Knee arthroscopy is considered a safe procedure with low rate of complications. The aim of the study was to calculate the incidence of symptomatic thromboembolic events: deep vein thrombosis and pulmonary embolism, associated with knee arthroscopy and evaluate possible related risk factors.
Materials and MethodsRetrospective cohort study. Patients who underwent knee arthroscopy between January 2011 and December 2015 at a University Hospital were included. Follow-up was performed during the first 30 postoperative days. Demographic characteristics, symptomatic thromboembolic events, type of arthroscopic procedure and possible risk factors were recorded.
Results1,097 arthroscopic knee surgeries were performed in the 5 years of the study. 100% had 10-day postoperative follow-up and 90.5% of patients completed the 30-day follow-up. The mean follow-up time was 15.1 months. The rate of symptomatic thromboembolic events during follow-up was 1.4% (n= 14). There were two risk factors statistically associated with the outcome of the study: previous thromboembolic events (p= 0.013) and the current use of anticoagulants (p= 0.001). The mean age of the group with thromboembolic events was significantly higher (58 years) than that of the control group (46 years) (p=0.009).
DiscussionThe incidence of symptomatic thromboembolic events associated with knee arthroscopy was low. The routine use of thromboembolic prophylaxis is not recommended in patients undergoing this surgery. We recommend using it in patients with risk factors such as history of previous thromboembolic events and actual use of anticoagulants. Likewise, its use in patients over 50 years should be considered.
Level of evidenceIII, Retrospective Cohort Study.
La artroscopia de rodilla es usualmente un procedimiento seguro con pocas complicaciones. El objetivo de este estudio es calcular la incidencia de eventos tromboembólicos sintomáticos: trombosis venosa profunda y tromboembolismo pulmonar, asociados a artroscopia de rodilla y los posibles factores de riesgo relacionados.
Materiales and MétodosCohorte retrospectiva que incluyó todos los pacientes llevados a artroscopia de rodilla entre Enero 2011 y Diciembre 2015 en un hospital universitario. El seguimiento fue de 30 días después de la cirugía. Se registraron datos demográficos, los eventos de interés, el tipo de cirugía y los posibles factores de riesgo.
Resultados1,097 artroscopias de rodilla se hicieron en los 5 años. El 100% tuvieron seguimiento de 10 días mínimo, 90.5% alcanzaron el seguimiento de 30 días. El tiempo promedio de seguimiento fue 15.1 meses. El porcentaje de eventos tromboembólicos fue de 1.4% (n=14). Se encontraron dos factores de riesgo asociados: eventos tromboembólicos previos (p=0.013) y uso de anticoagulantes previo a la cirugía (p=0.001). La edad promedio fue mayor en los pacientes con eventos tromboembólicos comparado con los que no tuvieron eventos (58 vs 46 años), p=0.009.
DiscusiónLa incidencia de eventos tromboembólicos sintomáticos tras artroscopia de rodilla es bajo. El uso rutinaio de profilaxis tromboembólica no se recomienda. En los pacientes con historia de eventos tromboembólicos previos o que estpan anticoagulados en el momento de la cirugía, si se recomienda. Además, en los pacientes mayores de 50 años, debería considerarse su uso.
Nivel de EvidenciaIII, Estudio de Cohorte Restrospectiva.
Knee arthroscopy has brought advantages such as less complications, ambulatory procedures, earlier rehabilitation, reductions in costs and time until returning to work. It is one of the most frequent orthopedic procedures in the world.1 Complications associated with this procedure are rare; rates between 0.27% and 4.7% have been reported.2–5 Among these complications, thromboembolic events such as deep vein thrombosis (DVT) and pulmonary embolism (PE), have been considered infrequent, especially when compared to their occurrence during major surgeries such as joint replacements, where their incidence in the absence of thromboprophylaxis is approximately 40%.6 The incidence for knee arthroscopy has been found to be very low.7 It can be as low as 0.34% in symptomatic patients or as high as 17.9% in those who during the immediate postoperative period were screened with diagnostic images (asymptomatic cases).8–12 This variability may be due to factors such as the use of thromboprophylaxis, patient age, comorbidities and the type of surgical procedure performed.8,13,14
Currently, the routine use of thromboprophylaxis is not recommended in a regular patient undergoing knee arthroscopy. It would probably be indicated in patients with certain risk factors. However, its use remains controversial and it is yet to be determined which are those risk factors despite efforts to have a consensus.15
This study aims to estimate the incidence of symptomatic thromboembolic events after knee arthroscopy and establish the associated risk factors.
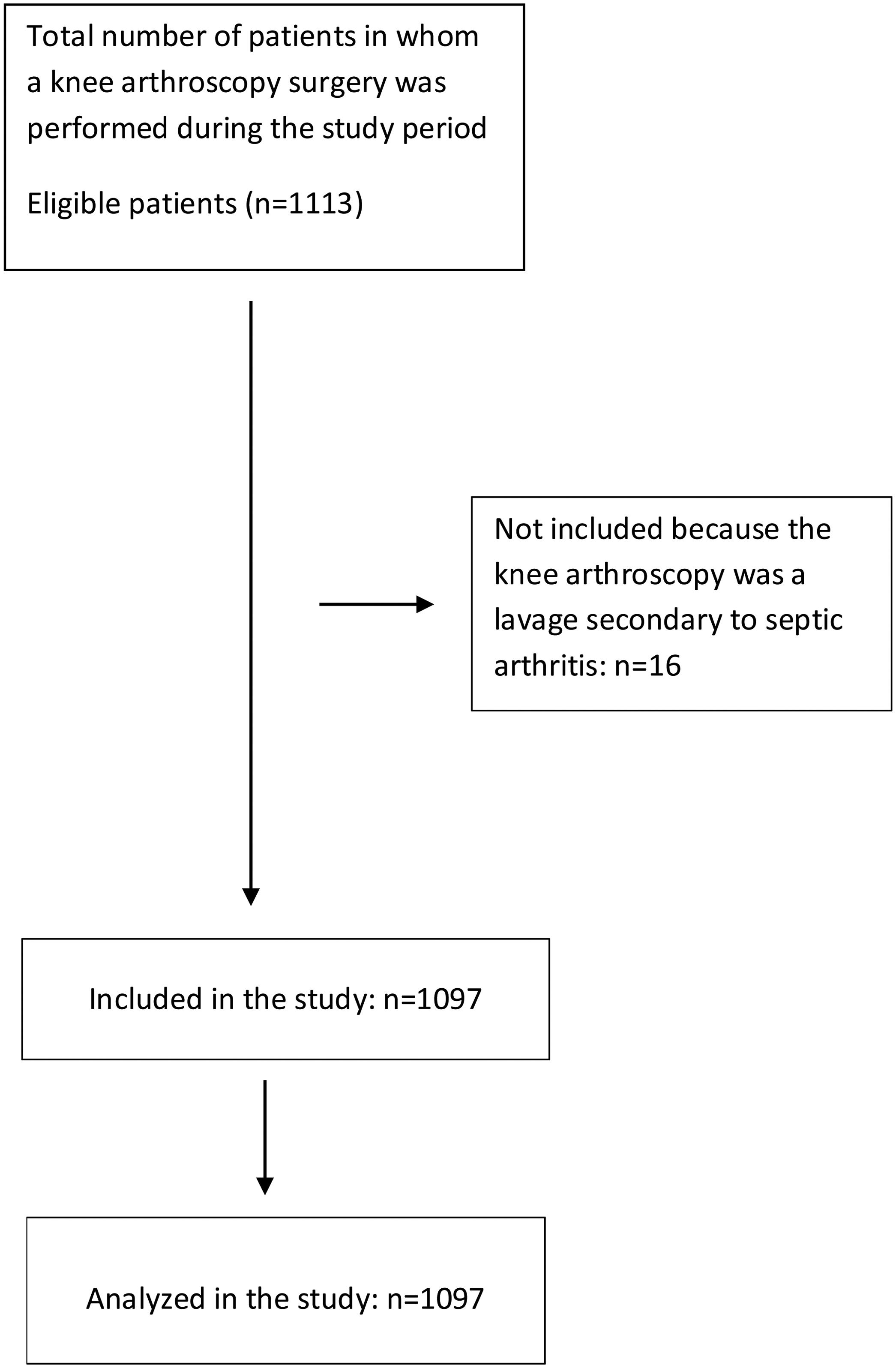
Materials and methodsType of study and populationRetrospective cohort with a nonprobabilistic sampling. All patients who underwent arthroscopic knee surgery between January 2011 and December 2015, treated at a Level 1 University Hospital (Fundación Valle del Lili, Cali, Colombia), were included. Patients were excluded when operated of arthroscopic lavage secondary to septic arthritis. Follow-up was planned to be during the first 30 postoperative days. Primary outcomes: pulmonary embolism and deep vein thrombosis were diagnosed with CT pulmonary angiogram and venous duplex ultrasound.
Data collection and managementSurgical codes that correspond to procedures guided by knee arthroscopy were identified (19 codes). With this information, the medical records in SAP NetWeaver digital computer system database of the hospital were searched. Each retrieved record was reviewed (verifying that each met the eligibility criteria). The flow diagram of patients included can be seen in Figure 1. The information of interest was extracted, and the data were later digitized in the BD Clinic clinical database administration system. Once the data collection was completed, quality control was performed. Ten percent of the records in the database were randomly selected and compared with the source documents (digital medical records), seeking to match the data.
Measures of central tendency and dispersion were used to group the quantitative data. For those variables with distributions that met normality criteria, the mean and standard deviation were calculated; the median and interquartile range were applied to the variables that did not met normal distribution criteria. The qualitative variables are presented as percentages. The comparison of the quantitative variables was performed using Student's t-test, while the qualitative variables were analyzed with the χ2 test.
Finally, relative risk with 95% confidence interval were calculated for the variables that were considered possible risk factors (age, comorbidities, smoking, previous anticoagulation, type of surgery, use of tourniquet and previous thromboembolic events). A result was considered statistically significant when the p-value was <0.05.
Ethical considerationsThis study was conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). The institutional review board (IRB) approved the study, considering that no informed consent was necessary because of the descriptive nature of it.
ResultsDuring the 5 years studied, there were 1097 arthroscopic knee surgeries. The average follow-up time was 15.1 months, with 992 patients (90.5%) completing the 30-day follow-up and 100% a 10-day follow-up. There were 14 symptomatic thromboembolic events (4 were DVTs and 10 were PEs). The incidence rate calculated for symptomatic thromboembolic events after knee arthroscopy was 1.4% (DVT=0.4%, PE=1%).
59% of the individuals in the group without events were male, compared with 50% in the group with events. The difference in median body mass index in the groups was not statistically significant. In both groups, operations on the right knee were more frequent. This information can be seen in more detail in Table 1. The type of surgical procedure most performed in both groups was chondroplasty (75%), followed by meniscectomy and anterior cruciate ligament reconstruction (Table 2). In both groups, there were some patients in whom more than one type of arthroscopic procedure was performed, without affecting the incidence of events (Table 3).
Baseline demographic characteristics of participants in those who had thromboembolic events and those who did not.
| Patients with DVT/PEn=14 | Patients with no events n=1083 | P-value | |
|---|---|---|---|
| Age, M (SD) | 58(16) | 46(17) | 0.009 |
| Sex, male (%) | 7(50) | 638(59) | 0.501 |
| BMI, Me (IQR) | 26(24-28) | 25(23-28) | 0.698 |
| Laterality of surgery, right (%) | 9(64) | 597(55) | 0.493 |
Note: M, mean; SD, standard deviation; BMI, body mass index; Me, median; IQR, interquartile range.
Arthroscopic knee procedures according to the presence or absence of thromboembolic events.
| Patients with DVT/PEn=14 | Patients with no eventsn=1083 | P-value | |
|---|---|---|---|
| Chondroplasty, n (%) | 13(93) | 813(75) | 0.209 |
| Meniscectomy, n (%) | 10(71) | 712(66) | 0.782 |
| ACL, n (%) | 2(14) | 274(25) | 0.537 |
| PCL, n (%) | 0 | 19(1.7) | NA |
| Medial patellofemoral ligament, n (%) | 0 | 18(1.7) | NA |
| Lateral retinacular release, n (%) | 0 | 13(1.2) | NA |
| Released adhesions, n (%) | 1(7) | 12(1) | 0.165 |
Note: ACL, anterior cruciate ligament; PCL, posterior cruciate ligament, NA, not applicable.
Comorbidities and possible risk factors associated with thromboembolic events in both groups of participants.
| Patients with DVT/PEn=14 | Patients with no eventsn=1083 | P-value | |
|---|---|---|---|
| Medical history | |||
| Smoking, n (%) | 1(7) | 87(8) | 0.473 |
| Cancer, n (%) | 1(7) | 26(2.4) | 0.27 |
| Rheumatic disease, n (%) | 1(7) | 13(1.2) | 0.054 |
| Previous thrombotic event, n (%) | 2(14) | 30(2.8) | 0.013 |
| Previous anticoagulation use, n (%) | 4(29) | 33(3) | 0.001 |
| Factors related to surgery | |||
| Thromboembolic prophylaxis, n (%) | 4(29) | 27(2.5) | 0.000 |
| Use of tourniquet, n (%) | 2(14) | 142(13) | 0.706 |
Two of the possible risk factors studied had a statistically significant association with the outcome of interest: history of previous thromboembolic events (p=0.013) and current use of anticoagulants (p=0.001). In addition, the mean age of patients in the group with thromboembolic events (58 years old) was significantly higher than that of patients in the healthy group (46 years old) (p=0.009).
The other possible risk factors did not show statistical significance association with thromboembolic events after arthroscopic knee surgery: sex (p=0.501), body mass index (p=0.698), type of surgical procedure (p=0.165-0.782), smoking (p=0.473), history of cancer (p=0.27), rheumatic disease (p=0.054) and use of tourniquets (p=0.706). Mortality during the follow-up time was 0.2% (n=2), with no relationship with the outcome of interest or surgery. Finally, there was a higher percentage of patients who received thromboembolic prophylaxis in the group that developed thromboembolic events than in the group without these events (p <0.001).
DiscussionThis study describes the incidence of symptomatic thromboembolic events and the risk factors associated with their development. With a total of 14 patients with events, the incidence rate for this population was 1.4%. This finding is within the range reported in the literature (0.34% to 3.7%) for symptomatic thromboembolic events after knee arthroscopy.10,12,16 Based on these results, we can conclude that the incidence of symptomatic thromboembolic complications for this type of surgeries is low.
Multiple studies have described the incidence of DVTs in arthroscopic knee surgery.17 Bohensky et al. conducted a retrospective study with a large cohort (180,717 knee arthroscopies) in which they analyzed complications associated with surgery in the first 30 and 90 postoperative days; at 30 days, they found that DVT was the most frequent complication (n=579, 0.32%).2 Mauck et al. found in a cohort of 4833 patients, 18 symptomatic thromboembolic events that developed in the first six postoperative weeks, including 16 DVT events, corresponding to an incidence rate of 0.34%.10 In our study, the incidence rate for symptomatic DVTs was 0.4%, very similar to those studies.
Regarding PE, the incidence rate calculated in our study was 1%, a value that is higher than hat has been reported elsewhere.7,10,12. In 2011, in New York, United States, a database with a total of 418,323 knee arthroscopies from 1997 to 2006 was analyzed, finding an incidence rate for symptomatic PEs of 0.028% (117 patients).7 Krych et al. analyzed 12,595 patients who underwent arthroscopic knee surgery across 2 decades in a single institution and found that within the first four postoperative weeks, there were 5 PEs (0.06%).12 The highest incidence reported is described in a study published in 2012, in which a cohort of 20,770 patients had 35 cases of symptomatic PE (0.17%).18
Regarding demographic and clinical variables, we only found a statistically significant difference in the age of the patients in the groups. The age of patients who presented thromboembolic events was, on average, 12 years older than those who did not present thromboembolic events. Therefore, we consider that older age increases the risk of developing thromboembolic events after arthroscopic knee surgery, a conclusion consistent with what has been previously reported in other studies.2,10,16 Although factors such as sex, body mass index and type of procedure performed by arthroscopy with thromboembolic complications have been historically correlated, in our study, those factors were not associated with the outcomes of interest.
In our study, PEs were more frequent than DVTs. This might be explained because patients are more likely to consult when they had respiratory distress than when they had pain in the gastrocnemius/soleus region. Therefore, the incidence of DVTs could be underestimated. It is very probable that patients with pulmonary embolism had concomitant DVTs that were not diagnosed, but that was the etiology of a thrombosis that eventually embolized to the lungs.
Within the history and perioperative variables studied, we found an increased risk for patients with previous history of thromboembolic events and in those who were receiving anticoagulants at the time of surgery. History of thromboembolic events was also identified by Krych et al. as a factor that increased 3 times risk of new events.12 In our study, the risk was 5 times higher for patients with history of previous thromboembolic events and 9.7 times higher for those using anticoagulants. Regarding the use of anticoagulants prior to the procedure, we did not find any relevant literature, but it is reasonable to assume that if someone is receiving anticoagulants due to a state of hypercoagulability, they have a greater risk of this type of events after stopping treatment for surgery and undergoing a surgical procedure. Until 2015, the percentage of patients who received prophylaxis after knee arthroscopy in our hospital was very low (2.8%).
History of smoking, cancer, or rheumatic disease and use of tourniquets were not related to the development of thromboembolic events during the postoperative period. The results are inconsistent with previous studies, in which an increased risk was observed in patients who had these characteristics.7,19This finding could be related to the sample size. Perhaps with a larger sample, an association could be found, or on the other hand, our population may not have these risk factors.
When venous ultrasonography is used to assess for DVT in every patient, the incidence found for these events is higher. Oshiba et al., found 6.6% incidence for DVT after anterior cruciate ligament reconstruction assisted with knee arthroscopy.20 Though, this ultrasonography is not routinely done and it is uncertain if asymptomatic patients may have worse outcomes than symptomatic patients.16
There are some limitations in our study. First, the retrospective analysis of patients limits data to what was written in the medical records; therefore, the presence of some variables could be underestimated, leading to information bias. The sample size was intermediate for a study of this nature, resulting in less statistical power to find associations with less frequent variables. Finally, approximately 10% of patients did not complete the 30-days follow-up period, therefore, the reported incidence could be underestimating or overestimating the real value.
ConclusionThe findings of our study show that despite the low incidence of symptomatic thromboembolic events after knee arthroscopy, there are certain risk factors that, when identified, make thromboembolic prophylaxis suitable. We do not recommend the routine administration of thromboembolic prophylaxis, except in patients with history of previous thromboembolic events and in patients who are using anticoagulants at the time of surgery. Likewise, its use should be considered in patients older than 50 years, given the results of this study.
FundingThere was no funding for this study.
Conflicts of InterestThe authors have no conflicts of interest.