Neuropsychiatry is a specialized clinical, academic and scientific discipline with its field located in the borderland territory between neurology and psychiatry. In this article, we approach the theoretical definition of neuropsychiatry, and in order to address the practical aspects of the discipline, we describe the profile of a neuropsychiatric liaison service in the setting of a large hospital for neurological diseases in a middle-income country. An audit of consecutive in-patients requiring neuropsychiatric assessment at the National Institute of Neurology and Neurosurgery of Mexico is reported, comprising a total of 1212 patients. The main neurological diagnoses were brain infections (21%), brain neoplasms (17%), cerebrovascular disease (14%), epilepsy (8%), white matter diseases (5%), peripheral neuropathies (5%), extrapyramidal diseases (4%), ataxia (2%), and traumatic brain injury and related phenomena (1.8%). The most frequent neuropsychiatric diagnoses were delirium (36%), depressive disorders (16.4%), dementia (14%), anxiety disorders (8%), frontal syndromes (5%), adjustment disorders (4%), psychosis (3%), somatoform disorders (3%), and catatonia (3%). The borderland between neurology and psychiatry is a large territory that requires the knowledge and clinical skills of both disciplines, but also the unique expertise acquired in a clinical and academic neuropsychiatry program.
La neuropsiquiatría es una disciplina médica cuyo campo clínico, académico y científico se localiza en el territorio fronterizo entre la neurología y la psiquiatría. En este artículo se aborda la definición teórica de la neuropsiquiatría y, con el objetivo de tratar los aspectos prácticos de la neuropsiquiatría, se describe el perfil de un servicio de interconsulta neuropsiquiátrica en el contexto de un hospital dedicado a las enfermedades del sistema nervioso, en un país de ingreso económico medio. Se incluyó a 1.212 pacientes evaluados consecutivamente en el Instituto Nacional de Neurología y Neurocirugía de México. Los diagnósticos principales fueron infecciones cerebrales (21%), neoplasias del sistema nervioso (17%), enfermedad cerebrovascular (14%), epilepsia (8%), enfermedades de la sustancia blanca (5%), neuropatías periféricas (5%), enfermedades extrapiramidales (4%), ataxias (2%) y traumatismos craneoencefálicos (1,8%). Los diagnósticos neuropsiquiátricos más frecuentes fueron síndrome confusional (36%), depresión (16,4%), demencia (14%), ansiedad (8%), síndromes frontales (5%), reacciones de ajuste (4%), psicosis (3%), trastornos somatoformes (3%) y catatonia (3%). El territorio fronterizo entre la neurología y la psiquiatría es extenso y requiere los conocimientos y fortalezas de ambas disciplinas, pero también la pericia entrenada mediante un programa clínico, científico y académico especializado.
Neuropsychiatry has been defined as “a field of scientific medicine that concerns itself with the relationship between human behavior and brain function, and endeavors to understand abnormal behavior and behavioral disorders on the basis of an interaction of neurobiological and psychological-social factors.”1 However, a critical history of neuropsychiatry has shown that this elusive term has different definitions according to philosophical assumptions, investigative techniques, patient populations and therapeutic goals; nevertheless, all forms of neuropsychiatric practice share the foundational claim that mental disorders are caused by changes in the physical conformation of the brain.2 According to Lishman, neuropsychiatry deals with the borderland between clinical neurology and clinical psychiatry. “Academic neuropsychiatry” is concerned with the brain mechanisms in relation to mental disorders, whereas “clinical neuropsychiatry” deals with those mental disorders which can be demonstrated to owe their origins to brain malfunction of a clearly identifiable nature.3 German Berrios defines neuropsychiatry as the discipline that studies the psychiatric complications of neurological disease, based on social and scientific narratives developed to understand and deal with mental symptoms found in the context of neurological diseases.4 According to the American Neuropsychiatric Association, the word “neuropsychiatry” may be used to describe a scientific field (the integrated study of psychiatric and neurologic disorders), but also a medical subspecialty, committed to understand the links between neuroscience and behavior, and to provide care to individuals with neurologically based behavioral disturbances. The Melbourne Neuropsychiatric Center defines neuropsychiatry as the intersection between basic and clinical neuroscience and psychiatry. As a clinical and scientific discipline, it combines principles derived from neurology, psychiatry and neurosciences in general and is often placed in the borders between them.5
This article describes the neuropsychiatric aspects of nervous system diseases and the aforementioned intersection between neurology and psychiatry in the context of a neuropsychiatric liaison service in a neurological center, The National Institute of Neurology and Neurosurgery of Mexico. This neuropsychiatric liaison service is clinically oriented, but it is also the basis for a subspecialty program for neurologists and psychiatrists, and provides support to a neuropsychiatric epidemiology research program. As other academic neuropsychiatric programs, it does not obviate the separate roles of neurology and psychiatry; instead, it covers the interface by assessing behavioral disturbances and cognitive impairments, for instance.6 Furthermore, the interface or borderland described in this paper includes both the field traditionally ascribed to behavioral neurology (starting with well-defined brain lesions related to deficiency syndromes such as aphasia, apraxia and agnosia), and the field ascribed to clinical neuropsychiatry (starting with mental symptoms and syndromes such as agitation, catatonia, and psychosis), as has been emphasized in other academic programs.7
Neuropsychiatric Experiences in a Multidisciplinary InstituteIn this article, we describe the philosophy of neuropsychiatry behind a specialized academic and clinical program from the National Institute of Neurology and Neurosurgery of Mexico. This is a large referral and academic center with a history of over half of a century. Its neuropsychiatric philosophy is informed by two sources: the first source is an interdisciplinary spirit that comes from the founder of the program, Dr. Dionisio Nieto, who was a former student of the Nobel Prize winner and Father of Neuroscience, Santiago Ramón y Cajal.8 As an example of this interdisciplinary spirit, Dr. Nieto was essentially a psychiatrist within the European psychopathological tradition, but also a neuropathologist. He was involved in the discovery of neurocysticercosis immunological reactions, which represented the first objective diagnostic tool for this parasitic disease. He also studied the role of copper in the neurochemistry of schizophrenia, the possibilities of limbic surgery, and the effectiveness of electroconvulsive therapy in the motor dysfunction of patients with Parkinson's disease. Dr. Nieto performed pioneering experiments with lithium in bipolar disorder patients from Latin America, but also, explored the phenomenology of the mind by testing hallucinogenic compounds (and using neuroscientific researchers as experimental subjects). Finally, he approached evolutionary neuroscience by writing a book on the brain morphology of dolphins. This wide array of interdisciplinary interest was complemented by a strong philosophical background with a particular interest in epistemology. The first source for our philosophy of neuropsychiatry is precisely the notion of interdisciplinary science. This interdisciplinary theory is scientific because it is built by the analysis of data which obtained by valid methods, and it is experimental because it tests hypothesis, generating new data by means of medical interventions in neuropsychiatric patients.
The second source of our philosophy of neuropsychiatry comes directly from clinical practice. The National Institute of Neurology and Neurosurgery is a large hospital with three hospitalization wards: neurosurgical, neurological, and psychiatric. This provides wide clinical experience that includes patients that are attended to in most psychiatric services around the world, including those with a diagnosis of schizophrenia, bipolar disorder, major depression or obsessive-compulsive disease. In our Institution, psychiatrists treat these patients who can be said to suffer from primary psychiatric disorders. However, a neuropsychiatric liaison service has been developed over the years to care for the hundreds of patients with neurological disorders presenting with behavioral abnormalities, cognitive dysfunctions, and the full range of mental symptoms. These neuropsychiatric phenomena are similar in many ways to the psychopathological features of the primary psychiatric disorders. However, there are also many differences regarding the form and content of these symptoms, and often the clinical competences that are relevant for assessment require special training, and a significant time investment to obtain expertise. These patients are often diagnosed as having primary psychiatric phenomena but in fact, have underlying neurological or systemic conditions that have a direct influence in mental state and behavior, so they require an extensive diagnostic workup that sometimes is not provided by psychiatrists, owing to lack of expertise. It also may not be provided by neurologists or neurosurgeons, as they frequently assume that the psychiatric symptoms are “psychological” in nature. This confounding aspect of mental symptoms in neurological patients leads to (at least) two kinds of diagnostic errors: the “false positive” error, in which a patient without a neurological disease is diagnosed as having one, and the “false negative” error, in which a neurological patient is diagnosed as having a primary psychiatric condition. Of course, we can also think of similar kinds of therapeutic mistakes. Prolonged clinical experience with this borderland between neurology and psychiatry provides a way to reduce these errors, especially if the clinician is instructed into the pertinent scientific traditions. From this, we obtain a medical specialist that has a professional background in psychiatry or neurology, but also a set of abilities and knowledge that are not part of the academic curriculum of psychiatry or neurology. This is the rational basis for a medical subspecialty profile.
In order to discuss this issue properly, we will describe the clinical-epidemiological profile of this borderland between the neurological and psychiatric services of the National Institute of Neurology and Neurosurgery.
The Practice of Neuropsychiatry: Learning From Clinical Experience at the National Institute of Neurology and NeurosurgeryMethodsAn observational study of neurologic patients undergoing neuropsychiatric assessment was performed. We included consecutive patients hospitalized in the Neurology, Neurosurgery, Intensive Care Unit, and Emergency Departments of the National Institute of Neurology and Neurosurgery of Mexico referred to the Neuropsychiatry Liaison Service for assessment due to psychiatric symptoms, from March 2007 to November 2012.
Data was gathered using the medical records. Age, sex, neurologic diagnosis according to the International Classification of Diseases in its tenth revision (ICD-10), and psychiatric diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders in its fourth edition Text Revision (DSM-IV-TR) at assessment were obtained. A systematic neuropsychiatric assessment was performed by clinical neuropsychiatrists, including semistructured interviews, cognitive evaluations, as well as clinical scales for the measurement of neuropsychiatric symptoms. According to the symptomatic diagnosis, specific scales were applied, such as the Bush and Francis Catatonia Rating Scale9 for patients with catatonia, and the DRS-98 for patients with delirium.10 The neuropsychiatric diagnosis was obtained by agreement between at least two clinical neuropsychiatrists, considering all sources of information, including routine neuropsychological tests.
Data was analyzed using SPSS for Windows (version 17.0). Numeric variables are described in terms of means±standard deviations, and categorical variables in terms of frequency of cases and percentages.
Overall Results1212 neurologic patients underwent neuropsychiatric assessment. Regarding the departments that requested the evaluation, 59% (n=715) of the requests were originated in the Neurology Department, 24.5% (n=297) in the Neurosurgery Department, 9.0% (n=109) in the Emergency Department, and 6.8% (n=83) in the Intensive Care Unit. The mean of age was 44.5±17.3 years. Six hundred and twenty three patients were males (51.4%).
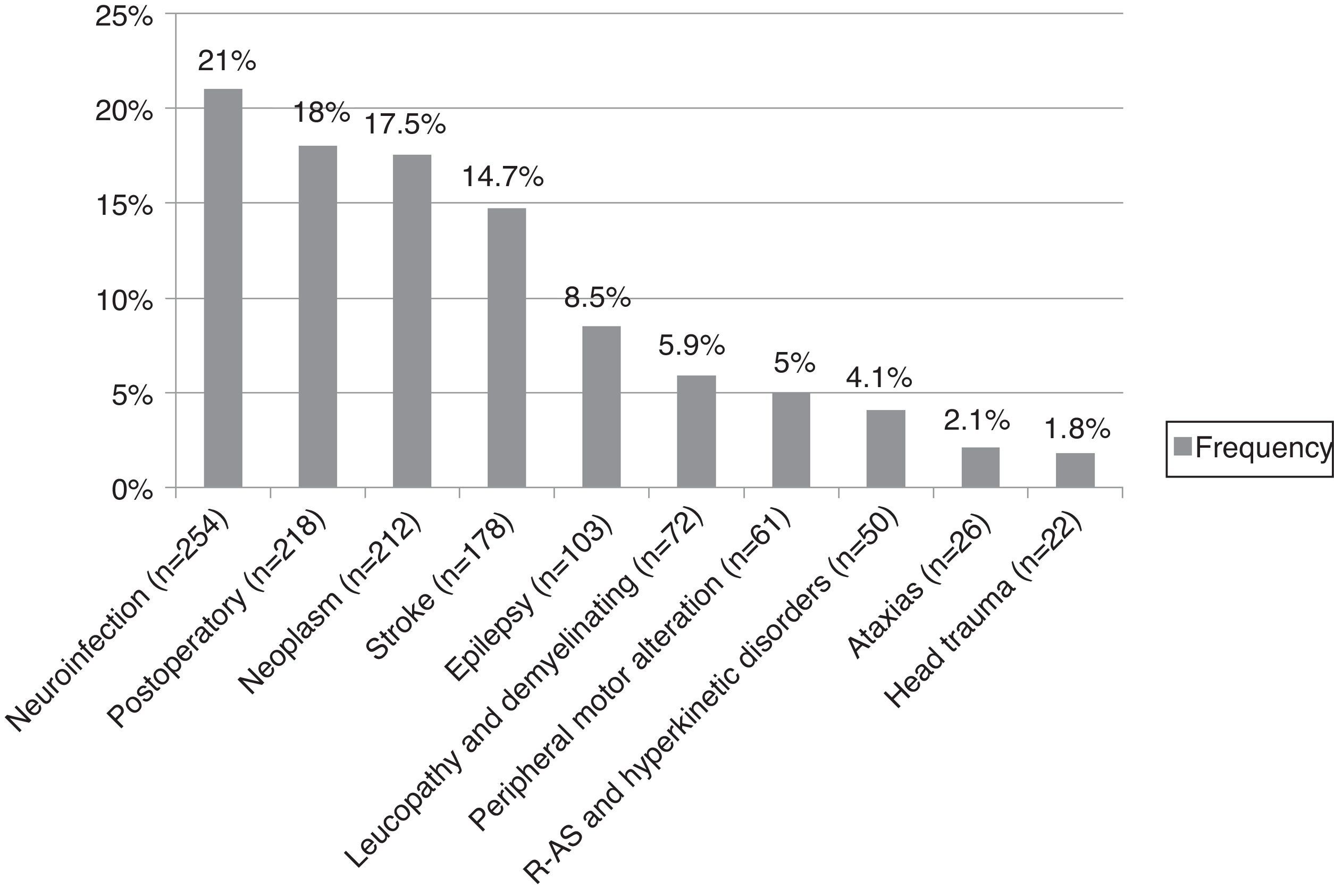
The nervous system diseases that required more evaluations by the Neuropsychiatric Liaison Service were neuroinfections (21%; n=254), with viral encephalitis as the leading cause (8.7%; n=105); patients in the neurosurgical postoperative period (18%; n=218); central nervous system neoplasms (17.5%; n=212); cerebrovascular disease (14.7%; n=178), with hemorrhagic disease as the most frequent subtype (7.7%; n=93); epilepsy (8.5%; n=103); and white matter and demyelinating diseases (5.9%; n=72). The frequency of neurological diagnoses appears in figure 1.
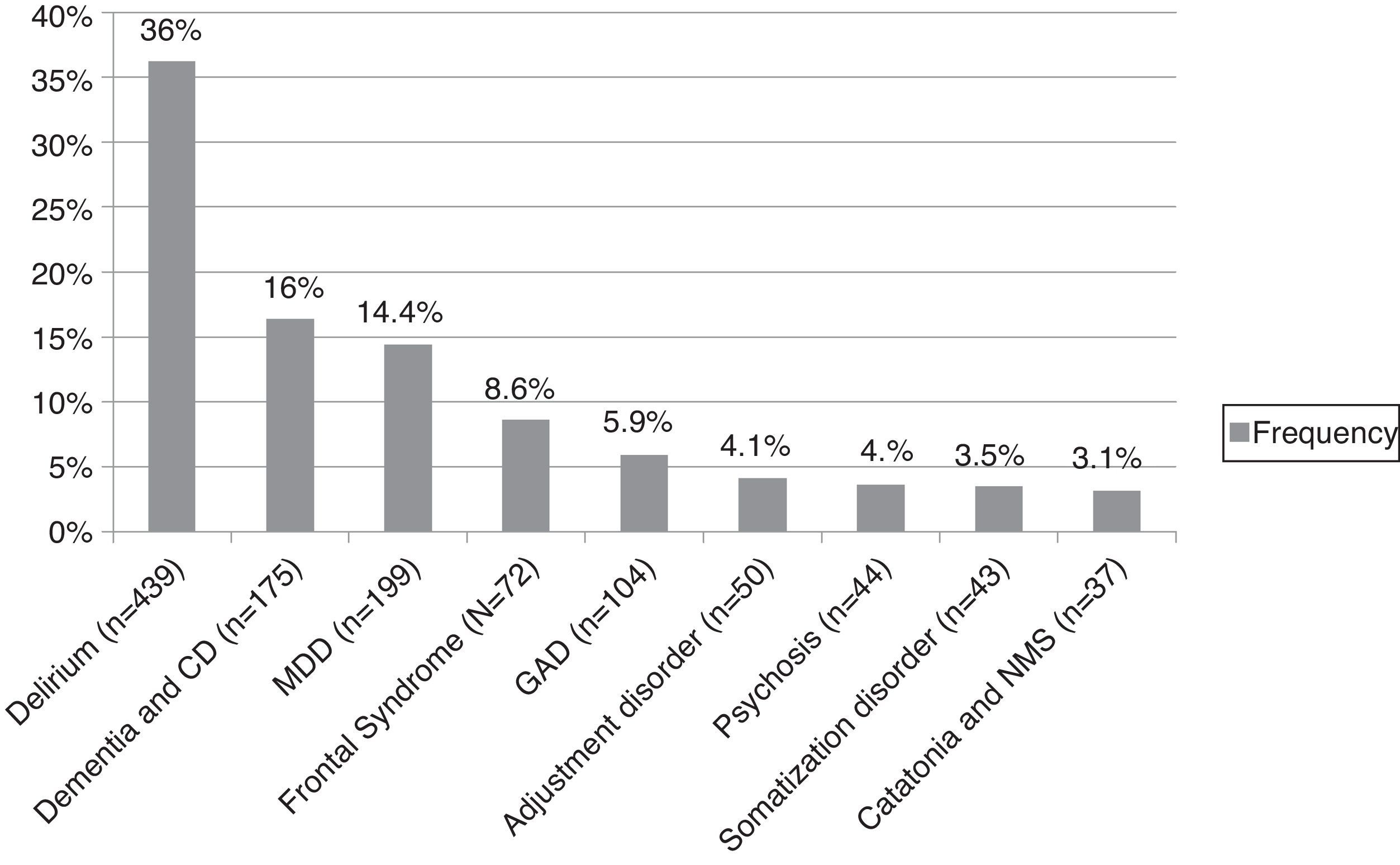
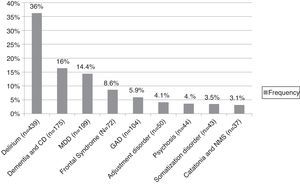
As may be seen in figure 2, the most frequent neuropsychiatric diagnoses were delirium (36.2%; n=439); major depressive disorder (16.4%; n=199); dementia and cognitive disorders (14.4%; n=175); anxiety disorders (8.6%; n=104); frontal syndromes (5.9%; n=72); adjustment disorders (4%); psychosis (3%); somatoform disorders (3%), and catatonia (3%).
DeliriumDelirium was diagnosed in 36.2% (n=439) of the total sample. The main neurological conditions in patients with delirium were: neurosurgical patients in the postoperative period (n=150), brain neoplasms (n=117), hemorrhagic stroke (n=61), viral encephalitis (n=56), and ischemic stroke (n=33).
Depressive DisordersDepression was diagnosed in 16.42% (n=199) of the patients undergoing assessment. The main neurological conditions in patients with depression were: brain tumors (n=27), epilepsy (n=15), neurosurgical postoperative conditions (n=15), ischemic stroke (n=12), human immunodeficiency virus (HIV) infection (n=12), and Guillain-Barré syndrome (n=11).
Dementia and Cognitive DisordersThe presence of any degree of cognitive decline was found in 14.4% (n=175) of the total sample. These patients presented epilepsy (n=12), ischemic stroke (n=11), leukoencephalopathy (n=10), neurocysticercosis (n=9), and HIV infection (n=8).
Anxiety DisordersAnxiety was found in 8.6% (n=104) of the patients. These patients had brain tumors (n=18), neurosurgical postoperative states (n=14), hemorrhagic stroke (n=10), viral encephalitis (n=9), and Guillain-Barré syndrome (n=7).
Frontal SyndromesFrontal syndromes were found in 5.9% (n=72) of the patients undergoing assessment. These patients were diagnosed with neoplasms (n=17), neurosurgical postoperative states (n=14), neurocysticercosis (n=10), ischemic stroke (n=4), toxoplasmosis (n=3), and ataxia (n=3). The medial frontal syndrome was the most frequent (n=24) presentation, followed by orbitofrontal and dorsolateral frontal syndromes (n=19 each).
Adjustment DisordersAdjustment disorders were found in 4.1% (n=50) of the sample. These patients presented neoplasms (n=12), neurosurgical postoperative states (n=11), Guillain-Barré syndrome (n=8), hemorrhagic stroke (n=6), bacterial meningitis (n=5), and transverse myelitis and cryptococcosis (n=4 each).
PsychosisA psychotic syndrome was found in 3.6% (n=44) of the patients. These were diagnosed with epilepsy (n=19), neurocysticercosis (n=6), brain neoplasms (n=5), viral encephalitis (n=4), and ischemic stroke and neurosurgical postoperative states (n=3 each).
CatatoniaCatatonia was diagnosed in 3.1% (n=37) of the total sample. These patients presented most frequently acute encephalitis (n=28) and epilepsy (n=4). The remaining cases corresponded to acute disseminated encephalomyelitis, leukoencephalopathy, subdural hematoma, and hemorrhagic stroke.
DiscussionLearning From Neuropsychiatric PracticeFrom an epidemiological perspective, it is quite clear that the data reported in this article is limited by the characteristics of its clinical setting, which is a problem shared by all studies arising from hospital-based populations. Some of the results confirm clinical and epidemiological data provided by previous studies, for instance, the recognition of a high neurological-psychiatric comorbidity. An epidemiological study analyzing data from several European psychiatric consultation-liaison services in general hospitals, focused in the patterns of neurological patients. Information was obtained from 33 neurological wards, with a total of 34 506 neurological admissions. Of these, 839 were referred to consultation-liaison psychiatry. Compared to other hospital wards, patients referred from neurology were more frequently diagnosed as suffering from somatoform and dissociative disorders.11 The Liaison Psychiatry service of Cork University Hospital described its experience with assessment of all in-patient neurology referrals over a 12-month period. Of 1685 neurology admissions, 106 (6%) were referred to liaison psychiatry. 91 referrals (86%) met criteria for a psychiatric disorder according to DSM-IV. Major depression (24%) and somatoform disorder (23%) were the commonest. Patients with multiple sclerosis or epilepsy comprised nearly half of all referrals.12 Our study differs slightly, because in our sample the highest frequency was obtained by delirium (36%), followed by depression (16%), whereas somatoform disorders were much more infrequent (3.5%). In an alternate clinical scenario, a study published with a population of psychiatric in-patients admitted to 16 private clinics and 6 private institutes showed that neurological diseases affected 13.05% of acute and 68.09% of chronic psychiatric patients.13 Frequent comorbidity seems to be the rule both in psychiatric as well as neurological wards, although some consultation-liaison services are most frequently required to assess patients with emotional problems,12 while other assess more patients with pseudoneurologic problems,11 and still others (like ours) are required to attend mostly patients with severe behavioral problems that disrupt the medical treatment or the hospital environment, as in the case of delirium patients with aggressiveness and agitation.
One of the earlier conclusions that can be obtained by our results and similar experiences is that the epidemiological profile of a neuropsychiatric liaison service shows clear differences as compared to the epidemiological profile of psychiatric hospitalization services. For instance, delirium was the main neuropsychiatric diagnosis in our sample. The frequency of delirium, a neuropsychiatric syndrome characterized by reduction in alertness, global and cognitive decline, and presence of hallucinatory phenomena,14 has been estimated in previous studies, ranging from 0.4% of the general population between 18 and 55 years, and increasing up to 1.1% in older patients. In a hospital setting the frequency raises up to 10-30% of the patients.15 It has also been estimated in a neurological scenario, observing the presence of delirium in up to 14.9% of the patients.16 Multi-causality as a determining factor for the presence of delirium must be considered in all cases,16,17 and this fact stresses one of the defining characteristics of neuropsychiatry: the clinical neuropsychiatrist must have an extensive and profound knowledge of the multiple neurological and systemic entities that might lead to abnormalities of alertness and consciousness. Although neurologists, internists and intensivists are well trained to identify and adequately workup patients in the coma spectrum, delirium may be a frequent source of confusion in the practice of these specialties, because usually these specialists have insufficient training in psychopathology.
Regarding emotional disorders and psychological adjustment, this category was frequently diagnosed in our study and is reported in many studies of neurological patients. Changes in emotional processing may be a result of disturbed brain mechanisms, psychological adjustment mechanisms, or both. In our sample, this was represented by the high frequency of depressive and anxious disorders, as well as adjustment reactions; this is expected according to previous studies. For instance, in a prospective cohort study set in a neurology service in Edinburgh, Scotland, 300 newly referred consecutive outpatients were assessed for anxiety and depressive disorders. 140 (47%) met criteria for one or more DSM-IV anxiety or depression diagnoses. Major depression was the most common (27%).18 The analysis of this topic poses a particular challenge both at the academic and clinical levels. It requires that clinicians have the technical knowledge and the clinical skills to recognize not only depression, mania, and anxiety disorders, but also that they are capable of distinguishing this conditions from other emotional processing disorders that are superficially similar, but that have a radically different medical significance (mainly because of their neurologic origin): Klüver-Bucy syndromes,19 apathic syndrome, involuntary emotional expression disorder, moria, as well as the emotional changes observed in patients with Urbach Wiethe disease. Another critical point for discussion is the frequent occurrence of adjustment reactions in neurological patients. This challenges the notion of neuropsychiatry as an ultra-materialistic discipline that seeks for a materialistic reductionism. Defense mechanisms, as conceptualized by psychodynamic psychiatry, may have an important role in symptom formation. Quoting German Berrios, “neurological patients have reasons for their symptoms, that is, neurological diseases happen to real people and hence have semantic contexts. This adds an entire new layer of meaning, hermeneutics and therapeutic response.”4 An important question for the epistemology and the clinical semiology of neuropsychiatry might be formulated as follows: in some cases, the mental symptom may be considered a manifestation of an abnormal brain signal provoked by a pathological process; in other cases, however, the mental symptom can be understood as a symbol in need for an hermeneutic approach. How can the clinicians know when should they use one approach or the other? As well, this issue has implications regarding the research agenda of neuropsychiatry, which should include (in the proper contexts) some methods of qualitative research along with the more widely used quantitative methods.
Somatoform disorders were present in our sample, reflecting the need for a differential diagnosis between neurological and the so-called “pseudoneurological” syndromes, and the combination of neurological and psychiatric skills required to diagnose these disorders. Previous studies have shown that, as compared to other contexts within general hospitals, patients referred from neurology wards are more frequently diagnosed with somatoform and dissociative disorders.11 A study done with 199 neurology patients referred to a psychiatric consultation-liaison service revealed that the most common reasons for referral were conversion symptoms, including pain and pseudoseizures.20 Somatoform disorders represent a highly valuable source for interaction between neuroscientific and psychodynamic schools at a theoretical level; however, patients with these diagnoses should be carefully assessed to rule out atypical presentations of neurological disease.
Our study found a frequency of 14.4% of cases of dementia and other less severe forms of cognitive impairment as main reasons for referral to the neuropsychiatry service. Although the high frequency of dementia due to degenerative disorders is well known in developed and developing countries, in the context of open population surveys,21 our sample focuses in neurological hospitalized patients and highlights the topic of secondary dementias, related to epilepsy, stroke, leukoencephalopathy, brain cysticercosis and HIV infection. The ability to establish a differential diagnosis of patients with major and minor cognitive disorders, as well as therapeutic skills in this populations, are relevant parts of the academic profile of neuropsychiatrists.
The cluster of behavioral, affective and cognitive phenomena associated to frontal syndromes was frequently diagnosed in our sample. The three stereotyped behavioral presentations of frontal lesions (medial-apathetic, orbital-disinhibited, and dorsolateral-disexecutive) were present in the sample, as well as mixed forms, although one academic observation concerns the lack of precise criteria for diagnosis of these three syndromes. Most authors agree that prefrontal signs and symptoms may be produced not only by damage of the prefrontal cortex, but by several processes affecting the other components of the fronto-subcortical circuits (including white matter, caudate nucleus, accumbens nucleus, globus pallidus, and the anterior and dorsomedial thalamic nuclei). The academic curriculum of neuropsychiatry needs to deal with prefrontal syndromes, as well as with the white matter and subcortical pathology that may lead to clinical features resembling frontal lobe damage.22
Psychosis was also a frequent cause of consultation in our study. The most frequent underlying neurological disorder, as expected, was epilepsy, a well-known comorbidity.23 However, other neurological diseases should be considered in this differential diagnosis, for instance neurocysticercosis,24 brain neoplasms,25 viral encephalitis,26 and vascular psychosis.27 Neuropsychiatrists should be expert specialists in the medical and neurological approach to psychosis, including other pathological entities that are represented in other studies: prion diseases, systemic autoimmune diseases, anti-NMDA encephalitis.
Catatonia was another important diagnosis in our sample. It has been pointed previously that this syndrome may be present both in neurologic and psychiatric patients, and it represents a diagnostic and therapeutic challenge.28 Patients with agitated catatonia may have a risk of severe adverse events with use of typical antipsychotics,28 and its recognition and detailed description requires specific skills that are infrequent in general psychiatrists and neurologists. This is the kind of disorder that may represent medical challenges in the borderland.
Conceptualization of Neuropsychiatry: a Clinical-Scientific Discipline Dedicated to the Borderland Between Neurology and PsychiatryThis study highlights frequent occurrence of psychiatric phenomena in patients with well-established nervous system diseases. From an academic and clinical perspective, the borderland between clinical neurosciences represents a problematic issue, because neither neurological nor psychiatric traditional approaches show enough emphasis in these clinical problems.5 This training problem has been pointed out by previous authors, for instance from the McLean Hospital Neuropsychiatry and Behavioral Neurology Service, the King's College Hospital and the Joint Committee on Subspecialty Certification of the American Neuropsychiatric Association (ANPA), and the Society for Behavioral and Cognitive Neurology (SBCN).29
At the National Institute of Neurology and Neurosurgery of Mexico, this borderland is the deontological foundation of a clinical, academic and scientific program dedicated to neuropsychiatry as a subspecialty derived both from neurology and psychiatry. Regarding the boundaries of these disciplines, one must remember that historically, neurology studies disorders with a proven organic basis, whereas psychiatric disorders are mainly defined by the phenomenology and course of the symptoms,30 although this definition does not account for several diagnostic entities within neurology (such as migraine and other forms of headache). It is quite possible that academic and professional conventions which are shaped beyond a pure scientific approach define the scope of these complementary medical specialties. However, decades ago it was predicted that the development in neuroscience would rekindle interest in neuropsychiatry, and increase all levels of interaction between psychiatrists and neurologists in teaching hospitals, expanding the interface between psychiatry and neurology.31 Other authors called to enlarge this interaction territory to include neuropsychology.32
According to some academic leaders, neurology and psychiatry have been separated by an artificial wall created by the divergence of their philosophical approaches and research and treatment methods, but scientific advances in late 20th Century and early 21th Century have shown that this separation could be arbitrary and counterproductive. However, there are several implications from the increasing recognition of the frequency and burden of psychiatric disturbances among patients with neurological disease for training, service provision and research. Training of both neurologists and psychiatrists needs to include knowledge and skills in the recognition and treatment of common disorders. As pointed out in a previous paper, the gap between this aspiration and the current service is considerable.33 Few working models of interdisciplinary teams share expertise in real time, while providing clinical and academic training to neurology and psychiatry residents. The McLean Hospital Neuropsychiatry and Behavioral Neurology service reported their experience regarding the integration of a team comprising psychiatrists, neurologists, and neuropsychologists, which can function effectively as a unit while providing enriched cross-specialty training for fellows, residents, and medical students.34 A similar experience has been reported in the National Institute of Neurology and Neurosurgery of Mexico.35
The complementarity of clinical approaches between neurology and psychiatry requires a careful appreciation of the advantages of each approach. As has been previously stated, “the strengths of psychiatry lie in the rich description of mental phenomena, well-developed interviewing skills, understanding of multiple causation of behavioral disturbance, appreciation of individual variation, ability to deal with ambiguity, interpersonal context, and the combination of biological with psychological and behavioral therapies. Equally, neurology prides itself in its rigorous clinical examination skills, its empiricism, and its objectivity.”5 However, one of the most stimulating challenges in the development of an effective interaction space between both disciplines relates to the mutual transfer of information according to the clinical language of each discipline.
Conflicts of interestThe authors have no conflicts of interest to declare.