Payment mechanisms for health care providers have been used as a strategy to improve management, health indicators, cost containment, equity and efficiency. Among the mechanisms implemented in the past decade is pay-for-performance (P4P). In Chile, it was incorporated since 2003 in primary care in addition to the salary by seniority and training.
ObjectivesTo assess the impact of P4P on the efficiency of primary oral health care providers in Chile.
MethodsWe performed a retrospective cohort study to compare the performance of oral healthcare practices belonging to primary health providers measured by the rate of dental discharge in 6 year-old children between years in which P4P was used and years in which P4P was not used, in the 52 municipalities of the Metropolitan Region of Chile. We also explored whether rurality, and the human development index (HDI) had an association with the efficiency of health care teams. We calculated the rate of discharge per 1000 patients, and its adjusted and unadjusted association with the predictors of interest, using a Random-effects Poisson regression.
ResultsWe found statistically significant differences in the rate of dental discharges when comparing P4P versus no P4P (822.59/1000 and 662.59/1000, respectively, p<0.0001) and high versus low HDI (692.23/1000 and 832.85/1000, respectively, p=0.01). Rurality was not statistically associated with P4P (727.24/1000 in rural and 770.19/1000 in urban municipalities, p=0.553). Unadjusted and adjusted rate ratios were very similar.
ConclusionsP4P financial incentives can improve the performance of primary care dental practices, and seem to be useful interventions to improve the performance of oral health care providers.
Se han venido utilizando mecanismos de pago a los profesionales de la atención sanitaria para mejorar la gestión, los indicadores sanitarios, la contención de costes, la equidad y la eficacia. Entre los mecanismos introducidos en el último decenio se encuentra el pago por desempeño- pay for performance (P4P). En Chile, se lleva incorporando a la atención primaria desde 2003, además del salario por antigüedad y la formación.
ObjetivosEvaluar el impacto del P4P sobre la eficacia de los profesionales de la atención sanitaria oral primaria en Chile.
MétodosRealizamos el estudio comparativo de un grupo, para comparar el desempeño de las prácticas de los cuidados sanitarios orales de los profesionales de la salud primaria, medido mediante el índice de las altas dentales en niños de seis años, entre los años en que se utilizó el P4P y los años en que no, en cincuenta y dos municipios de la región metropolitana de Chile. También exploramos si la ruralidad y el índice de desarrollo humano (IDH) estaban asociados a la eficacia de los equipos de atención sanitaria. Calculamos el índice de altas por 1000 pacientes, y su asociación ajustada y no ajustada a los predictores del interés, utilizando el modelo de regresión de los efectos aleatorios de Poisson.
ResultadosEncontramos diferencias estadísticamente significativas en el índice de altas dentales al comparar P4P frente a no P4P (822,59/1000 y 662,59/1000, respectivamente, p<0,0001), y el elevado frente al bajo IDH (692,23/1000 y 832,85/1000, respectivamente, p=0,01). La ruralidad no estuvo estadísticamente asociada al P4P (727,24/1000 en municipios rurales y 770,19/1000 en municipios urbanos, p=0,553). Los ratios no ajustados y ajustados fueron muy similares.
ConclusionesLas incentivas financieras P4P pueden mejorar el desempeño de las prácticas de atención primaria dental, y parecen resultar unas intervenciones útiles para mejorar el desempeño de los profesionales de la atención sanitaria oral.
Oral health is recognized as an important component of the overall health of individuals and the community. Socio-economic inequality in children's oral health exists within developed countries and between countries with different levels of development.1 Population programs aimed at improving upstream factors are of priority for further improving children's oral health in different populations.1 In this context, dental care has been incorporated into the service portfolio of the health systems of many countries.2 This has resulted in an increase or redistribution of resources allocation in the health field in order to extend the coverage of dental services.3,4
Payment mechanisms for health care providers have been used in different environments as a strategy to improve management, health indicators, cost containment, and efficiency.2 Among the most used to reimburse healthcare providers are fee-for-service (FFS) and capitation. Literature links FFS to higher productivity but also to perverse incentives toward over-treatment.5 The per capita funding mechanism encourages cost containment, coordination between health providers and greater equity in the allocation of resources.6
In the context of the health reform, Chile has implemented and deepened a series of transformations aimed at improving the efficiency and equity in the health system.4 One strategy has been to incorporate new payment mechanisms as a tool to ameliorate the management and health indicators, and to help contain costs and improve efficiency. Since 1990, the capitation mechanism financed Primary Health Care in Chile. It consists in transferring government contributions to the primary care management entities.4
Meanwhile, in the international context, a payment mechanism called “Pay for Performance” (P4P) was introduced in the past decade.7 It is an evolution of fee-for-services8 defined as the transfer of money or material goods conditional on taking a measurable action or achieving a predetermined performance target.9 P4P rewards health care providers in exchange for compliance with generally predefined objectives in terms of quality and efficiency of care.8 Some P4P schemes pay doctors, teams of health professionals or hospitals directly on the basis of multiple indicators. Lazear10 links P4P and productivity. It can also be based on indicators of structure, process and/or outcomes, evaluating providers regarding quality parameters or compared with other providers.
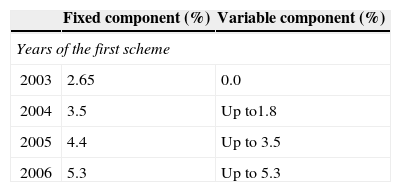
In Chile, since 2003 Primary Health Care (PHC) teams from municipal establishments started receiving additional money as P4P, in addition to the salary according to seniority and training, depending on the collective compliance of performance indicators defined under technical criteria and negotiated in tripartite committees composed of representatives of PHC Municipal Entities administrators, unions representing the workers and the Ministry of Health. According to the degree of compliance of the goals, the P4P implied a percent increase of remuneration that varied between 5–10% at the beginning and 10–21% by 2010 (Table 1).
First and second payment schemes according to collective performance showing incentives based reimbursement given in gradually over a period of four years, according to the following schedule, Chile 2003–2010.
| Fixed component (%) | Variable component (%) | |
|---|---|---|
| Years of the first scheme | ||
| 2003 | 2.65 | 0.0 |
| 2004 | 3.5 | Up to1.8 |
| 2005 | 4.4 | Up to 3.5 |
| 2006 | 5.3 | Up to 5.3 |
| Fixed component (%) | Compliance of 90% or more of the targets | Compliance between 75% and 89% of the targets | |
|---|---|---|---|
| Years of the second scheme | |||
| 2007 | 6.7 | 7.0 | 3.5 |
| 2008 | 8.0 | 8.6 | 4.3 |
| 2009 | 9.2 | 10.2 | 5.1 |
| 2010 | 10.3 | 11.9 | 5.95 |
In the dental care field, the percentage of pregnant women, 6 year-old, and 12 year-old children with dental discharges were established as performance indicators. However the Health Authority decided excluding oral health care for 6 year-old children from the P4P scheme in the years 2007–2008 because these services joined the Explicit Health Guarantees scheme (Garantías explícitas en salud – GES).4 As a consequence, it was informally observed that dental discharges in 6 year-old children markedly decreased. Thereby, oral health care for this population was reinstated to P4P scheme again since 2009 and oral healthcare providers were incentived again for that.
Use of financial incentives to directly reward ‘performance’ and ‘quality’ in primary care is increasing in a number of countries.11 However, there are few studies on incentives based remuneration within dentistry and also there is a lack of studies regarding the effects of a P4P on primary medical and dental care.12,13 Thus this study aimed to describe one of the few experiences of implementing P4P to pay dentists in developing country and to evaluate the association between P4P and the efficiency of Chilean primary care dentists.
Materials and methodsDesign and study populationIn this retrospective cohort study, we reviewed the records of dental discharges over a period of 5 years in 6 year-old children, and compared the rate of discharge between the years in which P4P was implemented against the rate when it was not. The study population consisted of oral healthcare providers belonging to Primary Health Care Providers (Municipalities) from the Metropolitan Region of Santiago de Chile. We included all 52 municipalities of the region (which concentrate over 40% of whole Chilean population), between years 2006 and 2010. To avoid bias, we excluded the first three years of P4P (2003–2005) because although the legal framework established P4P regimen since 2003, this was made effective only since 2006. In addition, it was not until this year that all municipalities across the region had comparable infrastructure and staff conditions. Then 2003–2005 was as a preparatory phase, when details of the forthcoming incentivised targets were in the public domain but were not yet measured.
Data sourceOfficial records from the Oral Health Department of the Health Ministry of Chile grouping dental discharges data of all communes.
OutcomeThe outcome of interest was performance measured as efficiency,14 defined as the rate of discharge of 6 year-old per 1000 patients. Data to inform this outcome was obtained for each municipality, per year.
PredictorsThe main predictor of interest was P4P. In each municipality, there were data regarding three years in which P4P was used (2006, 2009, 2010), and two years in which P4P was not used (2007, 2008). Secondary predictors of interest were the geographic location (whether the municipality was rural or urban, as measured by the percentage of rural population in each municipality), and Human Development Index (HDI) (whether the municipality had a HDI over or under the region median, according to the 2003 measurement).
Statistical analysisIn order to describe the data and the results, we calculated the rate of discharge per 1000 patients. We started by calculating the rate of discharge using the number of patients discharged and the total population per municipality, per year. Then, we pooled these rates together as detailed below. In addition, we calculated the adjusted and unadjusted rate ratio of discharge, according to the predictors of interest.
To explore the association between the rate of discharge and P4P, we used a Random-effects Poisson regression. In this analysis, the fixed effects corresponded to the effects of payment regimen, and a random effect for accounting for the fact that each municipality contributed with data for each of the five years was used.
In the secondary analyses, we explored the association between the rate of discharge and the other predictors of interest. In those analyses, fixed effects for rurality and the HDI below the median were included.
For determining the association between the rate of discharge and each of the predictors, a Wald test was used. The level of significance was set at 0.05.
All analyses were done using the software R (Core Team, R Foundation for Statistical Computing).
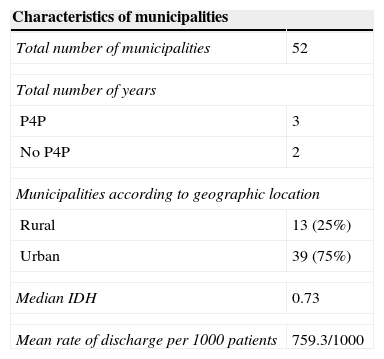
ResultsCharacteristics of the study populationThe total of 52 municipalities had dental discharge data available during the 5 years of this study (Table 2). The overall mean rate of discharge was 759.3 per 1000 patients. This rate was very variable among municipalities. The lowest rate of discharge observed was 116.92/1000, whereas the highest rate of discharge observed was 2467.67/1000 patients.
Main characteristics of municipalities of Chile (2006–2010).
| Characteristics of municipalities | |
|---|---|
| Total number of municipalities | 52 |
| Total number of years | |
| P4P | 3 |
| No P4P | 2 |
| Municipalities according to geographic location | |
| Rural | 13 (25%) |
| Urban | 39 (75%) |
| Median IDH | 0.73 |
| Mean rate of discharge per 1000 patients | 759.3/1000 |
| Mean | SD | |
|---|---|---|
| Mean annual number of 6 year-old children old per municipality: | ||
| Global 2006–2010 | 1321 | 1464 |
| Years with P4P (2006, 2009, 2010) | 1313 | 1391 |
| Years without P4P (2007, 2008) | 1334 | 1576 |
P4P: years when pay-for-performance was used; noP4P: years when pay-for-performance was not used; IDH: human development index; SD: standard deviation.
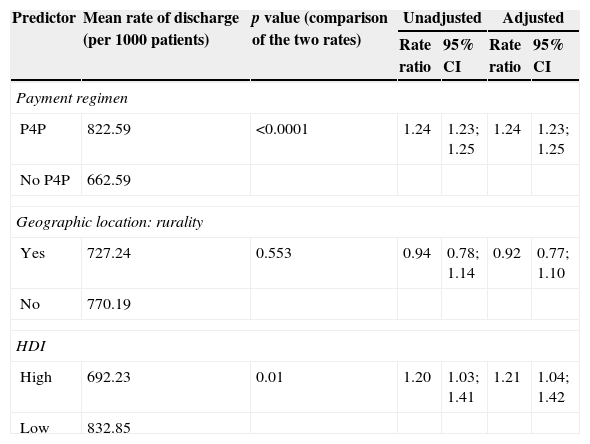
Table 3 shows that the mean rate of discharge was statistically significantly higher when the payment for performance regimen was used, and when the municipality had a HDI index lower than the region median. Even though not statistically significant, the mean rate of discharge was lower in rural wards. However, these results have remarkable implications in Public Health which we will discuss later. Table 3 also shows the association between the rate of discharge and the predictors of interest in terms of the rate ratio, and its 95% confidence interval. The adjusted ratios are very similar to the unadjusted ones. On average, when payment for performance is implemented, there is a 24% increase in the rate of discharge of patients, when compared to the period of time that this payment regimen is not used.
Mean rate and rate ratio of dental discharges according to the predictors of interest. Chile (2006–2010).
| Predictor | Mean rate of discharge (per 1000 patients) | p value (comparison of the two rates) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| Rate ratio | 95% CI | Rate ratio | 95% CI | |||
| Payment regimen | ||||||
| P4P | 822.59 | <0.0001 | 1.24 | 1.23; 1.25 | 1.24 | 1.23; 1.25 |
| No P4P | 662.59 | |||||
| Geographic location: rurality | ||||||
| Yes | 727.24 | 0.553 | 0.94 | 0.78; 1.14 | 0.92 | 0.77; 1.10 |
| No | 770.19 | |||||
| HDI | ||||||
| High | 692.23 | 0.01 | 1.20 | 1.03; 1.41 | 1.21 | 1.04; 1.42 |
| Low | 832.85 | |||||
P4P: years when pay-for-performance was used; no P4P: years when pay-for-performance was not used; IDH: human development index; 95% CI: Confidence interval 95%.
Among our main findings, P4P payment mechanism impacted the rate of dental discharge in 6 year-old Chilean population. We observed that the rate of discharge increased, on average, in 160 per 1000 patients when P4P was used when compared to the years in which it was not used. We also observed that there was an association between the rate of discharge and HDI, i.e. municipalities with lower HDI reached higher rates. The mean rate of discharge was not statistically significantly different although slightly lower in rural municipalities.
We consider that these results are relevant from a public health perspective, and useful to justify the use of incentives. We agree with Voinea-Griffin et al.,13 as P4P could be an strategy to improve efficiency for paying primary care dental practices and performance of dental staff.
In a recent review that aimed to assess the impact of financial systems to reimburse dentist, Johansson et al.,6 show that capitation has a different impact on provided care than FFS: it decreases restorative treatment and caries incidence and also increases preventive care. However, they could not conclude anything regarding productivity. Their study also suggests the need for more research that focus on efficiency.6
Trying to contribute to tackle this shortcoming, our study shows that the method used in Chile to reimburse dentists in capitated environments increased the efficiency compared when paying uniquely salary. Using blended schemes paying salary plus P4P could be a good experience, avoiding the disadvantages of using pure FFS or salary. Besides, we agree with Levy et al.15 who suggested that a blended payment scheme for dentist, e.g., a combined method of P4P and FFS or P4P and salary, could result on larger compensation range and increase the incentive for improved productivity levels.
In the Chilean experience, capitation funding of Primary Health Care and the salaried services foster a preventive approach to care and are particularly suitable where care is directed toward vulnerable groups within the community (municipalities with lower HDI), and also discourage overtreatment.9 Additionally, P4P helps to encourage dentists to deliver patient-centered, adequate, efficient services, and value-based services.16 In fact, Grytten et al.12 found that the transition to an incentive-based remuneration system led to an increase in the number of individuals under supervision without either a fall in quality or a patient selection effect.
Payment mechanisms and pay for performanceIn literature, the term P4P is also used as performance incentives, results-based financing and performance-based financing.9 Currently, P4P has received considerable attention as an innovative model to increase the efficiency and whole performance of health systems, as a payment mechanism that attempts to compensate for the undesirable effects of traditional payment mechanisms.9
In relation to the latter, some comprehensive reviews of the literature about the effects of different types of remuneration concluded that salary tend to be better than fee-for-service (FFS) when considering the global efficiency of a healthcare system. Although our study showed an increase in efficiency when using salary plus P4P compared to only salary, the literature related to the impact of target payment is inconclusive to obtain a clear answer to the question as to whether target payment remuneration provides a method of improving primary health care.6,17,18 Lately an encouraging finding from Baek et al.19 shows that financial incentives (P4P) aligned with clinic productivity/profitability do not to impede high-quality care.19
Regarding payment mechanisms to dentist, one generalized criticism for solo salary systems, is their lack of financial incentives toward productivity.16 On the other hand, FFS, widely used to pay dentist, is done per service provided and is linked to perverse incentives toward over-treatment.13 So, in public health systems where dentists are remunerated on a FFS basis, many concerns arise. On this topic, a system of dental remuneration based on piece work appears increasingly inappropriate in the modern era.16 Then blended payment based on salary plus P4P would help to optimize payment schemes.
Pay for performance and access to oral health care for underprivileged and rural peopleOur results show that the mean rate of discharge was statistically significantly higher when the P4P regimen was used, and when the municipality had a human development index lower than the regional median. Even though not statistically significant, the mean rate of discharge was slightly lower in rural wards compared to urban places. Nonetheless, we consider that these differences are relevant from the public health perspective, and useful when policymakers need to justify the use of incentives, like P4P, to improve efficiency of dental staff.
Municipaities with lower HDI (more deprived places), had higher rates of discharge. There is evidence that people of more vulnerable socioeconomic groups tend to show worse lower rate of visits to the dentist than people with higher socioeconomic level and also have poorer oral health.20 Therefore, if we compare our results with those from studies related to oral health inequalities20 and the preliminary evaluation of the guaranteed oral health delivery for 6 year-old children in Chile,20,21 we can value the importance of continuing with strategies to incentive higher efficiency in dental practices and to improve access to oral health care in the most vulnerable groups of 6 year-old population. Thus we could consider P4P as some of the strategies to address inequalities in access and use of dental services for underprivileged people.1
One of the social determinants of oral health is the place of residence. People who live in rural places have worse oral health status,1,20,21 due to the lack of access to care, having non-fluoridated water, and the lower participation in prevention programs or low exposure to fluorides among other reasons.22
Epidemiological studies demonstrating the marked inequalities in oral health status of the 6 year-old population in Chile,21 reported more decayed teeth in children living in rural areas. This may result in greater workloads to restore oral health of the rural 6 year-old population. Then, it would be, expected to find lower rates of dental discharge in rural places when compared with dentist working in urban areas. However, considering our results and assuming reliability of the dental records, we hypothesize that P4P incentived better engagement and commitment for rural dentists and municipalities in order to improve the access for children and get similar rates to those of urban areas. Furthermore, we should consider that the number of professionals and dental staff size are defined depending on the beneficiary population's size, without necessarily considering the difference between the oral health status of children from urban and rural areas. Therefore, we agree with some authors who emphasize economic incentives as one of the strategies to improve access to health services in rural and most vulnerable areas.23 In Chile, rural municipalities whose population has had major difficulties of geographical access to health centers also have been equipped with mobile dental clinics aimed primarily at meeting the oral health goals related to P4P. This could also explain that no differences were observed according to geographical location.
Some issues related to the implementation of pay for performance and dentistryIncentive schemes should be more carefully designed before implementation.11 Tickle et al.24 reported that the introduction of changes in the incentive structure for dentists in England coincided with large and abrupt changes in the provision of the dental treatments. So, policymakers and stakeholders involved in oral health care provision should consider that changes to financial incentive structures might produce changes in professional behaviors. Also, motives and objectives of professionals do not always agree with public health, then, more thought should be given to policies to change payment structures to mitigate unwanted incentives.
Therefore, we agree with Voinea-Griffin et al.,25 and we think that P4P implementation should be complemented with other indicators of quality performance in dentistry. For example, Grytten et al. propose to use extensive clinical and radiological data on quality before and after providing dental care.12 Other studies also propose that the results on dentists and patients satisfaction and also the potential unintended consequences of incentive schemes should be assessed when P4P is implemented in dentistry,12,14,26 by including a broader range of outcomes.11
Strengths and limitationsAmong the strengths of this study there is the data collection process. Complete data were obtained from a reliable source, i.e. statistical records from Ministry of Health. In addition, it is worth noticing that people from the Metropolitan Región (Santiago de Chile) account for more than 40% of the population of country.
Some municipalities provide dental care based on the number of 6 year-old children studying in the district, many of which, based on geographical capitation funding of primary health care level, are registered in primary health care providers belonging to another municipalities with fewer educational offer. Therefore, those children must attend establishments from other municipalities. Thus the major limitation is that some children were living in a municipality but were treated in another (e.g., they were in the numerator of a municipality and in the denominator of another). This may cause inaccurate evaluation of the association between the characteristics of rurality and vulnerability of the municipalities and the rate of discharges. However there was no way of assessing and estimating this effect because there is no data to quantify this phenomenon in Chile.
There may be problems of dual registration and audit data that overestimate dental discharges in years with P4P. Despite this, we used the best data we could get. The accuracy of the records is an issue that should be evaluated in another study.
Considering that in September of each year targets for the following year are published, the impact of excluding P4P on decreasing of the rate of dental discharges in 2007 may be underestimated due to a cumulative effect from 2006. Similarly, in 2008 the discharge rates might be also underestimated by projections of dental discharges for 2009.
Finally we must consider that the results could also be attributed in part to greater empowerment of the population in the use of guaranteed oral health care.
ConclusionFinancial incentives related to pay for performance can improve the efficiency of primary care dental teams in Chile. This effect was far clearer in municipalities with lower HDI. This payment mechanism seems to be a useful to improve the performance of oral health care providers.
Conflicts of interestM Cornejo belonged to union of primary care workers until September 2010. The other authors declare that they have no conflict of interests.
Contributions of authorshipM Cornejo is responsible for the paper. M Cornejo participated in the study design and fieldwork. All authors have participated in the data analysis and interpretation of the results. Similarly, all signatories have contributed significantly to the preparation and review of successive drafts of the manuscript and to the approval of the final version.
To “Departmento de Salud Bucal of Ministerio de Salud de Chile” for providing in 2011 the data analyzed in this study.