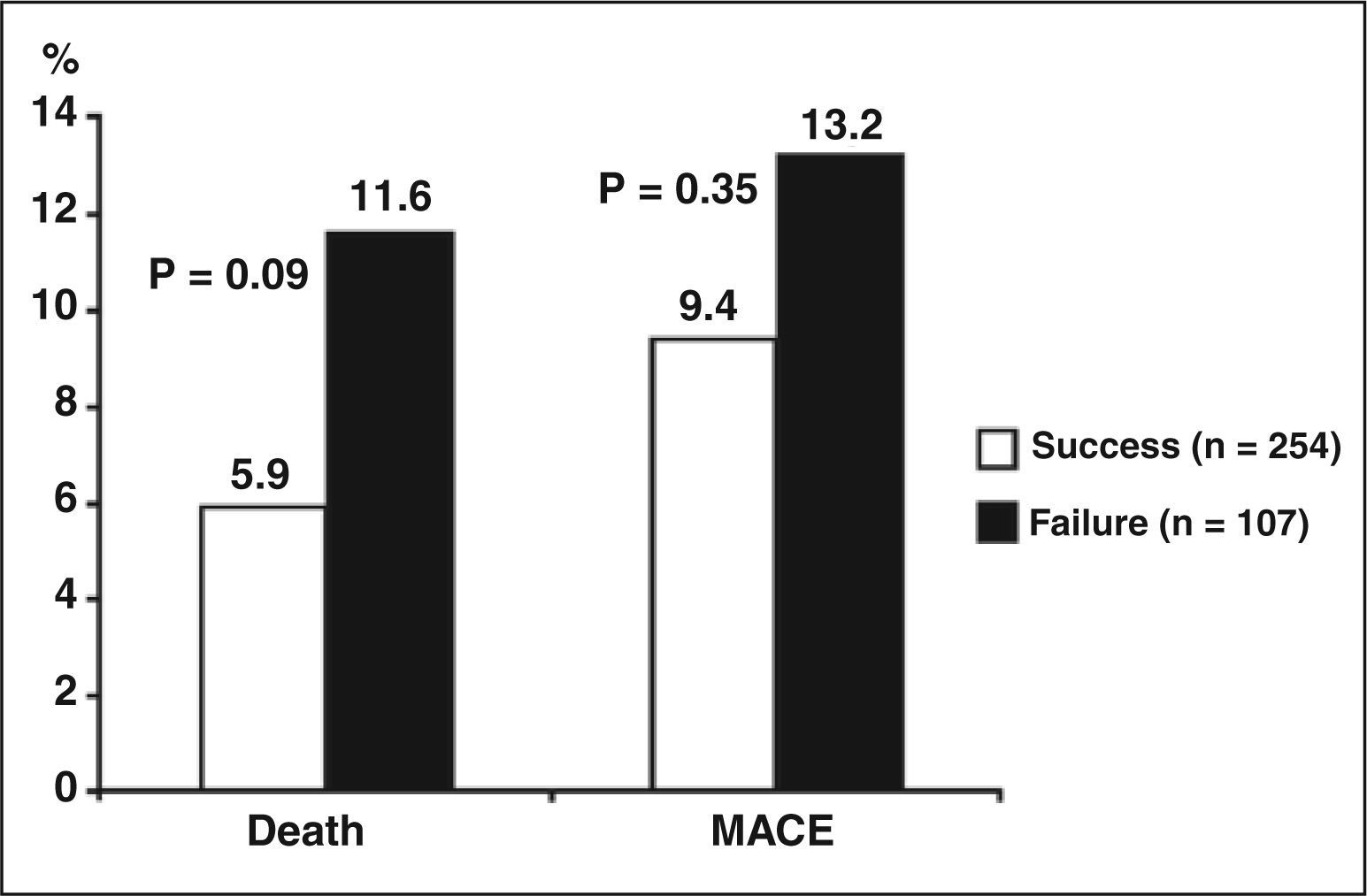
Results1,055 primary PCIs were performed and aspiration thrombectomy was used in 37% of cases with a success rate of 70%. Aspiration thrombectomy success was observed in 254 patients whereas failure was observed in 107 patients. Aspiration thrombectomy failure was associated with age, hypertension, diabetes mellitus, dyslipidemia, previous PCI, TIMI risk score, Killip IV, leukocyte count, serum fibrinogen, target vessel reference diameter and preprocedural TIMI 3 flow. Patients with failed thrombus aspiration had a trend towards higher mortality (11.6% vs. 5.9%; P = 0.09).
ConclusionsAspiration thrombectomy failure during primary PCI was observed in 30% of the cases and was associated with a trend towards higher mortality. The identification of clinical, laboratory and angiographic predictors may help improve these devices and the technique and enable better patient selection.
Preditores de Insucesso de Tromboaspiração em PacientesSubmetidos à Intervenção Coronária Percutânea Primária
IntroduçãoA tromboaspiração é recomendada como método adjunto à intervenção coronária percutânea (ICP) primária, mas o insucesso em recuperar trombos é relativamente frequente. O objetivo deste estudo foi avaliar as taxas de insucesso de tromboaspiração e identificar seus preditores, em uma série contemporânea de pacientes.
MétodosEstudo de coorte prospectivo que incluiu pacientes consecutivos atendidos com infarto agudo do miocárdio com elevação do segmento ST e submetidos à ICP primária com tromboaspiração no período de dezembro de 2009 a dezembro de 2011. Os procedimentos de tromboaspiração foram realizados por decisão do operador, e o sucesso foi definido como aspiração efetiva de trombo pelo cateter dedicado, com recuperação do fluxo coronário (fluxo TIMI > 0).
ResultadosForam realizadas 1.055 ICPs primárias, sendo que a tromboaspiração foi utilizada em 37% dos casos, com taxa de sucesso de 70%. Foram identificados 254 pacientes com sucesso e 107 com insucesso da tromboaspiração. Insucesso de tromboaspiração foi associado a: idade, hipertensão, diabetes mellitus, dislipidemia, ICP prévia, escore de risco TIMI, Killip IV, contagem de leucócitos, fibrinogênio sérico, diâmetro de referência do vaso-alvo e TIMI 3 préprocedimento. Pacientes com insucesso da tromboaspiração apresentaram tendência a maior mortalidade (11,6% vs. 5,9%; P = 0,09).
ConclusõesInsucesso de tromboaspiração durante ICP primária ocorreu em 30% dos casos e esteve associado a tendência de maior mortalidade. A identificação de preditores clínicos, laboratoriais e angiográficos pode auxiliar no aprimoramento desses dispositivos e em sua técnica, além da escolha de pacientes mais adequados para seu emprego.
Cardiovascular diseases remain the main cause of death in Brazil.1 Acute myocardial infarction (AMI) is the most severe manifestation. Mechanical recanalization treatment is the best choice if this procedure is available in the first 12 hours, thereby decreasing the mortality, when compared with fibrinolytics.2
The presence of an intracoronary thrombus is associated to worse coronary flow and myocardial perfusion, which can be quantified by Thrombolysis in Myocardial Infarction (TIMI)3 classification and by the degree of myocardial blush,4 respectively. Moreover, the clinical outcome is worse in this subgroup, both in the in-hospital phase and in the late phase.5-7 Coronary thrombus is also a predictor of late thrombosis.8
Coronary thrombus is present in most manifestations of acute coronary syndrome, with high prevalence in patients with AMI and ST-segment elevation. To reduce the thrombus burden by pharmacologic means, thrombolytic, antiplatelet, anticoagulant agents, and glycoprotein IIb/IIIa inhibitors are used. Devices for mechanical removal are advantageous versus antithrombotic agents, because these procedures do not increase the risk of bleeding. Aspirators may be electronic or manual, and the latter type is more popular, for its simplicity and costs. Despite the increasing use of pharmacological and mechanical therapy, distal coronary embolization may occur in 6%-15% of cases of AMI,9 causing decreased tissue perfusion, with consequent increase in AMI extent and mortality.7,8
There are several clinical trials evaluating the efficacy of devices for thrombus aspiration in mechanical recanalization procedures for AMI. A meta-analysis of these studies showed an improvement of the surrogate outcomes related to myocardial perfusion. In addition, some studies have suggested improvement of perfusion, myocardial blush, ST-segment resolution, and mortality,10-12 and the effectiveness in the implementation of thrombus aspiration depends of clinical and angiographic factors.13
The aim of this study was to evaluate failure rates of thrombus aspiration, with identification of their predictors in a contemporary cohort of patients undergoing primary percutaneous coronary intervention (PCI), and cardiovascular outcomes according to the result of thrombus aspiration.
METHODSPatientsThis was a prospective cohort study that included all AMI patients undergoing primary PCI in Instituto de Cardiologia da Fundação Universitária de Cardiologia do Rio Grande do Sul (IC/FUC) in the period from December 2009 to December 2011. The project was approved by the ethics committee, and all patients received information about the study and signed an informed consent.
The inclusion criterion was AMI with indication of primary PCI by the attending physician. AMI was defined as a typical chest pain at rest associated with persistent ST-segment elevation of at least 1 mm in two contiguous leads in the frontal plane, or 2 mm in the horizontal plane, or the presence of a typical chest pain at rest in patients with new (or presumably new) left bundle branch block. The exclusion criteria were chest pain lasting > 12 hours, age < 18 years, or no written consent to participate in the study.
Clinical and angiographic characteristicsAll patients were evaluated immediately after the hospital admission, and their clinical, angiographic, and laboratory data were recorded and stored in a dedicated database. The patients received a daily visit from one of the researchers to assess the occurrence of in-hospital outcomes.
The angiographic evaluations were performed in at least two projections by experienced surgeons, using a previously validated digital electronic system (Axiom Artis; Siemens – Munich, Germany) and intracoronary nitroglycerin was routinely administered in doses of 100 to 200 mcg prior to the measurements. The diameter of the target vessel was defined as the average of luminal diameters proximal and distal to the lesion, and the stenosis severity was measured in two orthogonal projections. The length of the lesion was measured “shoulder to shoulder”, and long lesions were considered as singular in the presence of a normal arterial segment < 10 mm between them. The coronary flow was evaluated before and after the procedures, and described according to TIMI criteria.3 The myocardial perfusion was evaluated by myocardial blush, as previously described.4
Primary PCI proceduresThe IC/FUC is a tertiary interventional cardiology center that performs approximately 2,500 coronary interventions per year. Thrombus aspiration was performed with one of three manual suction catheters available: Export (Medtronic Vascular Inc. – Santa Rosa, USA), Diver CE (Invatec – Brescia, Italy), or Pronto (Vascular Solutions – Minneapolis, USA). The aspects related to the procedure, such as access route, administration of glycoprotein IIb/IIIa inhibitors and number of implanted stents, as well as the decision for conducting the thrombus aspiration, were left to the surgeons’ discretion. The thrombus aspiration was performed before the balloon dilation (as described in TAPAS study),10 with several passages, if necessary. The intra-aortic balloon was used only in patients with cardiogenic shock.
The drugs used in the initial care and the indication for primary percutaneous coronary intervention were left to the discretion of the care team, according to the clinical routine. All patients received a loading dose (300 mg) of acetylsalicylic acid (ASA) and clopidogrel (300 to 600 mg). After the coronary angiography, unfractionated heparin was administered at a dose of 60 to 100 U/kg. Primary PCI was performed as described in the guidelines.14
Outcomes and follow-upAll patients were followed during their hospitalization period, and the occurrence of events one month after the index procedure was assessed by telephone contact from one of the researchers. Major adverse cardiovascular events (MACE) were defined as the combination of death from all causes, recurrent AMI, or stroke. Recurrent AMI was defined as a chest pain with new elevation of markers of myocardial injury, associated to a new ST-segment elevation or Q wave. Stroke was defined as a focal neurological deficit, beginning suddenly, and irreversible in the first 24 hours.
Statistical analysisThe results were presented as mean and standard deviation or absolute number and percentage. Variables with asymmetric distribution were presented as median and interquartile range. For comparisons among categorical variables, the chi-squared or Fisher’s exact test were used. For comparisons among continuous variables, Student’s t-test was used. The Mann-Whitney test was used for variables with asymmetric distribution. A two-tailed P-value of < 0.05 was considered significant. Data were collected using an ACCESS database, and the statistical analysis was performed using SPSS version 17.0 for Windows (SPSS Inc. – Chicago, Illinois, United States).
The authors are responsible for the design and conduction of the study, its analysis, writing and editing of the manuscript, and approval of the final content. Absolutely no external funding was used to support this work.
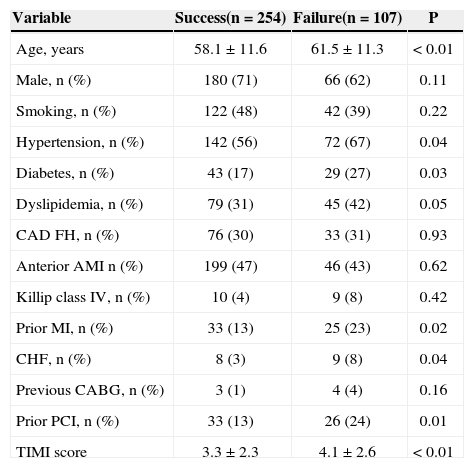
RESULTSDuring the study period, 1,055 patients diagnosed with AMI underwent primary PCI; of these, 986 cases had < 12 hours of symptoms. Manual thrombus aspiration was used in 37% of cases, with 70% success. Thus, the study identified 254 patients with successful thrombus aspiration and 107 patients with failure, whose clinical characteristics are presented in Table 1. Thrombus aspiration failure was associated with older age, systemic hypertension, diabetes mellitus (DM), dyslipidemia, previous AMI, primary PCI, cardiac insufficiency, and TIMI risk score (P < 0.05 for all associations).
Clinical characteristics
| Variable | Success(n = 254) | Failure(n = 107) | P |
|---|---|---|---|
| Age, years | 58.1 ± 11.6 | 61.5 ± 11.3 | < 0.01 |
| Male, n (%) | 180 (71) | 66 (62) | 0.11 |
| Smoking, n (%) | 122 (48) | 42 (39) | 0.22 |
| Hypertension, n (%) | 142 (56) | 72 (67) | 0.04 |
| Diabetes, n (%) | 43 (17) | 29 (27) | 0.03 |
| Dyslipidemia, n (%) | 79 (31) | 45 (42) | 0.05 |
| CAD FH, n (%) | 76 (30) | 33 (31) | 0.93 |
| Anterior AMI n (%) | 199 (47) | 46 (43) | 0.62 |
| Killip class IV, n (%) | 10 (4) | 9 (8) | 0.42 |
| Prior MI, n (%) | 33 (13) | 25 (23) | 0.02 |
| CHF, n (%) | 8 (3) | 9 (8) | 0.04 |
| Previous CABG, n (%) | 3 (1) | 4 (4) | 0.16 |
| Prior PCI, n (%) | 33 (13) | 26 (24) | 0.01 |
| TIMI score | 3.3 ± 2.3 | 4.1 ± 2.6 | < 0.01 |
CAD FH = positive family history of coronary artery disease; AMI = acute myocardial infarction; CHF = congestive heart failure; CABG = myocardial revascularization; PCI = percutaneous coronary intervention; TIMI = Thrombolysis in Myocardial Infarction.
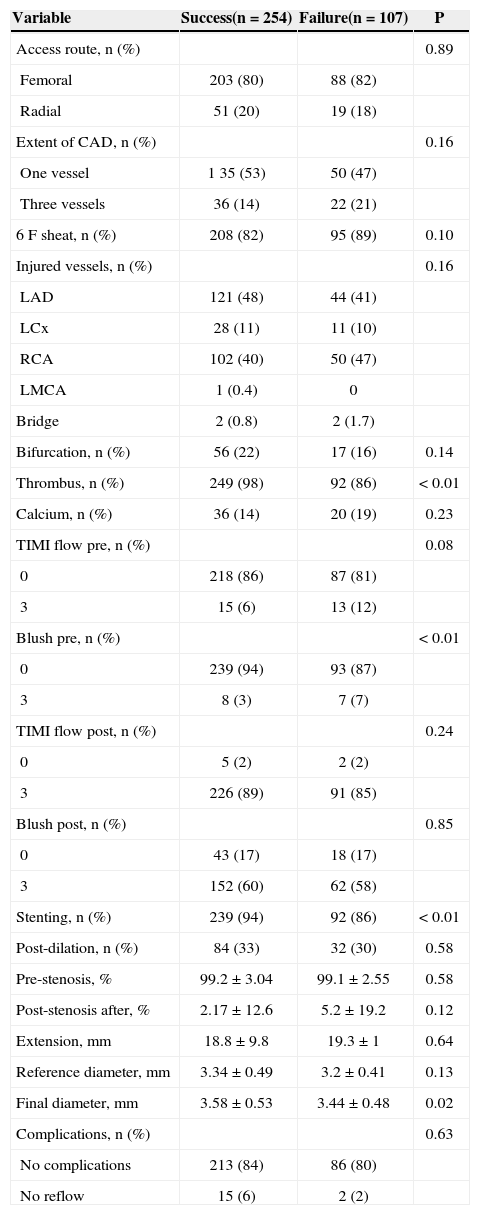
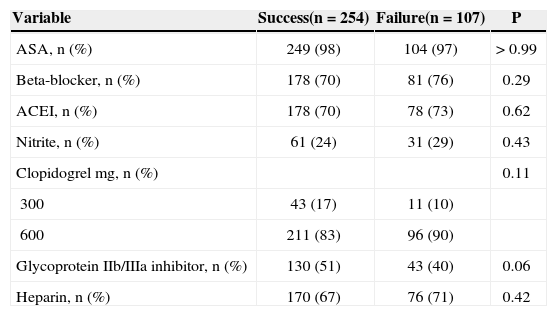
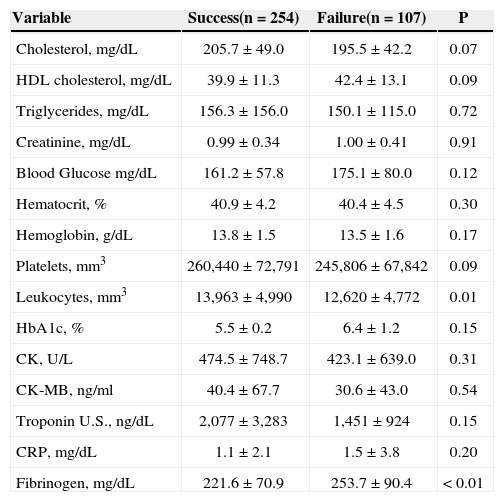
Regarding angiographic and laboratory characteristics, TIMI 3 flow pre-primary PCI (P = 0.08), smaller reference diameter of the target vessel, lower platelet and leukocyte count (P = 0.09), and increased serum fibrinogen were associated with thrombus aspiration failure. Regarding the drugs used in the first 24 hours of care, thrombus aspiration failure presented a tendency for association with decreased use of glycoprotein IIb/IIIa inhibitors (Tables 2-4).
Angiographic and procedural characteristics
| Variable | Success(n = 254) | Failure(n = 107) | P |
|---|---|---|---|
| Access route, n (%) | 0.89 | ||
| Femoral | 203 (80) | 88 (82) | |
| Radial | 51 (20) | 19 (18) | |
| Extent of CAD, n (%) | 0.16 | ||
| One vessel | 1 35 (53) | 50 (47) | |
| Three vessels | 36 (14) | 22 (21) | |
| 6 F sheat, n (%) | 208 (82) | 95 (89) | 0.10 |
| Injured vessels, n (%) | 0.16 | ||
| LAD | 121 (48) | 44 (41) | |
| LCx | 28 (11) | 11 (10) | |
| RCA | 102 (40) | 50 (47) | |
| LMCA | 1 (0.4) | 0 | |
| Bridge | 2 (0.8) | 2 (1.7) | |
| Bifurcation, n (%) | 56 (22) | 17 (16) | 0.14 |
| Thrombus, n (%) | 249 (98) | 92 (86) | < 0.01 |
| Calcium, n (%) | 36 (14) | 20 (19) | 0.23 |
| TIMI flow pre, n (%) | 0.08 | ||
| 0 | 218 (86) | 87 (81) | |
| 3 | 15 (6) | 13 (12) | |
| Blush pre, n (%) | < 0.01 | ||
| 0 | 239 (94) | 93 (87) | |
| 3 | 8 (3) | 7 (7) | |
| TIMI flow post, n (%) | 0.24 | ||
| 0 | 5 (2) | 2 (2) | |
| 3 | 226 (89) | 91 (85) | |
| Blush post, n (%) | 0.85 | ||
| 0 | 43 (17) | 18 (17) | |
| 3 | 152 (60) | 62 (58) | |
| Stenting, n (%) | 239 (94) | 92 (86) | < 0.01 |
| Post-dilation, n (%) | 84 (33) | 32 (30) | 0.58 |
| Pre-stenosis, % | 99.2 ± 3.04 | 99.1 ± 2.55 | 0.58 |
| Post-stenosis after, % | 2.17 ± 12.6 | 5.2 ± 19.2 | 0.12 |
| Extension, mm | 18.8 ± 9.8 | 19.3 ± 1 | 0.64 |
| Reference diameter, mm | 3.34 ± 0.49 | 3.2 ± 0.41 | 0.13 |
| Final diameter, mm | 3.58 ± 0.53 | 3.44 ± 0.48 | 0.02 |
| Complications, n (%) | 0.63 | ||
| No complications | 213 (84) | 86 (80) | |
| No reflow | 15 (6) | 2 (2) |
CAD = coronary artery disease; LADA = left anterior descendent artery; LCx = left circumflex artery; RCA = right coronary artery; LMCA = left main coronary artery; TIMI = Thrombolysis in Myocardial Infarction.
Drugs used in the first 24 hours of admission
| Variable | Success(n = 254) | Failure(n = 107) | P |
|---|---|---|---|
| ASA, n (%) | 249 (98) | 104 (97) | > 0.99 |
| Beta-blocker, n (%) | 178 (70) | 81 (76) | 0.29 |
| ACEI, n (%) | 178 (70) | 78 (73) | 0.62 |
| Nitrite, n (%) | 61 (24) | 31 (29) | 0.43 |
| Clopidogrel mg, n (%) | 0.11 | ||
| 300 | 43 (17) | 11 (10) | |
| 600 | 211 (83) | 96 (90) | |
| Glycoprotein IIb/IIIa inhibitor, n (%) | 130 (51) | 43 (40) | 0.06 |
| Heparin, n (%) | 170 (67) | 76 (71) | 0.42 |
ASA = acetylsalicylic acid; ACEI = angiotensin converting enzyme inhibitors.
Laboratory characteristics
| Variable | Success(n = 254) | Failure(n = 107) | P |
|---|---|---|---|
| Cholesterol, mg/dL | 205.7 ± 49.0 | 195.5 ± 42.2 | 0.07 |
| HDL cholesterol, mg/dL | 39.9 ± 11.3 | 42.4 ± 13.1 | 0.09 |
| Triglycerides, mg/dL | 156.3 ± 156.0 | 150.1 ± 115.0 | 0.72 |
| Creatinine, mg/dL | 0.99 ± 0.34 | 1.00 ± 0.41 | 0.91 |
| Blood Glucose mg/dL | 161.2 ± 57.8 | 175.1 ± 80.0 | 0.12 |
| Hematocrit, % | 40.9 ± 4.2 | 40.4 ± 4.5 | 0.30 |
| Hemoglobin, g/dL | 13.8 ± 1.5 | 13.5 ± 1.6 | 0.17 |
| Platelets, mm3 | 260,440 ± 72,791 | 245,806 ± 67,842 | 0.09 |
| Leukocytes, mm3 | 13,963 ± 4,990 | 12,620 ± 4,772 | 0.01 |
| HbA1c, % | 5.5 ± 0.2 | 6.4 ± 1.2 | 0.15 |
| CK, U/L | 474.5 ± 748.7 | 423.1 ± 639.0 | 0.31 |
| CK-MB, ng/ml | 40.4 ± 67.7 | 30.6 ± 43.0 | 0.54 |
| Troponin U.S., ng/dL | 2,077 ± 3,283 | 1,451 ± 924 | 0.15 |
| CRP, mg/dL | 1.1 ± 2.1 | 1.5 ± 3.8 | 0.20 |
| Fibrinogen, mg/dL | 221.6 ± 70.9 | 253.7 ± 90.4 | < 0.01 |
HDL = high-density lipoprotein; CK = creatinephosphokinase; U.S. = ultrasensitive; CRP = C-reactive protein.
Patients with thrombus aspiration failure showed a higher percentage of MACE, although without statistically significant difference (9.4% vs. 13.2%; P = 0.35) and with a trend to higher mortality (5.9% vs. 11.6%; P = 0.09), as shown in Figure 1.
DISCUSSIONPrevious studies have demonstrated the benefit of thrombus aspiration in patients undergoing primary PCI for AMI.10-12 However, the clinical and angiographic predictors of failure of thrombus aspiration were not reported in these studies.
Vink et al,13 in a single-centre study, demonstrated that calcified lesions, marked tortuosity, and bifurcation lesions were independent predictors of failure of the thrombus aspiration catheter to overcome the target lesion. Age > 60 years and left circumflex artery were independent predictors of failure of thrombus aspiration. This was the first nationwide trial evaluating these clinical and angiographic predictors of failure in thrombus aspiration.
Clinical characteristics of major morbidity, such as presence of hypertension, diabetes, dyslipidemia, and older age, may be related to a greater extent of coronary atherosclerosis, with greater difficulty in the thrombus aspiration. The severity and the extent of the atherosclerotic plate may hinder the progression of the suction catheter.
TIMI 3 pre-coronary flow was also predictor of failure, an association that may have been influenced by bias, thanks to the minor insistence on thrombus aspiration in patients who already had the desired coronary flow, or who exhibited less thrombus burden. A significant difference in final TIMI flow outcomes was not observed between the two groups with and without successful thrombus aspiration.
In cases of AMI, the content of platelets and fibrin in the thrombus is highly dependent on ischemic time. A longer ischemic time is associated with higher content of fibrin and lower content of platelets in the occlusive thrombus.15 It is possible that the group with unsuccessful thrombus aspiration, which showed smaller number of circulating platelets and a higher level of serum fibrinogen, would present longer ischemic times and more organized thrombi, which hampered the aspiration.
This study also demonstrated that there was a tendency for higher mortality and lower use of glycoprotein IIb/IIIa inhibitors in cases of thrombus aspiration failure.
Limitations of the studyThe potential limitations of this study include its observational design, limited to patients who underwent manual thrombus aspiration at the discretion of the surgeon’s analysis. For convenience, this selection possibly excluded cases of greater anatomical complexity, which could provide more information about the predictors of failure. The relatively small sample size should also be highlighted, making it impossible to conduct multivariate analysis in order to identify independent predictors of failure. However, the inclusion of patients for a longer period of time could not represent the contemporary treatment of AMI, of which manual thrombus aspiration is inserted part; rather, the authors opted for the analysis of patients treated over a two-year period. In addition, an analysis of outcome in the medium and long term was not presented; the follow-up of these patients was not greater than 30 days from the index event.
When analyzing the angiographic variables, the presence of a visible thrombus was described, but the classification of the thrombotic burden was not applied, which could help to differentiate the degree of thrombus burden that is associated with failure in the thrombus aspiration technique.8,16
Regarding the comparison of the present results with the literature, the lack of standardisation of the outcomes of thrombus aspiration success and failure suggests that caution should be exercised in the analysis of the studies published to date, and that a standardization of outcomes would assist in future comparison of results.
CONCLUSIONSFailure of thrombus aspiration during primary percutaneous coronary intervention occurred in 30% of cases and was associated with a trend toward higher mortality. The identification of clinical, angiographic, and laboratory predictors can help to improve these devices and the pertinent technique, in addition to selecting the most appropriate patients for their use. The analysis of a larger number of patients with a longer follow-up may be needed, to define the prognostic role of thrombus aspiration failure.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.