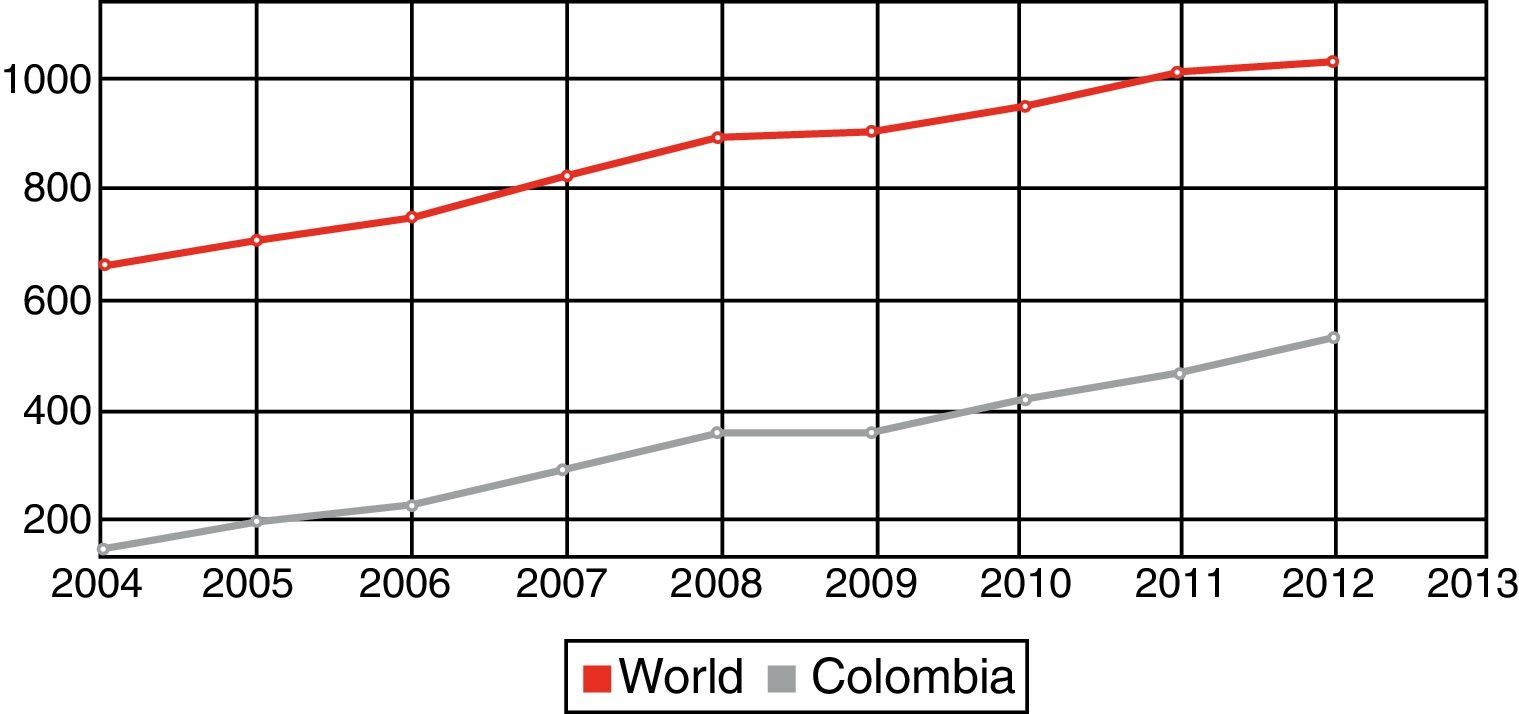
Control of health care expenditure remains one of the most significant challenges many countries in the world are currently facing given its potential to disrupt the provision of basic health care services within the next decade. As seen in this graphic from the World Bank (Fig. 1), health expenditure per capita in Colombia has followed the same upward trend seen in most developed and developing countries.1
Since cardiovascular disease remains the leading cause of morbidity and mortality, any large scale interventions will have a significant impact in healthcare budgets.
Cost-effectiveness analysis is a tool which provides different costs associated with health outcomes, compares costs of treatment alternatives and assesses which alternative is worth the cost. This information will provide policy makers elements for allocation decisions. The goal is to get the most out of the existing and projected financial resources.
Quality-adjusted life year, or QALY, reflects how many years of high-quality life a patient gains with a particular intervention. Another parameter used to measure value is the cost-effectiveness ratio. It is the price of buying more healthy years with a new treatment compared with the standard treatment, and whether it is a good value.
The World Health Organization has a rule of thumb: Three times per-person income per quality-adjusted life year gained is a cost-effective intervention.
To make further progress in health, meet new challenges, and redress inequities, resources must be deployed effectively. This requires knowledge about which interventions actually work, information about how much they cost, and experience with their implementation and delivery
In this issue of the Revista Colombiana de Cardiología, M. Ceballos-González2 published an elegant cost effectiveness analysis of drug eluting stents (DES) compared to bare metal stents in patients with ST elevation myocardial infarction (STEMI) in Colombia. His analyses included actual costs, projected costs, probability determinations as well as many others calculations which are rather difficult to translate into clinical language. The main conclusion however, was that Sirolimus-eluting stents are not cost effective for patients with ST elevation myocardial infarction in Colombia.
It is important to remember that this analysis is circumscribed to STEMI patients and does not apply to elective or semi elective interventions. Prevalence has a large effect on the cost-effectiveness analysis. For example, screening and treatment for helicobacter, a bacterial risk factor for stomach cancer, is not cost-effective in the United States, but it is cost-effective in Colombia, because the prevalence of stomach cancer is higher in this country and many of the costs of treatment are lower. Thus, it is important not to necessarily extrapolate the results of STEMI to elective or semi-elective stenting as the prevalence and rate of complications are different. Additionally, patient and lesion characteristics may be more relevant when determining the choice of stents, bare vs drug eluting, than the actual consideration of coronary artery disease prevalence.
Price evolution may also make the difference between cost effective and not cost effective. A study published by Barone-Rochette et al.3 found that the sirolimus stents were not cost effective in 2008 but became cost effective by 2012 after its price was reduced.
As a health policy, the recommendation to avoid DES in the setting of STEMI in Colombia may seem reasonable from the economic standpoint. It is however important to remember that policies are guidelines and do not necessarily apply to every case scenario. When making the decision to use drug-eluting vs bare-metal stents is important to make individual patient considerations such as patient's compliance, type of lesion, concurrent illnesses that may increase the risk of restenosis (diabetics), etc. In this study, late complications outweighed the initial benefit of DES. Whether late complications were due to lack of compliance with anti platelet therapy for instance may not be excluded.
This study may help create the momentum toward delineating health policies around the management of STEMIs which will help standardize treatments across regions and centers. There are wide variations in how often doctors order tests, prescribe medicines, do procedures or surgeries—not just in different parts of the country, but in hospitals that are right next to each other. One place may do more procedures of a particular kind than the place next door.
If we could make the high-spending/poor-performance hospitals or regions or service areas more like the lower-spending/better-outcome ones, the health care system could save money and improve health at the same time.
If there is a lesson to be learned from the US health care system is that elevated health care costs are not sustainable in the long run and finding the balance between costs and outcomes will benefit both patients and providers.
This article is available in Spanish at www.elsevier.es/revcolcar