The treatment of a coronary chronic total occlusion is one of the main challenges of interventionist cardiology. Based on angiographs, the prevalence is 15 to 20%. Revascularization is indicated less frequently due to a greater failure rate, greater exposure to radiation, high cost, and a greater frequency of complications. Therefore, only 35% of coronary chronic total occlusions are reportedly referred for revascularization, in which cases success is close to 80%.
Uncertainties remain regarding the benefits of treatment, according to information obtained from observational studies1. Patients are referred due to their symptoms, or because of significant ischemia on non-invasive tests. The proportion of asymptomatic individuals is close to 10%. Finding a chronic total occlusion is one of the main reasons for referring a patient to coronary surgery.
FundamentalsThe indication for revascularization of a coronary chronic total occlusion is based on the severity of the symptoms, the ischemic territory, and ventricular viability and function2. The operator's experience versus the angiographic complexity of the occlusion (objectifiable using clinical-angiographic scores such as the J-CTO score), should be analyzed3. Treatment is begun with optimal medical management and risk stratification. The greater the risk (e.g. a greater area of ischemia), the greater the benefit of angioplasty, and the more appropriate its indication.
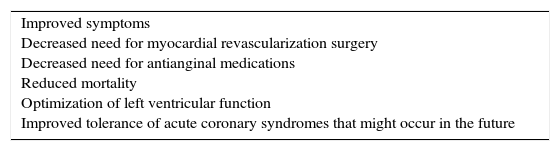
Table 1 shows the benefits of percutaneous intervention.
Potential benefits of revascularization of coronary chronic total occlusions3
| Improved symptoms Decreased need for myocardial revascularization surgery Decreased need for antianginal medications Reduced mortality Optimization of left ventricular function Improved tolerance of acute coronary syndromes that might occur in the future |
In Joyal's meta-analysis4 of 13 observational studies, mortality at six years was lower in the group with
successful rechanneling of the coronary chronic total occlusion, compared with the group that was not rechanneled (14.3% vs. 17.5%; OR 0,56).
Approach to the patient with coronary chronic total occlusionWhen coronary chronic total occlusion is found, the following factors are considered relevant.
Presence and degree of ischemiaRevascularization will be appropriate in patients with significant ischemia, even if they are asymptomatic, and/or have regional dysfunction of the left ventricle. Most cases of coronary chronic total occlusion will have significant ischemia, and it has been shown that angioplasty of a coronary chronic total occlusion significantly reduces ischemia, with a cut-off point of 12.5% ischemic burden as a predictor of benefit, and, lacking this, in ischemias lower than 6.25%5.
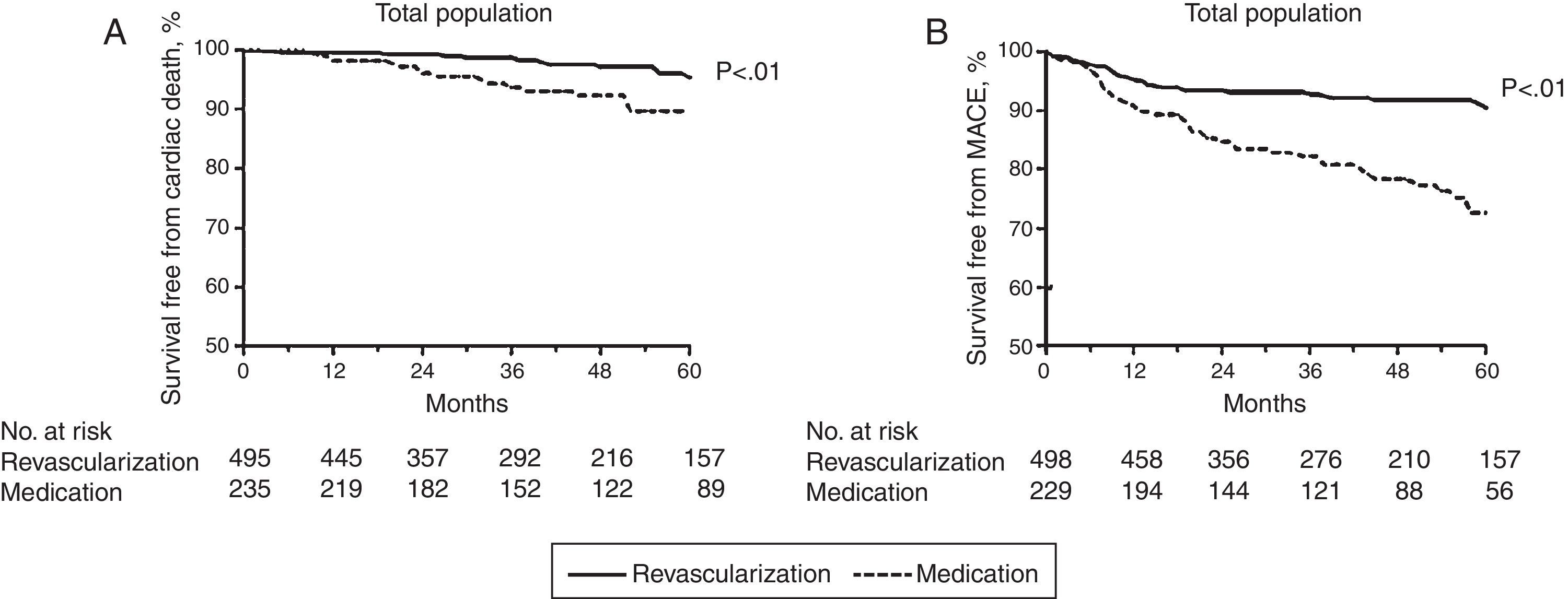
Typically, patients with coronary chronic total occlusion have collaterals to the distal segment, but these do not provide sufficient flow to the myocardium. Sachdeva et al., using FFR, showed that each coronary chronic total occlusion was hemodynamically significant, even with important collaterals6. A recent study comparing medical management of coronary chronic total occlusion with collaterals (Rentrop III) vs. percutaneous treatment, showed a lower incidence of cardiac death7 (HR:0.29; p<0.01) and MACE (HR:0.32) in the revascularization group (Fig. 1).
Presence of symptomsSuccessful revascularization of a coronary chronic total occlusion is associated with an improvement in symptoms. Benefits include decreased limitation of physical activity, fewer episodes of angina, and a better quality of life. A meta-analysis showed that successful rechanneling of a coronary chronic total occlusion produced greater symptom relief in long-term follow up, compared with the group where vessel rechanneling was unsuccessful4. In the FACTOR study, Grantham reported significant improvement at one month using the Seattle Angina Questionnaire in treated symptomatic patients8.
Possibility of successThe success rate in coronary chronic total occlusion ranged from 50% to 75%. Advances in techniques, new dedicated guide wires, microcatheters and greater operator experience have increased the success rate. The Euro CTO Club reports 83% success, and in Japan and groups in the USA with hybrid confrontation, rates close to 90% are reported. Against these figures, however, there is a greater rate of complications, especially coronary perforation (3%), periprocedural infarction (2.4%) and contrast-induced nephropathy (3%). Mortality is between 0.2 and 1.3%. The operator's learning curve and experience is a factor that should be considered.
Coronary chronic total occlusion in the presence of multivessel diseaseCoronary chronic total occlusion is common in multivessel disease and determines the option of revascularization. In the Canadian Registry of coronary chronic occlusions9, multivessel disease was present in ¾ of patients, a finding associated with greater referral for surgery.
Furthermore, if percutaneous treatment is selected in this context and there is a chronic total occlusion, failed revascularization is frequent. There is current evidence to show that incomplete revascularization in multivessel disease treatment is a determining factor in a worse prognosis.
Viability and ventricular dysfunctionPatients with multivessel disease frequently present a history of infarction and left ventricular dysfunction with potentially recoverable territory. The diagnostic tools for seeking viability are crucial for evaluating the potential benefit of revascularization. In our experience, nuclear magnetic resonance is the method of choice since in its delayed contrast analysis the extent of necrosis in the myocardial wall thickness can be determined. Necrosis of less than 75% of the thickness could be benefited by a percutaneous revascularization, with the beneficial effect increasing as the percentage of necrosis decreases. A meta-analysis published in 2015 by Hoebers10 showed that following percutaneous rechanneling of a coronary chronic total increased 4.4% (95% CI; 3.52-5.35, p<0.01) compared to baseline. In addition, a decrease in end diastolic volume was reported.
Revascularization of a coronary chronic total occlusion in post acute myocardial infarction patientsAmong acute myocardial infarction patients, approximately 40 to 60% have multivessel disease, and it is estimated that close to 10% have a coronary chronic total occlusion in a vessel unrelated to the infarction. Multivessel disease with a coronary chronic total occlusion is an independent predictor of mortality during infarction. The COREA-AMI study notes that patients who underwent a successful percutaneous rechanneling of the coronary chronic total occlusion (not responsible for the infarct) had a lower global mortality (16.7 vs. 32.3%) and MACE (21.9 vs.55.2%) compared with the non-treated group11, which suggests the relevance of the treatment in this context.
ConclusionsPercutaneous interventionism of the coronary chronic total occlusion may provide significant benefits for the patient when it is clinically indicated and the procedure is appropriate. Patients should be treated according to their symptoms or evidence of ischemia, in viable territory, and not according to the operator's skills (risk of inappropriate angioplasty). The myocardium irrigated by a coronary chronic total occlusion will always be an ischemic zone, even in the presence of good collateral circulation. Extensive ischemia, coronary chronic total occlusion in the presence of multivessel disease, or acute myocardial infarction, is associated with a worse prognosis. Successful treatment is associated with fewer symptoms, better quality of life and optimization of ventricular function indices. Benefits have been reported with regard to cardiovascular mortality, although there are no definitive data, as yet12. Successful complete percutaneous revascularization should be the goal, a factor which should increase the number of treated coronary chronic total occlusion patients. The foregoing supports the idea of developing coronary chronic total occlusion programs with dedicated operators having more than 50 coronary chronic total occlusion procedures/year, as well as referral networks, in order to optimize patient selection, maximize success, and decrease possible complications.