Tracheostomy is a procedure indicated for patients with extended mechanical ventilation.
ObjectiveThe objective of the study was to learn about the technical characteristics, the appropriate timing for the procedure and its evolution.
Material and methodObservational, retrospective study of ICU admitted patients during 2012, with elective tracheostomy. The demographic variables, the Apache II, the pathologies, the number of days in MV, length of stay and mortality were analyzed, both globally and by groups, depending on the early or late use of the technique. The study was approved by the Ethics Committee for Clinical Research of the institution, in accordance with the institutional bioethical principles.
ResultsThe mean age in the sample with 42 patients was 61.36, and the mean Apache II was 18. The most frequent pathology was neurological. The approach was percutaneous in 71.5%, with minor complications in 20% of the cases. In the early tracheostomy group, the number of days in MV and the length of stay were both considerably shorter.
ConclusionsElective tracheostomy is a commonly used technique in the ICU and the procedure is performed according to the protocol. The percutaneous approach is the most frequently used, with few complications. In neurological critical patients with extended weaning, an early approach reduces the number of days with ventilation and the length of stay, with no positive impact on mortality.
La traqueostomía es un procedimiento indicado en los pacientes con ventilación mecánica prolongada.
ObjetivoEl objetivo del estudio fue conocer sus características, técnica, momento adecuado de realización y evolución.
Material y métodoEstudio observacional retrospectivo, de pacientes ingresados en UCI durante 2012, con traqueostomía electiva. Se analizaron variables demográficas, escala Apache II, patologías, días de VM, estancia y mortalidad; de forma global, y por grupos según técnica precoz o tardía. El estudio fue aprobado por el Comité Ético de Investigación Clínica del centro, cumpliendo con los principios bioéticos del mismo.
ResultadosEn la muestra de 42 pacientes la edad media fue 61.36, con mediana de Apache II de 18. La patología más frecuente fueron los pacientes neurológicos, se realizó la forma percutánea en el 71.5%, con complicaciones menores del 20%. En el grupo de traqueostomía precoz se observó menor número de días de VM y estancia de forma significativa.
ConclusionesLa traqueostomía electiva es una técnica frecuente en UCI, realizado el procedimiento según protocolo; la modalidad percutánea es la más empleada, con escasas complicaciones. En los pacientes neurocríticos y con destete prolongado la técnica precoz reduce los días de ventilación y estancia, sin beneficio en la mortalidad.
Tracheostomy (TC) procedures in patients requiring extended mechanical ventilation are frequently performed in the intensive care unit (ICU). There is an ongoing debate with regards to the technique, the timing of the procedure, the impact of duration of mechanical ventilation1 (MV), length of stay, and mortality.2,3 The best time to do the TC is still being debated.4
The contradictory results in the literature, and the lack of evidence in favor of early tracheostomy warrant further research to contribute with additional information about the procedure. The objective of the study was to describe the characteristics of patients with indication for TC, comparing early versus late groups.
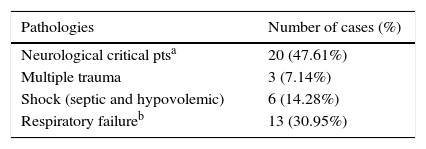
Material and methodsAn observational, descriptive study was performed in a cohort of patients admitted to the ICU with indication for tracheostomy during 2012. The patients undergoing tracheostomy were selected analyzing the demographics, the underlying pathologies (classified as critical neurological patients, multiple trauma patients, state of shock and respiratory failure), severity scale at the time of admission (Apache II), type of technique (percutaneous or surgical), complications (immediate and late), duration of MV, length of stay in the ICU, and survival. Patients with a history of laryngectomy, emergency procedure due to airway obstruction, or limitations for life support therapy were excluded.
Following the indication for TC approved by consensus during a clinical session, the elective procedure was performed as per the current protocol. The study was approved according to the rules of the Ethics Committee on Clinical Research. The technique was decided based on the cervical anatomy and the clinical situation. The percutaneous approach was safe and avoided transferring the patient. The surgical approach is the first line option in the presence of cervical pathology or anatomical alterations. This procedure was performed at the ICU unit or by ENT for more complex cases.
According to the model, the patients were classified as early and late TC, from day 14. The recent evidence5 recommends waiting 10 days to confirm the need for MV before indicating the procedure.
A prospective review of the medical records was performed, collecting variables and developing a database for further analysis. The categorical variables are expressed as percentages and frequency distributions, while the quantitative variables are expressed as means (95% CI) or medians (IQR). The contrasting hypotheses tests used for the quantitative variables were the t-Student test for the comparison of parametric measures and Mann–Whitney U test for the non-parametric. The chi-square test was used for the qualitative variables.
ResultsThe mean age of the sample (n=42) was 61.36 years, with 69% males. The mean Apache II was 18, IQR [13–20]. The most frequent pathology was neurological critical patients (Table 1). The percutaneous approach was used in 71.5% of the cases with 19% immediate complications reported and 16.7% late complications. The survival was 64.3%.
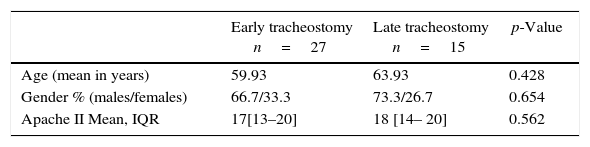
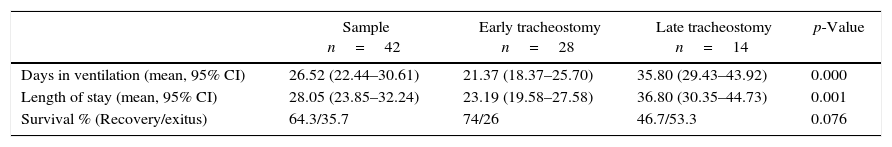
The mean number of days in MV until the TC was 14 IQR [9–17]; the mean number of total days in MV was 26.52 with 95% CI (22.44–30.61); and the mean length of stay was 28.05 with 95% CI (23.85–32.24). The cases were classified into groups: early TC performed before or on day 14 of MV (n=27, 64.3% of the sample); and late TC after day 14 of MV, (n=15, 35.7% of the sample). Both groups were comparable in terms of age, gender, and Apache II severity scale (Table 2). For the variables of total days in MV and length of stay, significant differences were identified, with higher mean values among the late TC group. There was no significant association between the TC time and survival (Table 3).
Group characteristics of groups in terms of the timing of the procedure: early (up to 14 days in MV), late (after 14 days in MV).
| Early tracheostomy n=27 | Late tracheostomy n=15 | p-Value | |
|---|---|---|---|
| Age (mean in years) | 59.93 | 63.93 | 0.428 |
| Gender % (males/females) | 66.7/33.3 | 73.3/26.7 | 0.654 |
| Apache II Mean, IQR | 17[13–20] | 18 [14– 20] | 0.562 |
MV, mechanical ventilation.
IQR, inter quartile range, percentile 25–percentile 75.
Source: authors.
Comparison of number of days in mechanical ventilation, length of stay, and survival Early technique (up to 14 days in MV), late (after 14 days in MV).
| Sample n=42 | Early tracheostomy n=28 | Late tracheostomy n=14 | p-Value | |
|---|---|---|---|---|
| Days in ventilation (mean, 95% CI) | 26.52 (22.44–30.61) | 21.37 (18.37–25.70) | 35.80 (29.43–43.92) | 0.000 |
| Length of stay (mean, 95% CI) | 28.05 (23.85–32.24) | 23.19 (19.58–27.58) | 36.80 (30.35–44.73) | 0.001 |
| Survival % (Recovery/exitus) | 64.3/35.7 | 74/26 | 46.7/53.3 | 0.076 |
MV, mechanical ventilation.
Source: authors.
TC is a technique frequently indicated in patients requiring extended MV. In our study the mean age was 61 years, with predominantly male patients. The most frequently used approach was percutaneous with a rate of complications of less than 20%, being a safe technique. The best timing to do the procedure is not yet defined. The median time in MV until the procedure was performed was 14 days. The patients in the early TC group has less days in MV and shorter length of stay as compared against the late TC group. These results are comparable to those in previous meta-analyses.6 By contrast, there were no differences in terms of mortality, in accordance with recent publications.7
Further research shall consider the heterogeneity of the patients included depending on the pathology. In neurological critical patients and/or patients with a high probability of extended MV, the early TC reduces the number of days in MV and the length of stay in the ICU,8 with no impact on mortality.9
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FinancingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Barrio ME, Berrazueta-S. de Vega A, Romero-Pellejero J, Fernández-Ratero JA, del Valle-Ortiz M, Armesto-Formoso D. Pacientes con indicación de traqueostomía en una cohorte de cuidados intensivos. Rev Colomb Anestesiol. 2016;44:278–281.