People with schizophrenia and bipolar disorder (BD) have a high risk of unwanted pregnancies and abortions, due to their condition of vulnerability or hypersexuality (common in BD). This is associated with difficulty in planning their actions and lack of sex education and counselling by medical personnel, and can lead to adverse obstetric outcomes and inability to care adequately for their children.
ObjectiveTo describe the characteristics in terms of sexual and reproductive health, and the use of contraception and counselling in psychiatric consultations, in a sample of patients with BD and schizophrenia in Medellin, Colombia.
MethodsObservational cross-sectional study. We included the 160 participants from the clinical trial, “The effects of a multimodal intervention programme in patients with bipolar disorder and schizophrenia”, who were recruited from the mood and psychosis disorders group clinic at Hospital Universitario de San Vicente Fundación in Medellin. They were contacted by phone by a third-year psychiatry resident, who applied a survey about the characteristics of their sex life, contraception and reproduction.
ResultsAlmost all of the patients with schizophrenia were single, had no undergraduate studies and were unemployed. No significant differences were found regarding the age of starting sexual relations when comparing by diagnosis and gender. Almost all patients with schizophrenia and almost half of the patients with BD reported not having an active sexual life. Almost all of those who admitted to having an active sexual life claimed to always use contraception; in the BD group, only 48.8% of single women admitted to using contraception and a little over half of men stated that they used a condom when having sex. A quarter of the pregnancies were unplanned. Although the majority of the patients stated that they had never received information about family planning in the consultations with their psychiatrist, 57.4% of the patients with BD and 78.8% of those who had schizophrenia, considered themselves to be well informed on the subject.
ConclusionsPatients with mental illness have cognitive and behavioural alterations that affect their sexual and reproductive lives. Psychiatrists should therefore address this issue, to ensure education in areas such as contraception, family planning and sexually transmitted diseases and help safeguard the safety and quality of life of their patients.
Las personas con esquizofrenia y trastorno afectivo bipolar (TAB) tienen alto riesgo de embarazos no deseados y abortos, debido a su condición de vulnerabilidad o comportamientos hipersexuales (frecuentes en este último trastorno); a esto se asocia dificultad en la planeación de sus actos y escasez de educación sexual y consejos del personal médico, lo cual lleva a resultados obstétricos negativos e incapacidad para cuidar adecuadamente a sus hijos.
ObjetivoDescribir las características de una muestra de pacientes con trastorno bipolar y esquizofrenia en Medellín, Colombia, sobre salud sexual y reproductiva, el uso de anticoncepción y el asesoramiento al respecto en las consultas de psiquiatría,.
MétodosSe realizó un estudio observacional de corte transversal. Se incluyó a los 160 participantes del ensayo clínico «Los Efectos de un Programa de Intervención Multimodal en Pacientes con Trastorno Afectivo Bipolar y Esquizofrenia», captados de la consulta del grupo de trastornos del ánimo y psicosis del Hospital Universitario San Vicente Fundación de Medellín. Un residente de tercer año de Psiquiatría contactó con ellos vía telefónica y les aplicó una encuesta acerca de las características de su vida sexual y reproductiva y la anticoncepción.
ResultadosCasi todos los pacientes con esquizofrenia estaban solteros, no tenían estudios de pregrado y se encontraban desempleados. No se encontraron diferencias significativas en cuanto a la edad de inicio de las relaciones sexuales al comparar por diagnóstico y por sexo. Casi todos los pacientes con esquizofrenia y casi la mitad de los pacientes con TAB reportaron no tener vida sexual activa. Casi todos los que reconocieron tenerla afirmaron que usaban siempre algún método anticonceptivo; del grupo de TAB, solo el 48.8% de las mujeres solteras reconocieron estar planificando y poco más de la mitad de los varones afirmaron que se servían del condón en sus relaciones sexuales. Una cuarta parte de los embarazos fueron no planeados. El 57.4% de los pacientes con TAB y el 78.8% de los que tenían esquizofrenia se consideraban bien informados sobre planificación familiar, a pesar de que la mayoría afirmaba que nunca habían recibido información sobre este tema durante las consultas con su psiquiatra.
ConclusionesLos pacientes con enfermedad mental tienen alteraciones cognitivas y conductuales que afectan a su vida sexual y reproductiva, por lo cual los psiquiatras deben abordar este tema para garantizar la educación en cuanto a anticoncepción, planeación de la natalidad y riesgo de enfermedades de transmisión sexual, entre otras, y así velar por la seguridad y la calidad de vida de sus pacientes.
Schizophrenia and bipolar disorder (BD) are chronic conditions which mainly affect individuals of childbearing age, with prevalences worldwide of 1 and 4% respectively.1 They are characterised for being affective and cognitive disorders which lead to a marked deterioration in reasoning and judgement2–5 and affect their sexual and reproductive life to a great extent; this risk is increased by the concomitant use of psychoactive substances, which reaches prevalences of between 25 and 65% in this population.6–9
Women with these disorders have a high risk of unwanted pregnancies and abortions, partly due to the difficulty they have in planning and measuring the consequences of their actions, which includes the lack of use or the inappropriate use of methods of contraception.3,5,10 There are reports in the literature that only 58.8% of women with BD use a method of contraception11; furthermore, there is evidence that patients with schizophrenia have a high percentage of unwanted pregnancies, despite the fact that the overall rate of pregnancy in this population is low.12 In addition, in both disorders there is a greater risk of negative obstetric outcomes, such as premature births, children with a low birth weight and recurrence of psychotic and affective symptoms during pregnancy.6,7,13–16
Other associated factors include their condition of vulnerability, which exposes them to being forced to have unwanted sex and, in the case of women with BD, hypersexuality is a clinical characteristic of the manic phase.10–12,17 Mentally ill parents may not be able to respond to the needs of their children, and delegate their care to others or run the risk of being separated from them.10,18
Added to this is that many of these patients receive antiepileptic drugs as part of their treatment and some of them may reduce the plasma concentration of oral contraceptives and reduce their efficacy15,19–21; in addition, there are mood stabilisers which can increase the teratogenic risk of this population.11,16 Paradoxically, oral contraceptives may reduce the concentrations of some psychotropic drugs and increase the risk of psychiatric decompensation.15,19,21,22
Furthermore, there is evidence that few women with a mental illness (MI) tend to ask for advice on contraception, and 32.2% of a sample of this population reported that they had never received information regarding this.5 This indicates that the evaluation and education on the topic in Psychiatry consultations is limited, due to factors such as: lack of knowledge of the psychiatrist on the use of contraceptives, the perception that this evaluation does not correspond to the mental health consultation, avoidance of the topic, the false belief that subjects with schizophrenia are asexual or even that antipsychotics protect against pregnancy due to secondary hyperprolactinaemia,4,18,23,24 due to pressure for the use of permanent methods of contraception considering that this population has limited self-determination ability17,18 and due to the limited information about this topic in the literature.11,15,25
The objective of this study was to describe the characteristics of a sample of patients with BD and schizophrenia in Medellín, Colombia, on sexual and reproductive health, the use of contraception and advice with regard to Psychiatry consultations.
MethodsAn observational, cross-sectional study was carried out. The enrolled patients were part of the clinical trial "The effects of a multi-modal intervention programme in patients with bipolar disorder and schizophrenia" and were recruited from the group consultation on mood disorders and psychosis at the Hospital Universitario San Vicente Fundación [San Vicente Foundation University Hospital] (HUSVF) in the city of Medellín. The evaluations were carried out between March and September 2016.
Ethical aspectsThis research had the approval of the ethics committee at the Medical Research Institute of the Faculty of Medicine of the Universidad de Antioquia (Antioquia University) and the HUSVF.
Inclusion and exclusion criteriaThey were the same as the source study: patients with a diagnosis of BD and schizophrenia, according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR),26 aged between 18 and 60, who were educated for longer than five years, were in a euthymic state at the time of the interview and who were in good health. In addition, they were accompanied by a family member or a close friend and signed the informed consent form after it had been explained to them by the professional. Patients who had received electroconvulsive therapy (ECT) with anaesthesia and relaxation in the past six months, those with a history of severe traumatic brain injury, who had a diagnosis of intellectual disability or schizoaffective, autism spectrum or personality disorder and those who had incomplete data in their medical records were excluded.
ProceduresFor this study, 301 participants from the source study were included. They had previously undergone the Diagnostic Interview for Genetic Studies (DIGS)27 by a trained psychiatrist, translated and validated version for Colombia, in order to confirm the psychiatric diagnosis and obtain a complete medical record.
Subsequently a third-year psychiatry resident contacted them by phone to explain this new project and the importance of carrying it out. After accepting their participation, a survey was then issued, designed by our research group, which consisted of some open questions about demographic data and personal history, followed by 18 multiple choice or dichotomous questions, aimed at investigating the characteristics of the sex life, contraception and reproduction of this population.
Statistical analysisThe groups were described according to the nature of the variables. In the qualitative variables, absolute and relative frequency measurements, expressed as percentages, were used. For the quantitative variables, the mean [interquartile range] was used. The software used was IBM SPSS version 23.0.
ResultsOf the 301 patients enrolled with a diagnosis of BD and schizophrenia, 141 were excluded due to the fact that they refused to participate in the research or it was not possible to contact them. In total, 160 patients were interviewed over the phone.
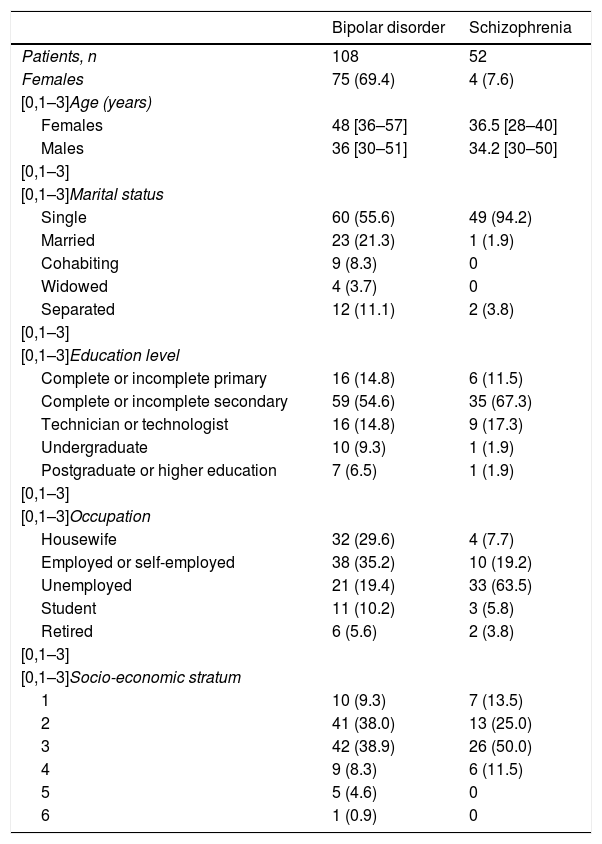
In the analyses of socio-demographic variables, the percentages of males and females were similar, but, after dividing up by groups according to the diagnosis, males predominated among participants with schizophrenia and females in the group with BD (92.3 and 69.4%, respectively). The mean ages were similar in both groups and more than 70% belonged to socio-economic strata 2 and 3. A total of 94.2% of the patients with schizophrenia were single, compared to only 55.2% of those who had BD; in addition, a third of patients were married or cohabiting in this last group. Almost all participants had managed to at least start or finish secondary school education, but very few had achieved undergraduate, postgraduate or higher education. This was more evident in the group of patients with schizophrenia. Regarding occupation, 63.5% of the participants with schizophrenia were unemployed and only 19.2% had a job; while in the group with BD, 35.2% were working, 29.2% did household chores and almost 20% were unemployed (Table 1).
Socio-demographic variables.
| Bipolar disorder | Schizophrenia | |
|---|---|---|
| Patients, n | 108 | 52 |
| Females | 75 (69.4) | 4 (7.6) |
| [0,1–3]Age (years) | ||
| Females | 48 [36–57] | 36.5 [28–40] |
| Males | 36 [30–51] | 34.2 [30–50] |
| [0,1–3] | ||
| [0,1–3]Marital status | ||
| Single | 60 (55.6) | 49 (94.2) |
| Married | 23 (21.3) | 1 (1.9) |
| Cohabiting | 9 (8.3) | 0 |
| Widowed | 4 (3.7) | 0 |
| Separated | 12 (11.1) | 2 (3.8) |
| [0,1–3] | ||
| [0,1–3]Education level | ||
| Complete or incomplete primary | 16 (14.8) | 6 (11.5) |
| Complete or incomplete secondary | 59 (54.6) | 35 (67.3) |
| Technician or technologist | 16 (14.8) | 9 (17.3) |
| Undergraduate | 10 (9.3) | 1 (1.9) |
| Postgraduate or higher education | 7 (6.5) | 1 (1.9) |
| [0,1–3] | ||
| [0,1–3]Occupation | ||
| Housewife | 32 (29.6) | 4 (7.7) |
| Employed or self-employed | 38 (35.2) | 10 (19.2) |
| Unemployed | 21 (19.4) | 33 (63.5) |
| Student | 11 (10.2) | 3 (5.8) |
| Retired | 6 (5.6) | 2 (3.8) |
| [0,1–3] | ||
| [0,1–3]Socio-economic stratum | ||
| 1 | 10 (9.3) | 7 (13.5) |
| 2 | 41 (38.0) | 13 (25.0) |
| 3 | 42 (38.9) | 26 (50.0) |
| 4 | 9 (8.3) | 6 (11.5) |
| 5 | 5 (4.6) | 0 |
| 6 | 1 (0.9) | 0 |
Unless otherwise specified, the values express n (%) or median [interquartile range].
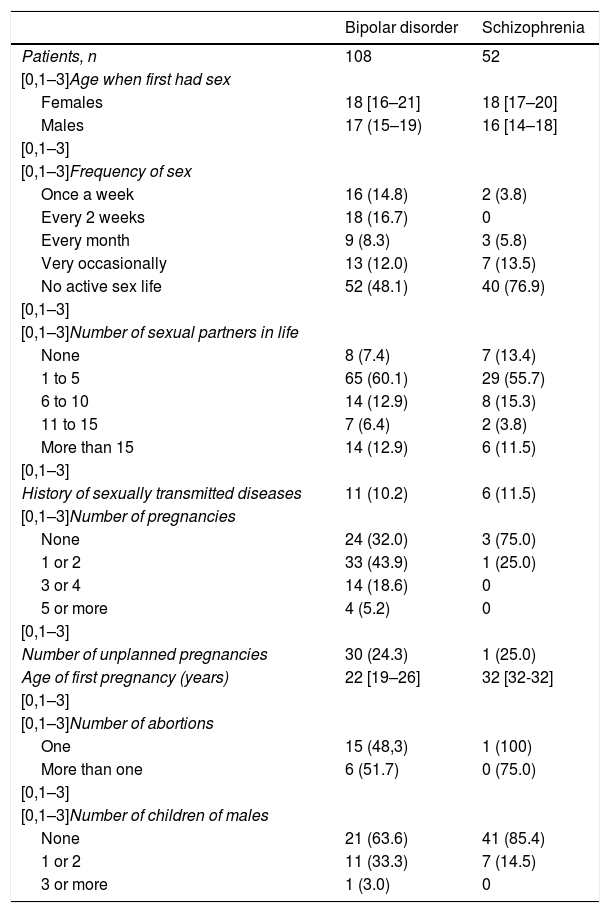
When investigating the sex life of participants, no significant differences were found with regard to the age at which they started having sex when comparing by diagnosis and by gender. The percentage of participants with schizophrenia who had never had sex was 13.4%, almost double that among those diagnosed with BD (7.4%). Between 55.7 and 60.1% had had at most five sex partners during their life and a little more than 10% said they had had more than 15 partners. Only 10.2 and 11.5% of the patients with BD and schizophrenia admitted having had a sexually transmitted disease during their lifetime. A total of 76.9% of the patients with schizophrenia and 48.1% of the patients with BD reported that they did not have an active sex life and, of those, 14.8% said they had sexual encounters at least once a week. 75% of women with schizophrenia and 32% of those with BD did not have children; 43.9% had one or two children, which in 24.3% of cases were unplanned pregnancies. The average age for the first pregnancy was 22, and in total there were 31 abortions. The number of children for men was small, most did not have any and only 33.3% of the patients with BD had at least one child (Table 2).
Variables related to sex life.
| Bipolar disorder | Schizophrenia | |
|---|---|---|
| Patients, n | 108 | 52 |
| [0,1–3]Age when first had sex | ||
| Females | 18 [16–21] | 18 [17–20] |
| Males | 17 (15–19) | 16 [14–18] |
| [0,1–3] | ||
| [0,1–3]Frequency of sex | ||
| Once a week | 16 (14.8) | 2 (3.8) |
| Every 2 weeks | 18 (16.7) | 0 |
| Every month | 9 (8.3) | 3 (5.8) |
| Very occasionally | 13 (12.0) | 7 (13.5) |
| No active sex life | 52 (48.1) | 40 (76.9) |
| [0,1–3] | ||
| [0,1–3]Number of sexual partners in life | ||
| None | 8 (7.4) | 7 (13.4) |
| 1 to 5 | 65 (60.1) | 29 (55.7) |
| 6 to 10 | 14 (12.9) | 8 (15.3) |
| 11 to 15 | 7 (6.4) | 2 (3.8) |
| More than 15 | 14 (12.9) | 6 (11.5) |
| [0,1–3] | ||
| History of sexually transmitted diseases | 11 (10.2) | 6 (11.5) |
| [0,1–3]Number of pregnancies | ||
| None | 24 (32.0) | 3 (75.0) |
| 1 or 2 | 33 (43.9) | 1 (25.0) |
| 3 or 4 | 14 (18.6) | 0 |
| 5 or more | 4 (5.2) | 0 |
| [0,1–3] | ||
| Number of unplanned pregnancies | 30 (24.3) | 1 (25.0) |
| Age of first pregnancy (years) | 22 [19–26] | 32 [32-32] |
| [0,1–3] | ||
| [0,1–3]Number of abortions | ||
| One | 15 (48,3) | 1 (100) |
| More than one | 6 (51.7) | 0 (75.0) |
| [0,1–3] | ||
| [0,1–3]Number of children of males | ||
| None | 21 (63.6) | 41 (85.4) |
| 1 or 2 | 11 (33.3) | 7 (14.5) |
| 3 or more | 1 (3.0) | 0 |
Unless otherwise specified, the values express n (%) or median [interquartile range].
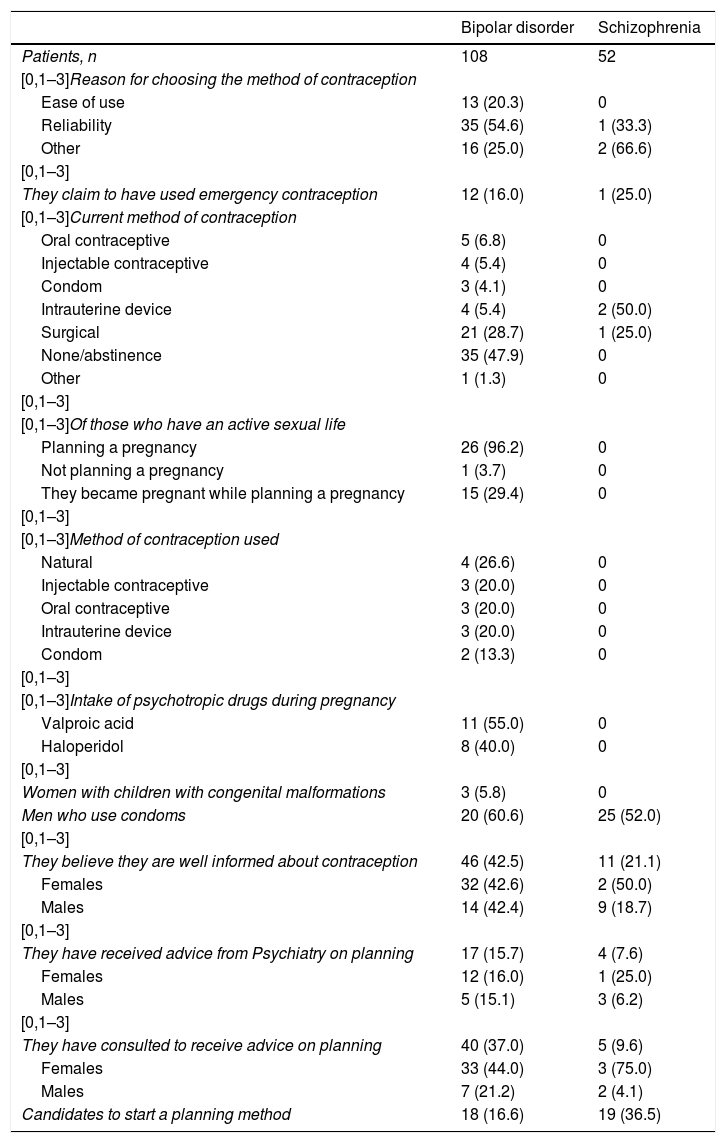
When asked about methods of contraception, almost all those who acknowledged having an active sex life said that they always used a method of contraception, and tubectomy was the most common among women. The main reasons for choosing these methods were reliability and ease of use. Of the BD group, only 48.8% of single women admitted planning the pregnancy, 12 said they had used a method of emergency contraception and 15 became pregnant while they were planning for a pregnancy; most of them were taking valproic acid during the pregnancy. There were only three cases of children with a congenital malformation, one associated with the intake of valproic acid and another with the intake of haloperidol. With regard to men, none had children with malformations and only 52.0% of the group of patients with schizophrenia and 60.6% of the group with BD claimed that they used condoms when having sex.
A total of 57.4% of the patients with BD and 78.8% of those who had schizophrenia considered that they were well informed about family planning, despite the fact that almost none and only a third of women with BD had asked for advice on it from trained personnel. The vast majority said they had never received information on the topic during their consultations with the psychiatrist, which is worrying as, according to this survey, a significant percentage of patients interviewed need to start a method of contraception (Table 3).
Variables related to the method of contraception.
| Bipolar disorder | Schizophrenia | |
|---|---|---|
| Patients, n | 108 | 52 |
| [0,1–3]Reason for choosing the method of contraception | ||
| Ease of use | 13 (20.3) | 0 |
| Reliability | 35 (54.6) | 1 (33.3) |
| Other | 16 (25.0) | 2 (66.6) |
| [0,1–3] | ||
| They claim to have used emergency contraception | 12 (16.0) | 1 (25.0) |
| [0,1–3]Current method of contraception | ||
| Oral contraceptive | 5 (6.8) | 0 |
| Injectable contraceptive | 4 (5.4) | 0 |
| Condom | 3 (4.1) | 0 |
| Intrauterine device | 4 (5.4) | 2 (50.0) |
| Surgical | 21 (28.7) | 1 (25.0) |
| None/abstinence | 35 (47.9) | 0 |
| Other | 1 (1.3) | 0 |
| [0,1–3] | ||
| [0,1–3]Of those who have an active sexual life | ||
| Planning a pregnancy | 26 (96.2) | 0 |
| Not planning a pregnancy | 1 (3.7) | 0 |
| They became pregnant while planning a pregnancy | 15 (29.4) | 0 |
| [0,1–3] | ||
| [0,1–3]Method of contraception used | ||
| Natural | 4 (26.6) | 0 |
| Injectable contraceptive | 3 (20.0) | 0 |
| Oral contraceptive | 3 (20.0) | 0 |
| Intrauterine device | 3 (20.0) | 0 |
| Condom | 2 (13.3) | 0 |
| [0,1–3] | ||
| [0,1–3]Intake of psychotropic drugs during pregnancy | ||
| Valproic acid | 11 (55.0) | 0 |
| Haloperidol | 8 (40.0) | 0 |
| [0,1–3] | ||
| Women with children with congenital malformations | 3 (5.8) | 0 |
| Men who use condoms | 20 (60.6) | 25 (52.0) |
| [0,1–3] | ||
| They believe they are well informed about contraception | 46 (42.5) | 11 (21.1) |
| Females | 32 (42.6) | 2 (50.0) |
| Males | 14 (42.4) | 9 (18.7) |
| [0,1–3] | ||
| They have received advice from Psychiatry on planning | 17 (15.7) | 4 (7.6) |
| Females | 12 (16.0) | 1 (25.0) |
| Males | 5 (15.1) | 3 (6.2) |
| [0,1–3] | ||
| They have consulted to receive advice on planning | 40 (37.0) | 5 (9.6) |
| Females | 33 (44.0) | 3 (75.0) |
| Males | 7 (21.2) | 2 (4.1) |
| Candidates to start a planning method | 18 (16.6) | 19 (36.5) |
Unless otherwise indicated, the values express n (%).
Like in this study, a low percentage of cohabiting or marriage among patients with schizophrenia is reported in the literature,5,28 while in those with BD, the average is below 41.1%, found by Magalhares et al.11 in this same population and it is similar to that found in people with MI in general,10 which would indicate that our patients with schizophrenia have a similar course to that reported in other countries, where the prematurity of the condition may be decisive with regard to the marital status of these individuals, while it is possible to achieve a greater premorbid functioning in BD as it appears later in the life cycle.
After analysing the work environment, up to 65.9% of the patients with BD are unemployed,11 a similar figure to that found in this study, while specific data on patients with schizophrenia were not found, only reports of studies carried out in people with this and other MI, which showed unemployment rates of 71.2,5 75.810 and 94.5%.16 It is worth stressing that our sample of patients, despite being part of a clinic for BD and psychosis, reveals that the provision of this health service with a view to comprehensive rehabilitation where patients can be guaranteed some sort of reintegration into work and where the living conditions of these subjects could be improved, is not talked about in our setting.
With regard to the age of starting to have sex, the result produced by this study coincides with that observed by other authors in patients with various MI, around the age of 1825,29 and, contrary to what many believe, it has been seen that most women with schizophrenia are sexually active,4 with rates that range from 5628 to 90%12; this can probably be explained because socially it is easier for a mentally ill woman to get a partner, as in our setting it is expected that it is the man who has a dominant role when selecting and starting life as a couple, which is why these female patients could have a more passive role in this process.
A study carried out in Brazil in 2475 patients with MI found that 24% had had a sexually transmitted disease,30 while in this study this percentage was reduced by half; however, under-reporting or difficulties in detecting these types of diseases cannot be ruled out.
The average age for the first pregnancy coincides with that found by Gomes et al.16 in women with MI, who stated that 47.7% were under the age of 19,16 with regard to unplanned pregnancies in the BD and schizophrenia groups. A study carried out in Turkey5 reported values of 50.5% and 47.5% respectively, which represents more than double that found in this study, while with regard to abortion rates (20.6 and 25%), the result was very similar. When talking about the parity of patients with BD, a Brazilian study reported that 22.1% did not have children and that 44.9% had one or two,11 results comparable to that of ours and others with women with MI (65.110 and 56.4%,16 respectively). The medical literature, like this report, claims that women with schizophrenia have fewer children.5 The similarity with Brazilian studies suggests that epidemiologically there may be similar behaviours in both countries, as it is the same region and due to the natural course of these mental disorders, as functionality could deteriorate as the condition progresses (including sexual and reproductive health) and the adverse sexual effects of medicines becomes more noticeable, among other individual factors.
The high proportion of women of childbearing age with a history of BD who said they were planning a pregnancy did not coincide with the results of other studies; 58.8%11 in a similar population and 13.7% of women with various MI.16 The most used method of contraception continues to be tubectomy (16.311 and 48.4%15). Of the four women with schizophrenia, none were planning a pregnancy. Despite the limited data on the frequency of the use of contraception in this population, very low percentages have been found.11 Probably due to the episodic nature of BD, in which one of the cardinal symptoms of manic episodes is increased impulsivity with high-risk behaviours and due to the teratogenicity of classic mood stabilisers, these patients reported a higher rate of the use of contraceptives than patients with schizophrenia in our sample.
Only a third of patients in the BD group said that they had received information on sexuality and contraception, which corresponds with that reported in studies carried out in Istanbul5 and New Zealand,5 while in another study conducted with women with schizophrenia, only 26.6% had undergone a gynaecological examination in the past three years, versus 56% of women in the control group.12 However, two of the four women in this study who had this diagnosis said they had received information about it, but it is not clear whether this information was provided directly by healthcare personnel or alternative means.
Some of the limitations of this study are its cross-sectional design, which does not allow for monitoring over time, the absence of a control group and the complexity of the patients enrolled, which means that the results obtained cannot be generalised. Furthermore, the reliability of the information is affected by the sensitivity of this topic, the impersonal nature of the telephone interview, possible memory errors, social stigma and embarrassment, among others.
ConclusionsA responsible sex and reproductive life requires appropriate cognitive and behavioural standards, which are altered in patients with MI. For this, psychiatrists, as part of the comprehensive care of their patients, should take the initiative and address this topic, to guarantee education regarding contraception, planning a pregnancy and risk of sexually transmitted diseases, among others, and therefore to ensure the safety and quality of life of their patients.
FundingThis original article did not receive funding from any entity.
Conflicts of interestNone.
Please cite this article as: Correa AMP, Carrillo RAA, Vega DCS, Cano SG, Arango LGA, Builes LFT, et al. Salud sexual y reproductiva de los pacientes con esquizofrenia y trastorno afectivo bipolar. Rev Colomb Psiquiat. 2020;49:15–22.