One of the key objectives in the pre-hospital environment is to control and secure the airway. Supraglottic airway laryngopharyngeal tube (SALT) is a basic device designed to ventilate and guide the blind introduction of the endotracheal tube. It has not yet been approved in our environment.
ObjectiveTo determine the blind intubation success rate of non-trained personnel.
ResultsA descriptive trial with 90 participants in a simulated environment with dummies. In 96.7% of the cases, the intubation procedure with the device was perceived as easy. In all, 90% had a successful intubation in the first attempt in 16s, which is a shorter time period as compared to intubation with other devices.
ConclusionSALT could be an effective airway management device for non-trained individuals.
En el ambiente prehospitalario, un objetivo fundamental es el control y aseguramiento de la vía aérea. El tubo laringofaríngeo supraglótico (SALT, por sus siglas en inglés) fue diseñado como dispositivo básico para ventilación y como introductor de TET para intubación a ciegas, aún no aprobado en nuestro medio.
ObjetivoDeterminar la tasa de éxito de intubación a ciegas en personal no entrenado.
ResultadosEstudio descriptivo, con 90 participantes en medio ambiente simulado con maniquíes. Se observó que el grado de dificultad percibida al intubar con el dispositivo fue fácil en el 96,7%. El 90% intubaron de manera exitosa en el primer intento, con un tiempo de intubación en el primer intento de 16s, corto respecto a otros dispositivos.
ConclusiónEl SALT es un dispositivo que podría ser una opción efectiva para asumir la vía aérea en personal no entrenado.
In Colombia, pre-hospital and disaster medicine is an emerging and growing area that has evolved toward adequate patient care outside the hospital environment. This is where emergency care is initially administered that may impact the risk of death or of undesirable sequelae if the patient survives. One of the cornerstones of pre-hospital care is airway control. Direct laryngoscopy (DL) Orotracheal intubation (OTI) is the gold standard for airway management (AW).1
Supraglottic devices are the second best treatment choice when emergency OTI is not available; consequently, the best options for a pre-hospital situation shall be carefully studied.
The SALT (Supraglottic Airway Laryngopharyngeal Tube2 (see Fig. 1) is a new supraglottic device that enables the insertion of a 6.5- to 9.0-mm endotracheal tube (ETT). The device may be left in place for 6h or may be removed upon verification of a correct intubation. On May 2005 the FDA approved the device for human use as a Class I device, but in our country it has not yet been approved.
Considering that the anatomic characteristics of the airway dimensions differ depending on the geographical population, the intended research is aimed initially at determining blind intubation success rate by unskilled personnel in a simulated environment.
MethodologyThis was a descriptive simulation trial using dummies, at the Universidad de Antioquia simulation center. The participants were medical students, 18 years old and above, first aid personnel from the army who attended training courses and pre-hospital care (PHC) at the simulation center. The participants with previous advanced airway management training and instructors of cardiopulmonary resuscitation were excluded. The sample size was 90 participants and the dummies used were: Laerdal: Resusci-Anne. A standard lubricated 7.5mm was used.
The participants received a 20-min training on the proper use of the device at the simulation room. Then each participant intubated the dummy. The time elapsed from the moment the device was delivered and the ETT insertion at every attempt was recorded in seconds. The stop watch began at zero seconds and the final time was the ETT insertion time.
Following each attempt to position the SALT and potential intubation, the researcher checked for proper intubation using direct laryngoscopy. In case of failed intubation defined as the malpositioning of ETT in the airway (trachea), the device was given back to the participant for a second attempt. Each participant was allowed a maximum of three attempts.
The ethics committee approved the research and each participant had to sign an informed consent prior to admission to the trial.
The variables measured included ETT insertion, successful intubation in three attempts, level of difficulty perceived for the intubation using a Linkert-type scale and the number of attempts required for a successful intubation. The SPSS version 20 statistical software was used for the analysis of the results.
ResultsA total of 90 participants were recruited as per the protocol. In the course of the trial, inexperienced staff from different areas were included (Pre-Hospital Care, military personnel, medical students). The age range of the participants was 19–51 years distributed as follows: 10–25 years, 58.9%, and more than 25 years, 41.1%.
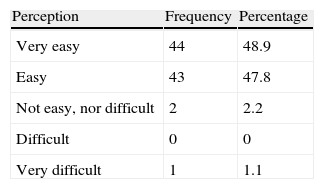
Of the participants 96.7% considered that using SALT was easy (see Table 1) and 90% accomplished a successful intubation at the first attempt (see Table 2).
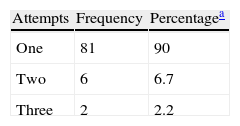
Number of attempts needed for a successful intubation.
| Attempts | Frequency | Percentagea |
| One | 81 | 90 |
| Two | 6 | 6.7 |
| Three | 2 | 2.2 |
Only one failed intubation event was recorded – 1.1% of the participants.
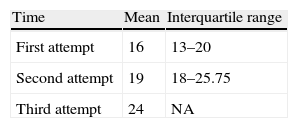
The mean time required for blind intubation during the first attempt was 16s (inter-quartile range 13–20s) (see Table 3).
Average Time in seconds to a successful intubation.
| Time | Mean | Interquartile range |
| First attempt | 16 | 13–20 |
| Second attempt | 19 | 18–25.75 |
| Third attempt | 24 | NA |
NA: not applicable.
Source: Tables 1, 2 and 3: Data collection and analysis during the course of the research: Evaluating SALT as a practical device for blind endotracheal intubation by non-experienced personnel in dummies.
Optimum airway (AW) and ventilation management of critical patients is a cornerstone for the patient's survival, evolution and prognosis, particularly in a pre-hospital setting and in the ER.3 Direct laryngoscopy OTI requires training of at least 50 successful attempts to achieve more than 90% success rate, in addition to regular practice to keep up that level of performance.4
It has been shown that OTI in the pre-hospital setting is possible when experienced personnel control the AW; there are several factors affecting the outcome including blood, vomiting and secretions, as well as anatomical variations, the patient's position, and environmental factors.5,6
The difficulty lies in the additional practice required to maintain the orotracheal intubation skills that sometimes may not be enough7 and may require further emphasis on the proper use of the Bag Mask Valve (BMV) or adequate handling of the supraglottic devices (SD).
The use of the BMV in a pre-hospital setting allows for effective ventilation with satisfactory neurological outcomes in patients with return or spontaneous circulation (ROSC) and may even be better than an advanced airway attempt;8 however, keeping it for long periods of time may prove to be difficult, particularly when the patient is transferred in an ambulance; a safe AW should be secured for transfer.9
Supraglottic devices for AW management are the second treatment option to secure the airway if intubation fails; however, these devices do not completely isolate the airway from the GI tract and there is a risk of bronchoaspiration, particularly in emergency situations when the assumption is that the patient has a full stomach.10
Supraglottic devices to secure a safe advanced airway could be the option as a pre-hospital approach for a considerable number of patients.11 Thus we researched SALT based on its characteristics and advantages as compared to other devices (easy-to-use design, minimum learning curve for blind intubation, suggested for difficult settings, use of conventional ETTs, and lower cost versus that of the devices available in the market (25 US$ in contrast to US$250 for a regular multiple use laryngeal mask (ILMA) and $70 for the single use and disposable mask).
The first consideration is SALT's effectiveness for securing an advanced airway with a high percentage of successful procedures in the first attempt, in contrast with the previous SALT trial that resulted in a first attempt success rate of 66.4%.4 This is a critical finding considering that the airway has to be secured in patients undergoing resuscitation or ROSC, who will have a long transfer time or when BMV ventilation is difficult, to contribute to a better outcome, both in terms of morbidity and mortality.
The time to introduction and intubation is short, considering that non-trained personnel may take 69s using the ILMA, (CI 95% 51–88) in their first attempt, without OTI,10 which is longer than with SALT and fail to secure an advance AW. This time may be influenced by the easy maneuver with SALT or by the lower risk perception when intubating a dummy.
The training time needed for the device was short, suggesting the SALT's learning curve is short, in addition to the fact that the introduction and intubation were considered easy, hence facilitating the training process of the Pre-Hospital Care staff in the proper use of the device.
The heterogeneity of the population associated with the percentage of intubations, may indicate that even people with minimal health care knowledge may be able to properly use the device.
The major limitation of the trial is the use of dummies; however, this allows for a strict standardization of the trial conditions; nevertheless, the data should be confirmed in a real life scenario.10 Comparisons have been made against the results from using supraglottic devices in dummies in a clinical setting, and the results suggest that the use of dummies is comparable.12
It should be noted that this device should be tested in humans (initially in cadavers) against other SDs because the anatomic characteristics of the larynx vary from patient to patient. The SALT was evaluated in cadavers in a Pre-Hospital setting with a 91% success rate (confidence interval CI 95%: 71–99) with a percentage intubation of 59% (CI 95%: 36–79) at first attempt,13 which was low versus our trial results. However, the same cadaver was used several times and this predisposes to a margin of error since the tissues must be intact to verify the effectiveness of the device.
ConclusionThe SALT is a simple and effective device that results in a high rate of successful first attempt blind intubation. The instructions for use of the SALT are easy to follow by non-skilled personnel and the mean time to complete the procedure is shorter than with other supraglottic devices.
Additional trials shall be conducted in our environment in humans to verify the real life effectiveness of the device, since the characteristics of the larynx may change from patient to patient. SALT's effectiveness has been demonstrated only in a simulated environment.
SALT may become a device for AW management by unskilled personnel or a second choice device for difficult airways.
FundingAuthors’ resources.
Conflict of interestsNone.
Please cite this article as: Uribe-Valencia HC, Correa IDA, Reyes JLA, Venue T. Evaluación del tubo laringofaríngeo supraglótico como un dispositivo útil para intubación endotraqueal a ciegas, en personal no experimentado, utilizando maniquíes. Rev Colomb Anestesiol. 2014;42:172–175.