Ultrasound-guided thrombin injection (TI) is an option for the treatment of femoral artery pseudoaneurysm. Nevertheless, the result of this technique in patients with acute coronary syndrome (ACS) may be compromised by the use of antithrombotic drugs. In addition, thrombin extravasation to systemic circulation could potentially cause an increase in thromboembolic events.
MethodsPatients admitted with ACS who developed femoral artery pseudoaneurysm after a percutaneous procedure and treated by TI between January 2007 and July 2011 were included. Clinical and laboratory characteristics, treatment results and complications were evaluated.
ResultsWe evaluated 23 patients with mean age of 67.1±14.2years, 60.9% were women, with body mass index of 28.4±4.7kg/m2 and 52.2% were diabetics. At presentation, 87% had non-ST elevation ACS and the remaining had ST elevation myocardial infarction. Of the evaluated patients, 70% were submitted to percutaneous coronary intervention. All patients were receiving aspirin, 78.3% used P2Y12 inhibitors and 39.1% used glycoprotein IIb/IIIa inhibitors. TI was successful in occluding the pseudoaneurysm in 100% of cases (96.7% after the first injection), without distal embolization, local infection or need of surgical correction. There were no cases of myocardial infarction, stroke or unscheduled revascularization. There was one death due to cardiogenic shock 22 days after TI, on the second post-operative day after an elective coronary artery bypass graft surgery.
ConclusionsTreatment of femoral artery pseudoaneurysm by TI is a safe and effective procedure in patients with ACS.
Injeção de Trombina Guiada por Ultrassom noTratamento de Pseudoaneurisma da Artéria Femoral após Procedimento Percutâneo em Pacientes com Síndrome Coronária Aguda
IntroduçãoA injeção de trombina guiada por ultrassom (IT) é uma opção para o tratamento de pseudoaneurisma da artéria femoral. No entanto, o resultado dessa técnica em pacientes com síndrome coronária aguda (SCA) pode ser comprometido pelo uso de medicações antitrombóticas. Também, o extravasamento de trombina para a circulação sistêmica pode causar aumento de eventos tromboembólicos.
MétodosForam selecionados todos os pacientes admitidos com SCA que apresentaram pseudoaneurisma da artéria femoral após procedimento percutâneo, tratados com IT, entre janeiro de 2007 e julho de 2011. Características clínicas e laboratoriais, resultado do tratamento e complicações foram avaliados.
ResultadosAnalisamos 23 pacientes, com idade de 67,1±14,2 anos, 60,9% eram do sexo feminino, com índice de massa corporal de 28,4±4,7kg/m2, e 52,2% eram diabéticos. À apresentação, 87% tinham SCA sem supradesnivelamento do segmento ST e o restante, infarto do miocárdio com supradesnivelamento do segmento ST. Entre os pacientes avaliados, 70% foram submetidos a intervenção coronária percutânea. Todos os pacientes estavam em uso de ácido acetilsalicílico, 78,3% utilizaram inibidores da P2Y12 e 39,1%, inibidores da glicoproteína IIb/IIIa. A IT foi eficaz em ocluir o pseudoaneurisma em 100% dos casos (96,7% após a primeira injeção), sem embolia distal, infecção local ou necessidade de correção cirúrgica em nenhum caso. Não houve infarto, acidente vascular cerebral ou revascularização não-programada. Houve um óbito por choque cardiogênico, 22 dias após a IT, no segundo dia após cirurgia eletiva de revascularização miocárdica.
ConclusõesO tratamento de pseudoaneurisma da artéria femoral com IT é um método seguro e eficaz em pacientes com SCA.
The occurrence of femoral artery pseudoaneurysm after heart catheterisation has an incidence between 0.05% and 2%, increasing to 3% to 8% in therapeutic procedures, due to the use of larger caliber sheaths, as well as more potent antiplatelet and anticoagulant therapies, especially in patients with acute coronary syndrome.1-4
The three main forms of treatment for this type of complication are surgical correction, ultrasound-guided compression, and thrombin injection (TI).
Traditionally, the surgical approach has been considered the reference standard; however, due to its invasive characteristic, it is associated with a higher rate of complications and wound infection, bleeding, and wound dehiscence. Moreover, it is also associated with a longer in-hospital stay and higher costs.5,6
In the early 1990s, ultrasound-guided compression was introduced by Fellmeth et al.7 as one of the first non-invasive methods for pseudoaneurysm correction. Its advantages are the fact that it is noninvasive and low cost, but most of the time, prolonged compression is necessary to achieve success. Many patients do not tolerate it due to the pain, and it is less effective, especially in the context of acute coronary syndromes.8,9
Recently, TI has become the method of choice in the treatment of this complication.10 Several studies, both Brazilian and international, have shown high success rates when using thrombin for femoral artery pseudoaneurysm correction.11-15 However, few data are currently available on the safety and efficacy of local thrombin use in patients with acute coronary syndrome. In this population, it is speculated that the frequent use of anticoagulants and antiplatelet agents could reduce the technique effectiveness. Conversely, any thrombin extravasation into systemic circulation could determine an increase in adverse events in this subgroup of patients at higher atherothrombotic risk.
This study aimed to evaluate the clinical performance of ultrasound-guided TI in patients with acute coronary syndrome who developed femoral artery pseudoaneurysm after percutaneous procedure.
METHODSAll patients with femoral artery pseudoaneurysm after diagnostic or therapeutic heart catheterisation due to acute coronary syndrome (unstable angina, acute coronary syndrome without ST-segment elevation [ACSWSTE], and myocardial infarction with ST-segment elevation [STEMI]), treated with ultrasound-guided TI at the Instituto do Coração of Hospital das Clínicas da Faculdade de Medicina of Universidade de São Paulo (São Paulo, SP, Brazil), from January 2007 to July 2011 were selected through electronic medical record analysis.
The arterial sheath was removed by manual compression for at least 15 minutes, six hours after the administration of unfractionated heparin or ten to 12 hours after the last administration of low molecular-weight heparin. After a local pressure dressing was applied, the patient remained on bed rest, with lower-limb movement restriction for at least six hours after sheath removal.
The pseudoaneurysm diagnosis was attained by clinical examination (presence of painful, pulsatile hematoma, with murmur) and confirmed with Doppler ultrasound. The decision for pseudoaneurysm treatment with thrombin was made at the attending physician’s discretion.
All TI procedures were performed by a team of interventional radiology professionals at this institution. After thrombin administration and confirmation of flow absence, local pressure dressing was applied and the patient remained at rest for 24 hours.
Method effectiveness was assessed by procedural success, defined by flow absence within the pseudoaneurysm after TI.
The presence of complications during hospitalisation was assessed for the safety analysis, and was defined by distal embolism in the treated limb, local infection, need for surgical correction, need for transfusions, acute myocardial infarction, stroke, new unplanned revascularisation after the index procedure, and death.
Data on clinical, laboratory characteristics, medications used, effectiveness, and safety of the procedure were collected in electronic medical records.
RESULTSOf the 31 patients who developed pseudoaneurysm of the femoral artery after catheterisation and/or percutaneous coronary intervention and were treated by ultrasound-guided TI, 23 had a diagnosis of acute coronary syndrome and were considered for the analysis.
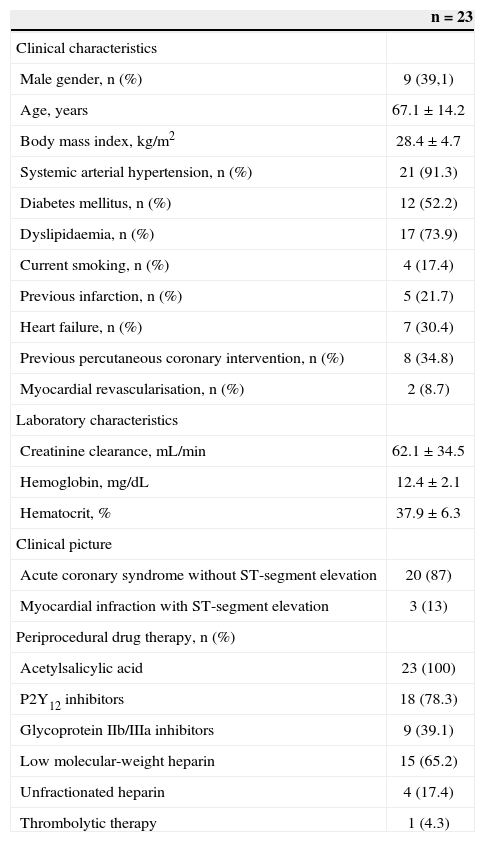
The majority were female (60.9%), aged 67.1±14.2years (32.6years to 92.8years), with body mass index=28.4±4.7kg/m2. Systemic arterial hypertension was present in 91.3% of the patients, diabetes in 52.2%, 17.4% were smokers, and 30.4% had heart failure. A third of the population had undergone previous percutaneous coronary intervention and 8.7% had been submitted to myocardial revascularisation.
Hemoglobin and hematocrit values at the time of the percutaneous procedure were 12.4±2.1mg/dL and 37.9±6.3%, respectively. Mean creatinine clearance, calculated by the Cockroft and Gault formula, was 62.1±34.5mL/min. All patients were receiving acetylsalicylic acid, 78.3% used P2Y12 inhibitors, 39.1% used glycoprotein IIb/IIIa inhibitors, 65.2% used low molecular weight heparin, and 17.4% used unfractionated heparin. Only one patient (4.3%) received thrombolytic therapy (Table 1).
Clinical and laboratory characteristics of patients
| n=23 | |
|---|---|
| Clinical characteristics | |
| Male gender, n (%) | 9 (39,1) |
| Age, years | 67.1±14.2 |
| Body mass index, kg/m2 | 28.4±4.7 |
| Systemic arterial hypertension, n (%) | 21 (91.3) |
| Diabetes mellitus, n (%) | 12 (52.2) |
| Dyslipidaemia, n (%) | 17 (73.9) |
| Current smoking, n (%) | 4 (17.4) |
| Previous infarction, n (%) | 5 (21.7) |
| Heart failure, n (%) | 7 (30.4) |
| Previous percutaneous coronary intervention, n (%) | 8 (34.8) |
| Myocardial revascularisation, n (%) | 2 (8.7) |
| Laboratory characteristics | |
| Creatinine clearance, mL/min | 62.1±34.5 |
| Hemoglobin, mg/dL | 12.4±2.1 |
| Hematocrit, % | 37.9±6.3 |
| Clinical picture | |
| Acute coronary syndrome without ST-segment elevation | 20 (87) |
| Myocardial infraction with ST-segment elevation | 3 (13) |
| Periprocedural drug therapy, n (%) | |
| Acetylsalicylic acid | 23 (100) |
| P2Y12 inhibitors | 18 (78.3) |
| Glycoprotein IIb/IIIa inhibitors | 9 (39.1) |
| Low molecular-weight heparin | 15 (65.2) |
| Unfractionated heparin | 4 (17.4) |
| Thrombolytic therapy | 1 (4.3) |
Regarding the clinical picture, 87% of patients had a diagnosis of unstable angina or ACSWSTE, and the remainder had a diagnosis of STEMI. Diagnostic catheterisation was performed in 30.4% and therapeutic procedure in 69.6% of cases. The 7F sheath was used in 73.9% of procedures and 6F in the remainder.
The mean time from the percutaneous procedure to the pseudoaneurysm diagnosis was 2.7±2.5days (median=2days), and until the ultrasound was performed, 3.2±0.8days. Pseudoaneurysm neck size ranged from 0.2cm to 3.7cm (mean 0.9±1cm), and the largest diameter ranged from 1.3cm to 6cm (mean 2.7±1.8cm); they were multiloculated in 17.4% of patients.
Procedural success was achieved in 96.7% of patients with the first TI and in 100% with the second procedure (performed 48 hours after the first attempt). Most patients (78.3%) were receiving dual antiplatelet therapy and more than half (56.5%) used prophylactic heparin during the procedure to repair the pseudoaneurysm. There were no reports of distal embolic complications, allergic reactions, local infection, need for surgical correction, need for blood products or acute myocardial infarction, stroke, and new revascularisation after the index procedure.
There was one death among the study population due to cardiogenic shock, on the second postoperative day after elective myocardial revascularisation, 22 days after TI.
DISCUSSIONPseudoaneurysm after percutaneous heart procedures is one of the most common vascular complications. The main risk factors for its occurrence are age > 65 years, hypertension, obesity, peripheral arterial disease, large calibre sheaths, and use of antiplatelet and anticoagulant agents.10 In the present sample, the mean age was 67.1years; 91.3% were hypertensive; 73.9% used 7F sheaths, and 69.6% were receiving dual antiplatelet therapy associated with heparin at a therapeutic dose.
Until 1990, the only available treatment for pseudoaneurysm was surgical correction. Although very effective, this procedure can present several complications. San Norberto García et al.16 studied 79 patients who underwent surgery for pseudoaneurysm repair. In this study, 71% of patients had some type of complication within 30 days; need for blood transfusion was the most frequent (53%), followed by infection (19%), and wound dehiscence (12.7%). The mortality related to surgery was 3.8%. The use of antiplatelet or anticoagulant therapy after cardiac catheterisation was an independent risk factor for increased postoperative morbidity.16
In 1991, Fellmeth et al.7 described the treatment of a pseudoaneurysm by ultrasound-guided compression. This method has success rates between 75% and 98% and low complication rates.17,18 However, in most cases, it is a lengthy and painful procedure, and approximately 80% of cases require 60 minutes of compression.8 Moreover, in patients using antiplatelet and anticoagulant agents, pseudoaneurysm recurrence rates can reach up to 30%.19
Ultrasound-guided TI for the treatment of pseudoaneurysm gained prominence after the publications by Liau et al.20 and Kang et al.,21 with success rates of 100% and 95%, respectively. Subsequently, several studies in the literature reported success rates between 93% and 100%.11-15 When compared to ultrasound-guided compression, TI had a higher success rate (100% vs. 87%; P < 0.05) with lower hospital cost.22 Krüger et al.11 also observed that the success rates were higher with simple pseudoaneurysms, when compared to the rates of multiloculated pseudoaneurysms (97% vs. 61%). However, in the present population, in which 17.5% of pseudoaneurysms were multiloculated, the success rate was 100%, regardless of the pseudoaneurysm characteristics.
TI in patients using antiplatelet and anticoagulant agents was also evaluated in some studies. The failure rate is higher in patients with concomitant use of antiplatelet and anticoagulant agents (6.3% vs. 1.3%; P=0.026).12 In a study of 30 patients, of whom 18 were anticoagulated, the success rate was 100%.23 In another study of 274 patients using antiplatelet and/or anticoagulant agents, the success rate with thrombin use was 97%24 In the present study, in which 78.3% of patients used dual antiplatelet therapy and 56.5% used associated prophylactic use of heparin at the time of treatment with thrombin, the success rate was 100%.
However, most studies did not specify the number of patients with acute coronary syndrome submitted to TI for pseudoaneurysm repair. In a Brazilian study of 15 patients treated with TI, all successful procedures, ten had a diagnosis of acute coronary syndrome at admission.14 To date, there have been no studies evaluating the use of TI only in patients with acute coronary syndrome.
Although rare, the procedure is not free of complications. In a multicenter study in Germany with 595 patients, the incidence of thrombus formation in the femoral artery after TI was 0.5%, with deep vein thrombosis reported in 0.5%, and pulmonary thromboembolism in 0.2% of the population.12 Ohlow et al.25 reported a case of distal limb ischemia after TI that progressed, requiring amputation of the affected limb. There were no reports of complications in the patients treated with thrombin at the present service. There was only one death due to cardiogenic shock after elective coronary artery bypass grafting, with no causal association with TI.
The present study demonstrated the effectiveness and safety of ultrasound-guided TI for the treatment of femoral artery pseudoaneurysm in patients with acute coronary syndrome. Success was achieved in 100% of cases, regardless of the pseudoaneurysm complexity and antiplatelet agent use. Additionally, there were no complications related to the use of this therapy.
Study limitationsThis is a pioneering study on the results of TI in the treatment of femoral artery pseudoaneurysm in patients with acute coronary syndrome. However, its observational nature, without a control group for comparison purposes, as well as the small number of patients does not allow the drawing of definitive and comprehensive conclusions on the subject; randomized trials with larger numbers of patients are required.
CONCLUSIONSThe present data suggest that ultrasound-guided TI is a safe and effective method for the treatment of femoral artery pseudoaneurysm occurring after diagnostic or therapeutic heart catheterisation in patients with acute coronary syndrome.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.