percutaneous transmitral commissurotomy has become an ideal treatment option for mitral stenosis due to its less adverse events and more favorable outcomes. Patients improve symptomatically after percutaneous transmitral commissurotomy but we have minimal available data about the quality of life after percutaneous transmitral commissurotomy.
Objectiveto assess the quality of life after percutaneous transmitral commissurotomy through WHOQol scoring covering different aspects of life, to determine its correlation with a net gain in mitral valve area (MVA) and to ascertain its association with gender.
Methodsit was a prospective cohort study carried out for a period of 15 months. A total of 100 patients with mitral stenosis who had successful percutaneous transmitral commissurotomy done were enrolled in the study. Among the total included, 4 patients were lost to follow up and data were collected from 96 patients. Quality of life was assessed before the procedure, at 1 month and 3 months follow up after percutaneous transmitral commissurotomy using WHOQol scoring questionnaire.
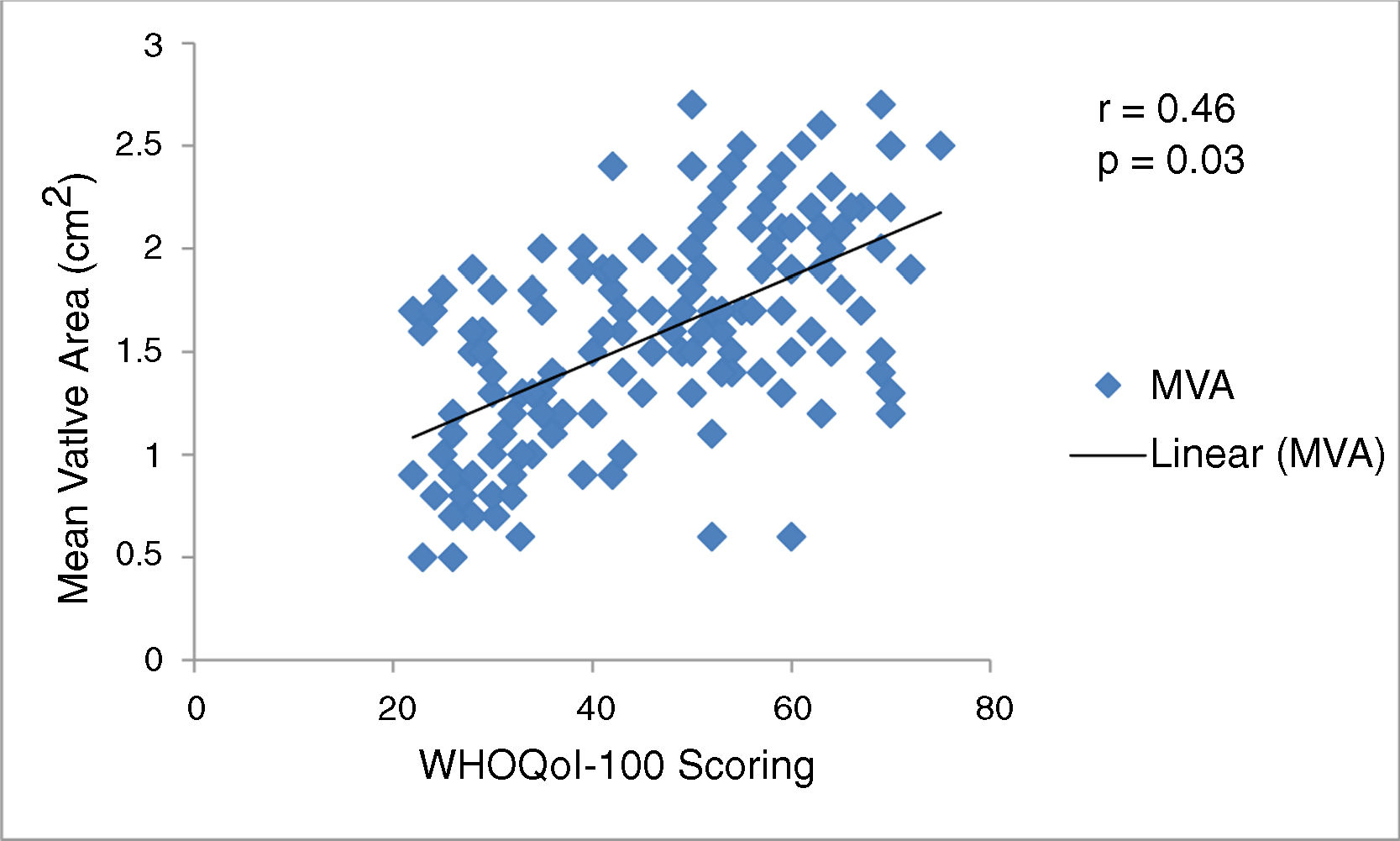
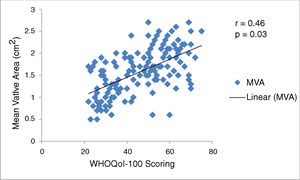
Resultsamong 96 patients, 64 (67%) were females and 32 (33%) were males. WHOQol scoring improved significantly after percutaneous transmitral commissurotomy from 32.8±8.9 to 54.6±11.2 and 62.8± 9.7, after one month and 3 months respectively. There was a significant association between net gain of MVA and WHOQol scoring with an R value of 0.46 and p value of 0.03. There was no difference in group comparison of all the six domains between male and female patients.
Conclusionsuccessful percutaneous transmitral commissurotomy improves the quality of life in mitral stenosis patients regardless of their gender and has a positive correlation with a net gain in mitral valve area.
La comisurotomía mitral percutánea se ha convertido en una opción terapéutica ideal para la estenosis mitral, debido a efectos menos adversos y a resultados más favorables. Los pacientes mejoran sintomáticamente tras la realización de esta técnica, aunque se dispone de escasos datos acerca de la calidad de vida tras su puesta en práctica.
ObjetivoEvaluar la calidad de vida luego de comisurotomía mitral percutánea mediante la puntuación WHOQol, que cubre diferentes aspectos de la vida, para determinar su correlación con la ganancia neta del área valvular mitral (AVM), y determinar su asociación con el sexo.
MétodosEstudio prospectivo de cohorte durante un periodo de 15 meses, en el que se incluyeron 100 pacientes con estenosis mitral a quienes se les practicó con éxito comisurotomía mitral percutánea. De entre el total incluido, se perdieron 4 pacientes durante el estudio, por lo que se recolectaron datos de los 96 pacientes restantes. La calidad de vida se evaluó antes del procedimiento, y transcurridos un mes y tres meses de seguimiento, utilizando el cuestionario de puntuación WHOQol.
ResultadosDe los 96 pacientes, 64 (67%) eran mujeres y 32 (33%) varones. La puntuación WHOQol mejoró considerablemente tras la realización de la comisurotomía mitral percutánea, con valores de 32,8±8,9 a 54,6±11,2 y 62,8± 9,7, transcurridos uno y 3 meses, respectivamente. Se produjo una asociación significativa entre la ganancia neta de AVM y la puntuación WHOQol, con un valor R de 0,46 y un valor p de 0,03. No se produjo diferencia alguna en cuanto a la comparación grupal de los seis dominios entre varones y mujeres.
ConclusiónLa comisurotomía mitral percutánea exitosa mejora la calidad de vida de los pacientes con estenosis mitral, independientemente del sexo, y tiene una correlación positiva con la ganancia neta del área valvular mitral.
There are multiple causes of mitral valve stenosis which include rheumatic heart disease, congenital heart disease, infective endocarditis, calcification, rare causes like SLE, carcinoid syndrome, Whipple disease, Fabry disease and rheumatoid arthritis. Among all, rheumatic heart disease (RHD) is the most abundant and leading cause of mitral valve scarring.1 The prevalence of RHD has declined globally but in underdeveloped countries, it is still highly endemic and most common cause of cardiovascular morbidity.2 The mitral valve is the most commonly involved valve in RHD.3,4 has a valve area of 4-6cm2 and causes symptoms when valve area becomes less than 2cm2. It is the most common valvular lesion of pregnancy and is poorly tolerated.5 Transthoracic echocardiography is the investigation of choice to diagnose mitral valve stenosis and to evaluate its area.6 Symptomatic mitral stenosis has different treatment options but percutaneous transmitral commissurotomy is the accepted treatment modality of choice in rheumatic mitral stenosis with favorable valve morphology7. The treatment of percutaneous transmitral commissurotomy started in 1980 and has evolved from double balloon to single Inoue balloon8. The efficacy results of the single balloon and double balloon are similar, but the single balloon has an added advantage of being more simple and having a more favorable safety profile.9 The percutaneous transmitral commissurotomy can provide symptomatic relief to patients of mitral stenosis who are planning to become pregnant and can be performed safely in the second trimester of pregnancy10. It can also treat mitral stenosis due to RHD, calcification or any other etiology effectively11.
The World health organization (WHO) defines health as not merely the absence of disease or infirmity but a state of mental, physical and social well-being12. The WHOQol 100 questionnaire was designed to assess the quality of life in six different domains13.This questionnaire was used to assess the quality of life in patients with chronic diseases in China14, but there is limited available data to evaluate the quality of life after percutaneous transmitral commissurotomy.
This study is therefore aimed to assess the quality of life after percutaneous transmitral commissurotomy using multimodal domains of WHOQol 100 questionnaire, determine its correlation with a net gain in mitral valve area and ascertain its association with gender.
Methods and materialsIt was a prospective cohort study carried out at the cardiology department of Rehman Medical Institute. Using a universal sampling technique, a total of 100 patients were enrolled over a period of 15 months. It included all those patients who had successful percutaneous transmitral commissurotomy done for mitral stenosis and had post procedure mitral valve area of more than 1.5cm2 on transthoracic echo. Patients with age, more than 20 years and less than 70 years, from both genders, multiple geographic locations, different socioeconomic status and diverse ethnic backgrounds were part of the study population.
Patient with aortic stenosis, hypertrophied obstructive cardiomyopathy (HOCM), severe mitral regurge 2+, severe aortic regurge 2+, new-onset atrial fibrillation, heart failure with NYHA class III/IV, myocardiaI infarction with regional wall motion abnormalities on echo, ejection fraction less than 40%, chronic renal disease with ultrasonographic evidence of renal parenchymal disease, chronic liver disease with ultrasonographic evidence of liver fibrosis, pericarditis and chronic obstructive pulmonary disease (COPD) with restrictive lung disease on spirometry were excluded from the study population because all of these conditions can invariably affect the quality of life. Informed written consent was obtained and confidentiality of the patients was maintained. Data was collected using WHOQoL-100 questionnaire before the procedure, after 01 months and 03 months of follow up. Ethical approval was obtained from the research and ethical unit (REU) of Rehman Medical Institute (RMI). Our study abided by the declaration of Helsinki.
The percutaneous transmitral commissurotomy procedure was done using femoral transvenous antegrade approach and mitral valve area was calculated noninvasively by transthoracic echo. Single Inoue balloon was used and balloon size was determined by height in the cm/10+10 formula. WHOQOL-100 questionnaire was completed, by asking questions using 24 facets in 6 domains along with 4 general facets and marking it from 0-5 with 0 being the worst and 5 being the best to assess the quality of life. A transformed total score was calculated at the end of the questionnaire to which each facet contributed equally and had a range from 0-100. High score denoted a better quality of life. Mitral valve area was measured echocardiographically by doing planimetry in parasternal-short axis view, from tips of mitral leaflets. Right ventricular systolic pressure was calculated by determining the pressure gradient between the right atrium and right ventricle from Doppler tricuspid jet in apical four chamber view using Bernoulli law P=4V2 and adding right atrial pressure determined from inferior vena cava collapsibility to it.
Statistical analysisThe data were analyzed using SPSS 20. Shapiro-Wilk test was used to check the distribution of data. Continuous variables were determined as mean ± standard deviation while categorical variables were determined as percentages and frequencies. T Test and ANOVA were used to compare the means. Pearson correlation coefficients were used to assess the correlation and relationship strength between continuous variables. A p value of less than 0.05 was considered significant.
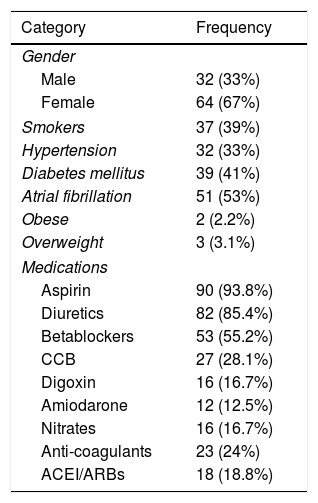
ResultsA total of 100 patients were enrolled in the study population who underwent percutaneous transmitral commissurotomy for mitral stenosis and had a valve area of more than 1.5cm2 on transthoracic echo, done after the procedure. Among the total, 4 patients were lost to follow up. Data were collected from 96 patients before the procedure and after the procedure over one month and 3 months follow up period which showed a mean age of 30.2 ± 3.8 years. Baseline characteristics are shown in Table 1.
Baseline characteristics of study population.
| Category | Frequency |
|---|---|
| Gender | |
| Male | 32 (33%) |
| Female | 64 (67%) |
| Smokers | 37 (39%) |
| Hypertension | 32 (33%) |
| Diabetes mellitus | 39 (41%) |
| Atrial fibrillation | 51 (53%) |
| Obese | 2 (2.2%) |
| Overweight | 3 (3.1%) |
| Medications | |
| Aspirin | 90 (93.8%) |
| Diuretics | 82 (85.4%) |
| Betablockers | 53 (55.2%) |
| CCB | 27 (28.1%) |
| Digoxin | 16 (16.7%) |
| Amiodarone | 12 (12.5%) |
| Nitrates | 16 (16.7%) |
| Anti-coagulants | 23 (24%) |
| ACEI/ARBs | 18 (18.8%) |
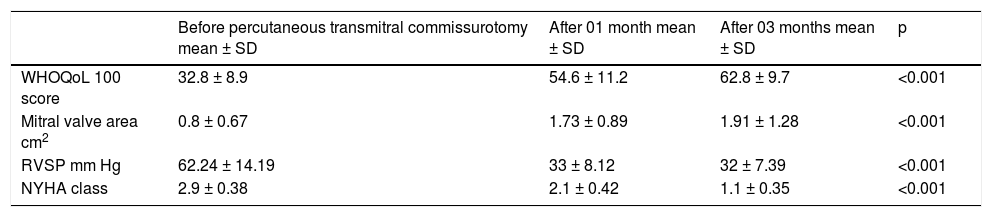
The mean value of four main variables was compared before the procedure after the procedure at one month and three months follow up period. There was a significant improvement in all the main variables, when measured before the procedure, at one month and three months follow up period on paired t-test with p<0.001 as shown in the Table 2 below.
Comparison of mean before and after percutaneous transmitral commissurotomy at 1 and 3 month follow up.
| Before percutaneous transmitral commissurotomy mean ± SD | After 01 month mean ± SD | After 03 months mean ± SD | p | |
|---|---|---|---|---|
| WHOQoL 100 score | 32.8 ± 8.9 | 54.6 ± 11.2 | 62.8 ± 9.7 | <0.001 |
| Mitral valve area cm2 | 0.8 ± 0.67 | 1.73 ± 0.89 | 1.91 ± 1.28 | <0.001 |
| RVSP mm Hg | 62.24 ± 14.19 | 33 ± 8.12 | 32 ± 7.39 | <0.001 |
| NYHA class | 2.9 ± 0.38 | 2.1 ± 0.42 | 1.1 ± 0.35 | <0.001 |
Chi square test was used to ascertain correlation between the WHOQol-100 scoring and increase in mitral valve area which showed statistical significance with p value of 0.03. Pearson correlation although positive, had a moderately positive coefficient(r) value of 0.46 as shown in the scatterplot graph in Figure 1.
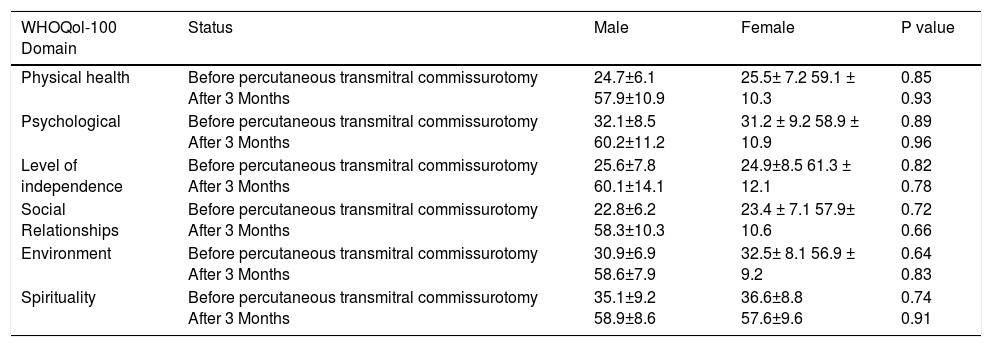
It was compared the group mean of six different domains of WHOQol-100 questionnaire with gender difference before percutaneous transmitral commissurotomy and after three months of the procedure. There was no significant group difference between male and female patients quality of life in all the six domains on ANOVA analysis as shown in Table 3.
Group correlation between gender with WHOQol-100 domains before percutaneous transmitral commissurotomy and after 3 months.
| WHOQol-100 Domain | Status | Male | Female | P value |
|---|---|---|---|---|
| Physical health | Before percutaneous transmitral commissurotomy After 3 Months | 24.7±6.1 57.9±10.9 | 25.5± 7.2 59.1 ± 10.3 | 0.85 0.93 |
| Psychological | Before percutaneous transmitral commissurotomy After 3 Months | 32.1±8.5 60.2±11.2 | 31.2 ± 9.2 58.9 ± 10.9 | 0.89 0.96 |
| Level of independence | Before percutaneous transmitral commissurotomy After 3 Months | 25.6±7.8 60.1±14.1 | 24.9±8.5 61.3 ± 12.1 | 0.82 0.78 |
| Social Relationships | Before percutaneous transmitral commissurotomy After 3 Months | 22.8±6.2 58.3±10.3 | 23.4 ± 7.1 57.9± 10.6 | 0.72 0.66 |
| Environment | Before percutaneous transmitral commissurotomy After 3 Months | 30.9±6.9 58.6±7.9 | 32.5± 8.1 56.9 ± 9.2 | 0.64 0.83 |
| Spirituality | Before percutaneous transmitral commissurotomy After 3 Months | 35.1±9.2 58.9±8.6 | 36.6±8.8 57.6±9.6 | 0.74 0.91 |
Health is not only an absence of disease or disability but is defined as a condition of mental, physical and social well-being by WHO.12 Quality of life is assessed by different tools but WHOQol-100 is validated as authentic one to assess the quality of life by WHO13 and is tested in patients with longstanding chronic diseases.14 Mitral stenosis is a chronic ailment which badly affects the quality of life.3,4 Percutaneous transmitral commissurotomy has evolved as an ideal treatment of choice not only in routine patients but can be carried out safely in pregnant patients as well.5 We are lacking data about its correlation with quality of life. This study was therefore aimed to assess the physical, social and mental wellbeing of patients after percutaneous transmitral commissurotomy using multimodal domains of WHOQol 100 questionnaire, to determine its correlation with a net gain in mitral valve area and ascertain its association with gender.
In this study, about 67% of the patients were females as compared to 33% males which are comparable with the results of Movahed et al.15 study in which mitral stenosis was more common in females, however, the cause of association was unknown. Khan et al.16 found, that symptomatic improvement occurs after percutaneous transmitral commissurotomy by improvement in NYHA score. In our study, the NYHA score improved from 2.9 ± 0.38 to 2.1 ± 0.42 and 1.1 ± 0.35, after one month and three months of percutaneous transmitral commissurotomy respectively. The leaflet mobility of mitral valve is improved to 1.5cm2 after which any further increase in MVA does not improve anterior and posterior leaflet mobility.17 This explains the subjective improvement and decrease in NYHA class after percutaneous transmitral commissurotomy in our subjects.
Our study showed that RVSP improved from 62.24 ± 14.19 to 33 ± 8.12 after one month and 32 ± 7.39 after 3 months of follow up which was consistent with the results of different studies in which the RVSP decrease in the majority of the patients after percutaneous transmitral commissurotomy.18,19 Evidence from multiple international studies carried in different countries shows that the mitral valve area improves after percutaneous transmitral commissurotomy.16,20 Our results showed that mitral valve area improved from 0.8 ± 0.67 before percutaneous transmitral commissurotomy to 1.73 ± 0.89 after one month and 1.91 ± 1.28 after 3 months of follow up.
Khan et al.16 stated that quality of life improves after percutaneous transmitral commissurotomy but showed no subjective evidence to measure it. Ay et al.21 showed that quality of life improves after mitral valve repair more than mitral valve replacement showing that native valve has more favorable outcomes then prosthetic valves. Regardless of primary procedure whether surgical or percutaneous transmitral commissurotomy, when percutaneous transmitral commissurotomy was done secondarily for restenosis, there was no difference in relation to gender.22 Our results showed that quality of life improves after percutaneous transmitral commissurotomy when measured using WHOQol-100 Questionnaire and it has significant correlation with net gain in mitral valve area with R value of 0.46 and p value of 0.03. Furthermore, there is no significant group difference in relation to gender among all the six domains of WHOQol-100 questionnaire.
LimitationSingle centered study was carried out which cannot truly depict the trend in the general population, however, it will provide references for further multicenter studies and clinical trials. Quality of life was assessed subjectively through history and may have been subject to both patient and observer bias, however, the probability remains same for all the domains. Mitral Valve area was assessed by transthoracic echo which is operator dependent and has its own limitations however standard precautions were adopted to minimize the bias and results were confirmed from 3 experienced operators.
ConclusionSuccessful percutaneous transmitral commissurotomy improves the quality of life in Mitral Stenosis patients. Quality of life has a positive correlation with a net gain in mitral valve area and there is no gender difference post-percutaneous transmitral commissurotomy in all the six domains of WHOQol-100 questionnaire.
Conflict of interestNone.