Medically unexplained symptoms are defined as physical symptoms that have been present for several weeks and that an adequate medical evaluation has not revealed any disease that explains them; when these symptoms become persistent, they lead to comprehensive clinical investigations and multiple interventions. These patients have a greater or at least comparable commitment to physical functioning, mental health, and negative health perception than patients with multiple chronic medical conditions; have significantly more stressful life events (psychological, physical and/or sexual abuse) and are more likely to meet diagnostic criteria for anxiety and depression.
ObjectiveTo characterise sociodemographic and psychiatric characteristics of a group of patients identified in primary care with medically unexplained symptoms.
MethodologyA descriptive, cross-sectional study with patients from 18 to 70 years old who were given PHQ-15, PHQ-9 and PHQ for anxiety, and a survey designed for the study.
Results36 patients were analysed, 94.4% women, median age 45 [RIC, 20] years-old, 33.3% married, 91.7% had children. 55% had severe functional somatic symptoms, 77.8% had one or more functional somatic disorders, and 77.7% had clinically relevant affective or anxiety symptoms. 25% of the patients reported a history of child abuse, 41.7% were mistreated by a partner, and 41.6% were victims of the Colombian armed conflict.
ConclusionsThe main finding of this study was that 8 out of 10 patients met criteria for a functional somatic disorder with great symptomatic severity and three out of ten patients met criteria for two functional disorders, most of these patients without other basic medical diseases. In addition, we found a high prevalence of exposure to different types of violence that these patients have been subjected to throughout their life.
Se define como síntoma médicamente inexplicado los síntomas físicos de varias semanas de duración cuya adecuada evaluación médica no revele alguna enfermedad que los explique; cuando estos síntomas se tornan persistentes, llevan a exploraciones clínicas exhaustivas y múltiples intervenciones. Estos pacientes tienen un deterioro mayor, o al menos comparable en cuanto a funcionamiento físico, salud mental y percepción negativa de su salud, que los pacientes con múltiples enfermedades médicas crónicas; tienen significativamente más eventos estresantes vitales (abuso psicológico, físico y/o sexual) y más probabilidades de cumplir criterios diagnósticos de ansiedad y depresión.
ObjetivoCaracterizar sociodemográfica y psiquiátricamente un grupo de pacientes identificados en atención primaria con síntomas médicamente inexplicados.
MétodosEstudio descriptivo transversal de pacientes de 18-70 años, a quienes se aplicó el PHQ-15, el PHQ-9 y el PHQ para ansiedad y una encuesta diseña para la investigación.
ResultadosSe analizó a 36 pacientes, el 94,4% mujeres, con una mediana de edad de 45 [20] años; el 33,3% de ellas estaban casadas y el 91,7% tenía hijos. El 55% tenía síntomas somáticos funcionales graves, el 77,8% tenía 1 o más trastornos somáticos funcionales y el 77,7% presentaba síntomas afectivos o ansiosos de relevancia clínica. El 25% de los pacientes reportaron antecedente de maltrato en la infancia; el 41,7%, maltrato de pareja, y el 41,6% había sido víctima del conflicto armado colombiano.
ConclusionesEl principal hallazgo de este estudio fue que cerca de 8 de cada 10 pacientes cumplían criterios de un trastorno somático funcional con gran intensidad sintomática, y cerca de 3 de cada 10 pacientes cumplían criterios de 2 trastornos funcionales, la mayoría de estos pacientes sin otras enfermedades médicas de base. Además, en estos pacientes se encontró alta prevalencia de exposición a diferentes tipos de violencia a lo largo de la vida.
Medically unexplained symptoms are defined as physical symptoms that have been present for several weeks, where an adequate medical evaluation has not revealed any disease that explains them.1,2 The symptoms are often presented in primary care (corresponding to approximately 50% of consultations).2–4 Many patients present a single somatic symptom, such as headaches, lumbago or nausea. Others present a functional syndrome characterised by a constellation of somatic symptoms, such as irritable bowel syndrome or fibromyalgia.5
Most medically unexplained symptoms are transitory and self-limiting, but when they become persistent, they lead to comprehensive clinical investigations that entail repeated visits to the primary care doctor, multiple remissions, an increase in the performance and repetition of diagnostic tests (including invasive procedures) and an increase in costly treatments and prolonged hospital stays.2,6
Patients with extensive somatisation have a greater or at least comparable deterioration in terms of physical functioning, mental health and negative health perception than patients with multiple chronic medical conditions.6 These patients are primarily young adults,4 women2–4 and those with a low level of education2 and have significantly more stressful life events (psychological, physical and/or sexual abuse)2,7 and are more likely to meet diagnostic criteria for anxiety and depression.2,4,7
The objective of this study was to characterise a group of patients with medically unexplained symptoms in a primary care setting in Medellín, Colombia.
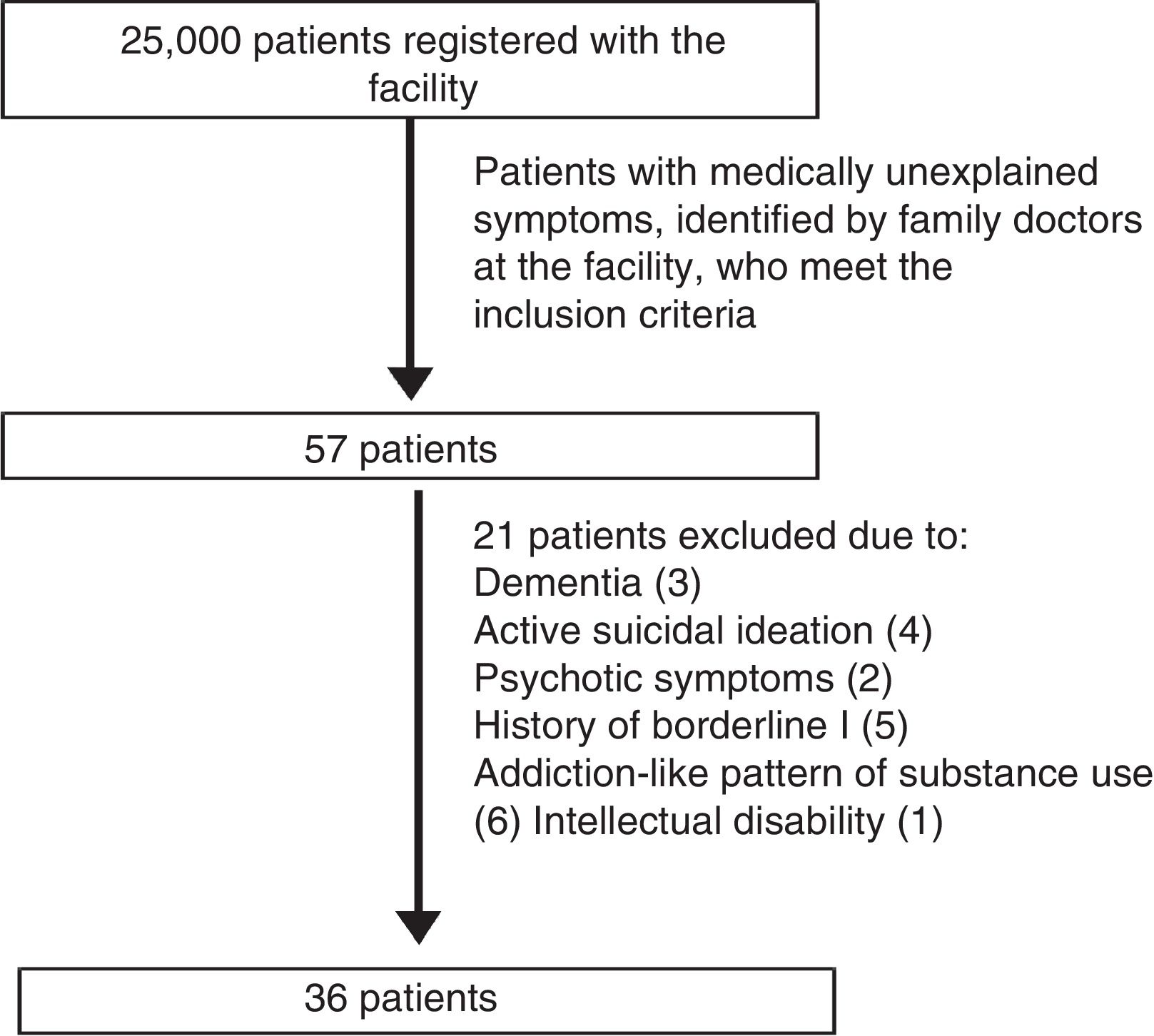
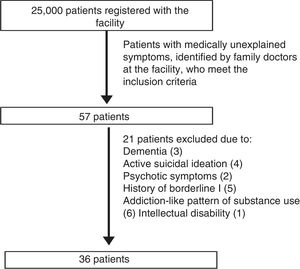
MethodsA descriptive, cross-sectional study in a reference population of 25,000 adults registered with a primary care facility in the city of Medellín, which uses the family health system, wherein family doctors know the family groups allocated to them well; members of the family group are cared for in the event of illness and through various promotion and preventive services; if they need specialised assessments or studies, patients are referred and the family doctor is always kept informed of what is happening with the patient.
The study population is made up of those patients with medical symptoms without adequate medical explanation according to the primary care staff of said facility. Sample selection was non-probabilistic, being based on the patients identified over the 20 months of sample collection who agreed to participate. The inclusion criteria were: literate native Spanish speakers between 18 and 70 years of age. The exclusion criteria were: presence of confusional symptoms compatible with dementia and/or delirium, presence of psychotic symptoms, active suicidal ideation, history of moderate to severe intellectual disability, history of schizophrenia, history of bipolar II disorder, addiction-like pattern of alcohol use and addiction like-pattern of use of illegal substances. During follow-up, no patient received a new clinical diagnosis that fully or partially explained the “medically unexplained” symptoms (Fig. 1).
The variables included were: age, gender, education, marital status, place of residence, employment, religion, number of children, questions relating to depression, anxiety, functional somatic symptoms and life events. The survey was self-administered and consisted of 42 questions.
Measuring instrumentsThe Patient Health Questionnaire (PHQ) is a diagnostic tool for mental health disorders used by health professional who require short and simple instruments for patients. It is based on the PRIME-MD interview developed by Spitzer et al.,8 and aims to screen for 12 mental health disorders. The same authors later developed the PHQ. The PHQ is a self-administered version of the PRIME-MD and includes the modules for depression, anxiety, alcohol, somatic symptom disorders and eating disorders from the PRIME-MD. Each question is scored from zero to two. The overall score is obtained by adding together the subscales.
PHQ-9The PHQ-9 is a self-administered subscale derived from the PHQ, which screens for major depression with a sensitivity of 92% and specificity of 89% and is validated in Spanish for Chile, Argentina and Colombia.9–11 It consists of nine items that assess the presence of depressive symptoms (corresponding to the DSM-IV criteria) in the last two weeks.12
PHQ-15The PHQ-15 subscale screens for 15 somatic symptoms that occur in around 90% of physical symptoms commonly reported by patients attending consultations.8,13 It is a validated tool that has been used in more than 40 studies in various countries and cultures14; it is validated in Spanish13. The PHQ-15 score is between 0 and 30 points, classifying somatic symptoms as: minimal (0–4), mild (5–9), moderate (10–14) and severe (15–30).13 The sensitivity and specificity of the PHQ-15 in primary care are 78% and 71%, respectively.15
GAD-7The GAD-7 subscale was developed to diagnose generalised anxiety and has been validated in 2740 patients in primary care. It has a sensitivity of 89% and a specificity of 82%. It screens for three anxiety diagnoses: panic disorder (sensitivity: 74%; specificity: 81%), social anxiety (sensitivity: 72%; specificity: 80%) and post-traumatic stress (sensitivity: 66%; specificity: 81%). It contains seven questions scored from zero to three (never, some days and almost all days, respectively) with an overall score between 0 and 21. The cut-off points for anxiety symptoms are 5 (mild), 10 (moderate) and 15 (severe).16,17
A pilot study was conducted in four patients to determine the time required to complete each survey and to ensure that the language of the questions was straightforward. To minimise possible information biases, it was verified that the survey was completed in full and each participant was given assistance with doubts that arose while completing it. Patient privacy while responding to the survey was ensured by asking accompanying persons to leave while they completed it. An epidemiologist with experience handling such information reviewed the database.
Descriptive analyses were carried out for the sociodemographic variables, tests of normality were performed for age, and measures of summary and dispersion were obtained. The SPSS® version 21.0 software package (SPSS Inc., Chicago, Illinois, USA) was used with a licence to analyse the data. This research is classified as “without risk” under article 11 of Resolution 008430 of 1993. Written informed consent was requested from the participants. The confidentiality of the information analysed was guaranteed at all times.
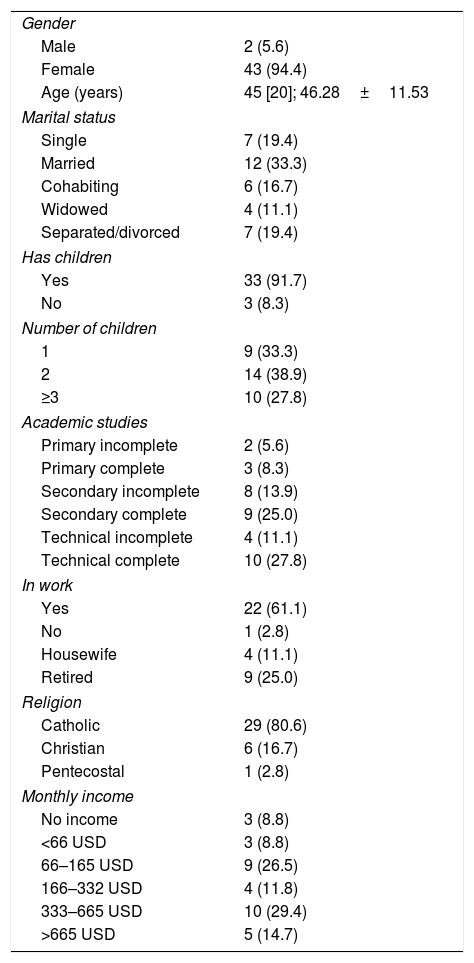
ResultsThirty-six patients were included. The majority were women (94.4%). The mean age was 45 [20] years. The majority were married (33.3%) and had children (91.7%), technical education (27.8%) and were in work (61.1%) (Table 1).
Sociodemographic characteristics of the study population.
| Gender | |
| Male | 2 (5.6) |
| Female | 43 (94.4) |
| Age (years) | 45 [20]; 46.28±11.53 |
| Marital status | |
| Single | 7 (19.4) |
| Married | 12 (33.3) |
| Cohabiting | 6 (16.7) |
| Widowed | 4 (11.1) |
| Separated/divorced | 7 (19.4) |
| Has children | |
| Yes | 33 (91.7) |
| No | 3 (8.3) |
| Number of children | |
| 1 | 9 (33.3) |
| 2 | 14 (38.9) |
| ≥3 | 10 (27.8) |
| Academic studies | |
| Primary incomplete | 2 (5.6) |
| Primary complete | 3 (8.3) |
| Secondary incomplete | 8 (13.9) |
| Secondary complete | 9 (25.0) |
| Technical incomplete | 4 (11.1) |
| Technical complete | 10 (27.8) |
| In work | |
| Yes | 22 (61.1) |
| No | 1 (2.8) |
| Housewife | 4 (11.1) |
| Retired | 9 (25.0) |
| Religion | |
| Catholic | 29 (80.6) |
| Christian | 6 (16.7) |
| Pentecostal | 1 (2.8) |
| Monthly income | |
| No income | 3 (8.8) |
| <66 USD | 3 (8.8) |
| 66–165 USD | 9 (26.5) |
| 166–332 USD | 4 (11.8) |
| 333–665 USD | 10 (29.4) |
| >665 USD | 5 (14.7) |
Vales expressed as n (%); median [interquartile range]; mean±standard deviation.
Some 61% of the patients had no diagnosed medical condition. Of the patients with underlying conditions, 27.8% had dyslipidaemia; 13.9% type 2 diabetes mellitus and thyroid problems; 8.3% lung problems; 5.6% hypertension and 2.8% chronic kidney disease. No patient had cardiovascular or rheumatic diseases, cancer or HIV infection.
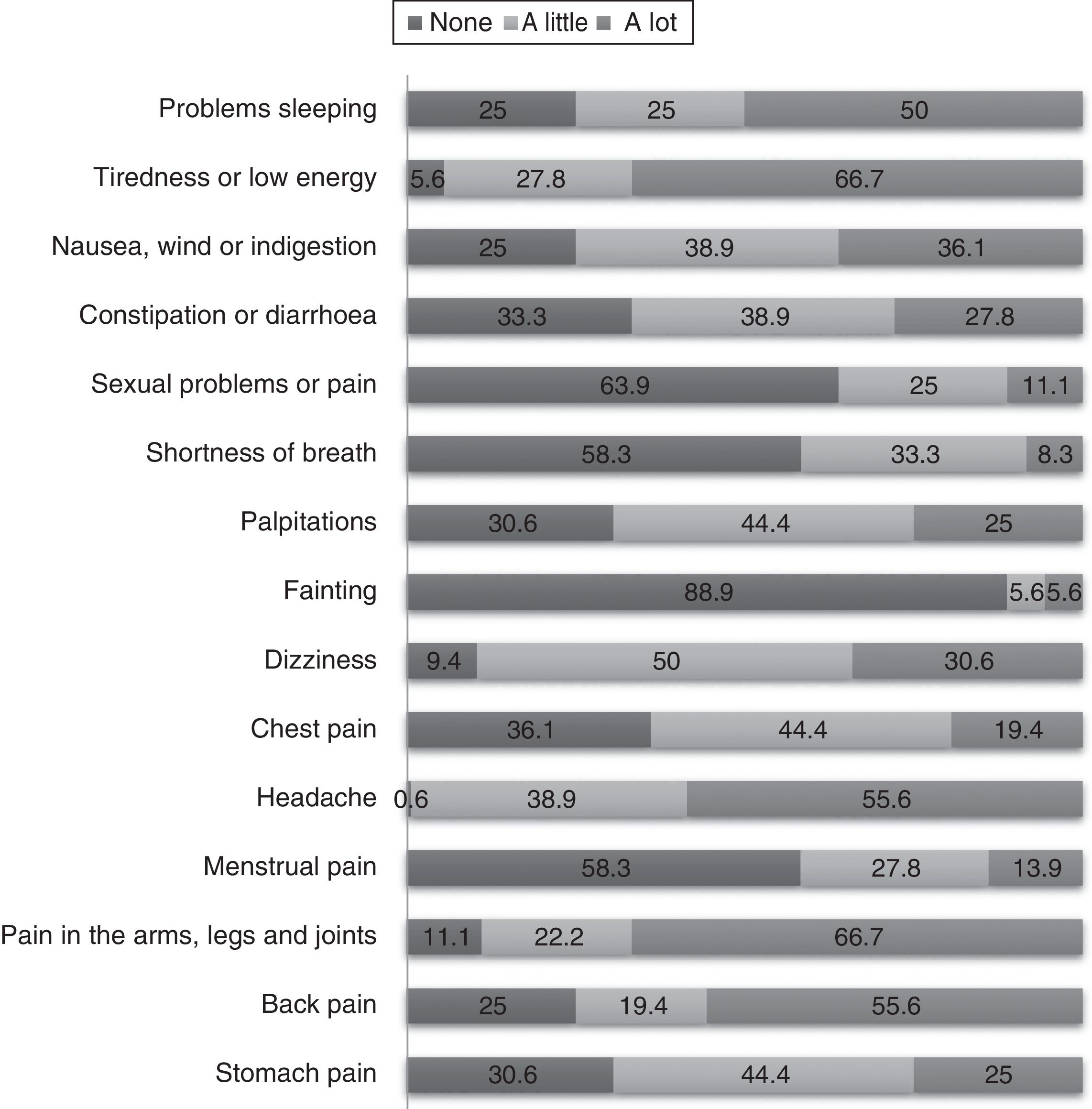
Somatic symptomsThe patients were questioned about 15 somatic symptoms and asked to rate them according to the intensity of the symptom, as never, a little or a lot, using the PHQ-15 scale. The symptoms with greatest somatic intensity were tiredness and low energy (66.7%), pain in the arms, legs and joints (66.7%), headache and back pain (55.6%) and problems sleeping (50.0%), among others (Fig. 2).
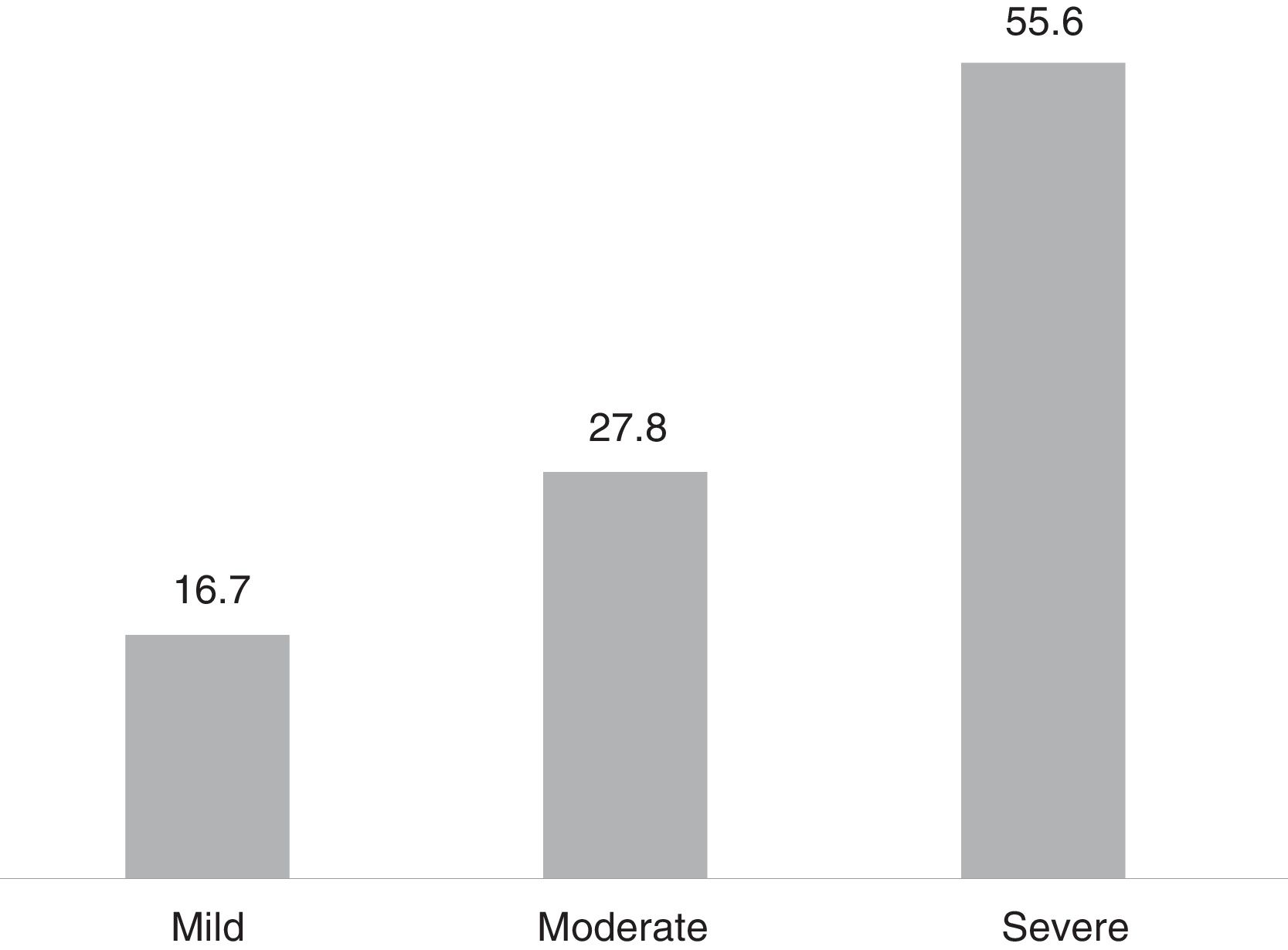
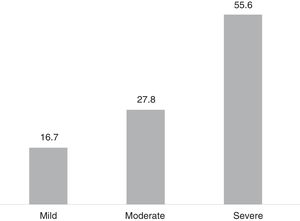
For most patients (55.0%), the symptoms were severe according to the PHQ-15 scale (Fig. 3).
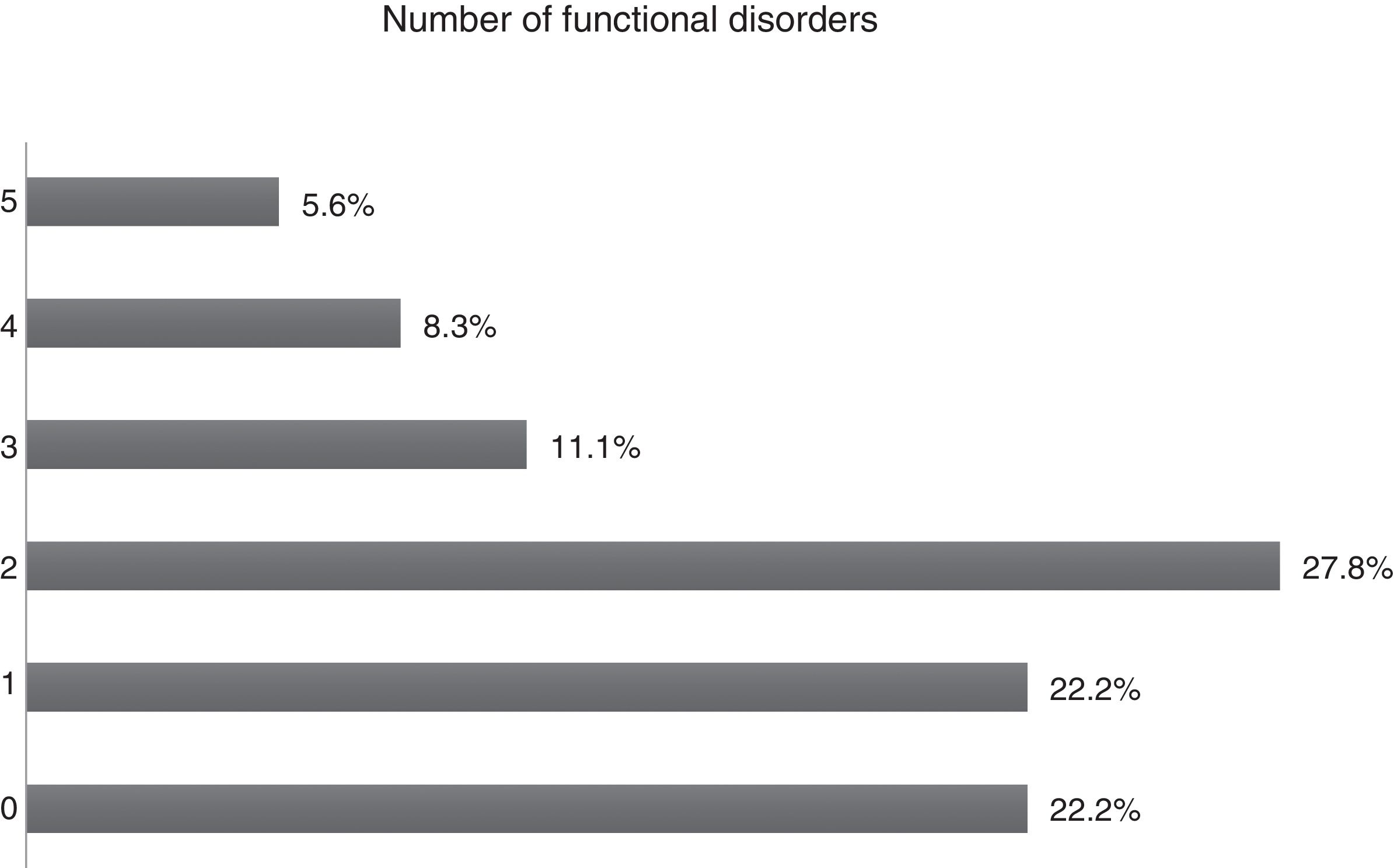
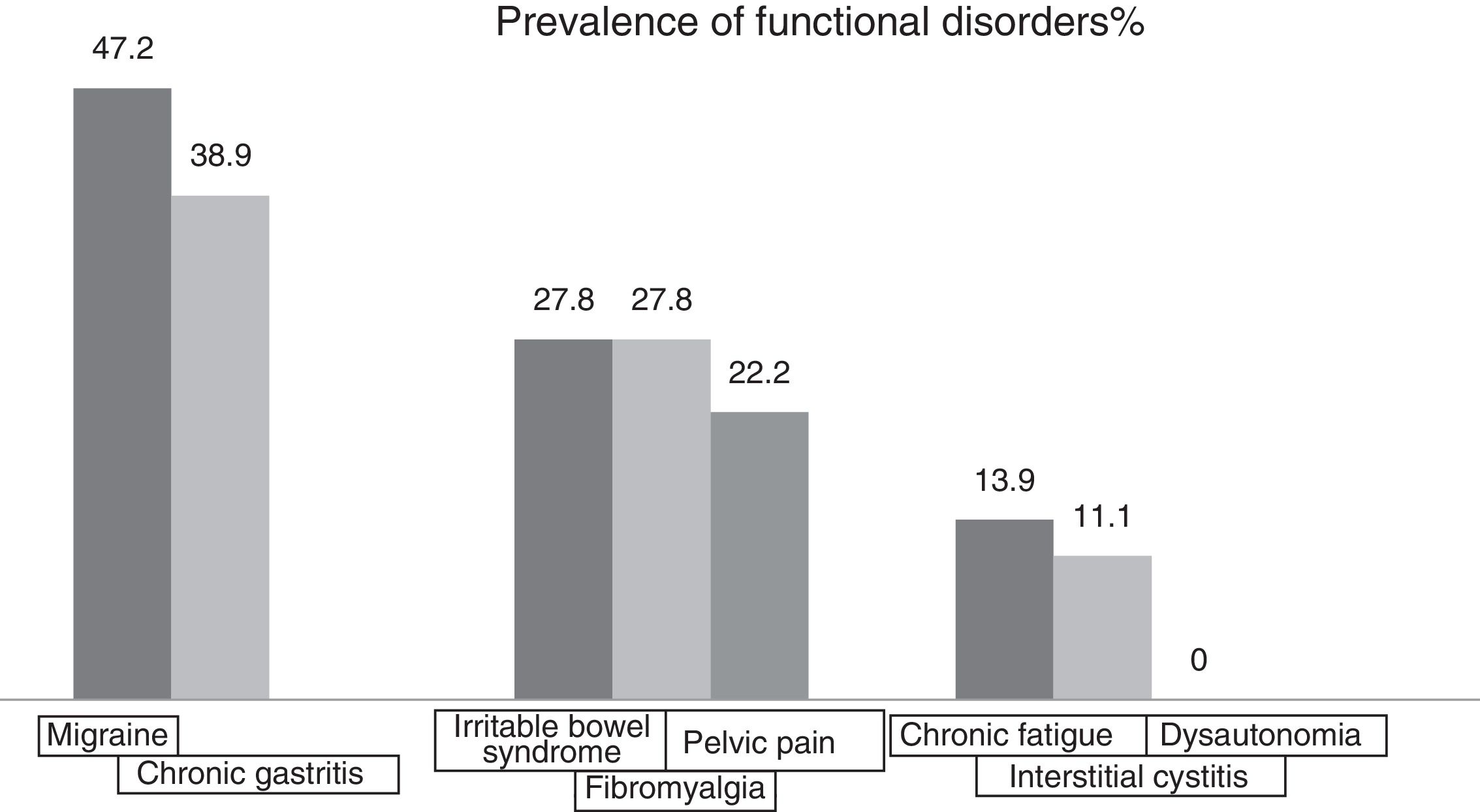
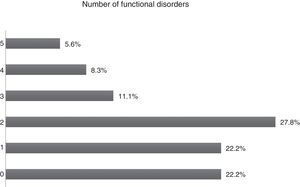
Functional disorderFunctional disorders were present in 77.8% of patients. Regarding the number of functional disorders, 27.8% stated that they had two disorders and 22.2% only one disorder; 22.2% said they had no functional disorders (Fig. 4).
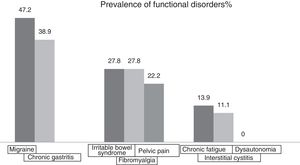
The most prevalent functional disorders were migraine (47.2%) and gastritis (38.9%). No patient had dysautonomia (Fig. 5).
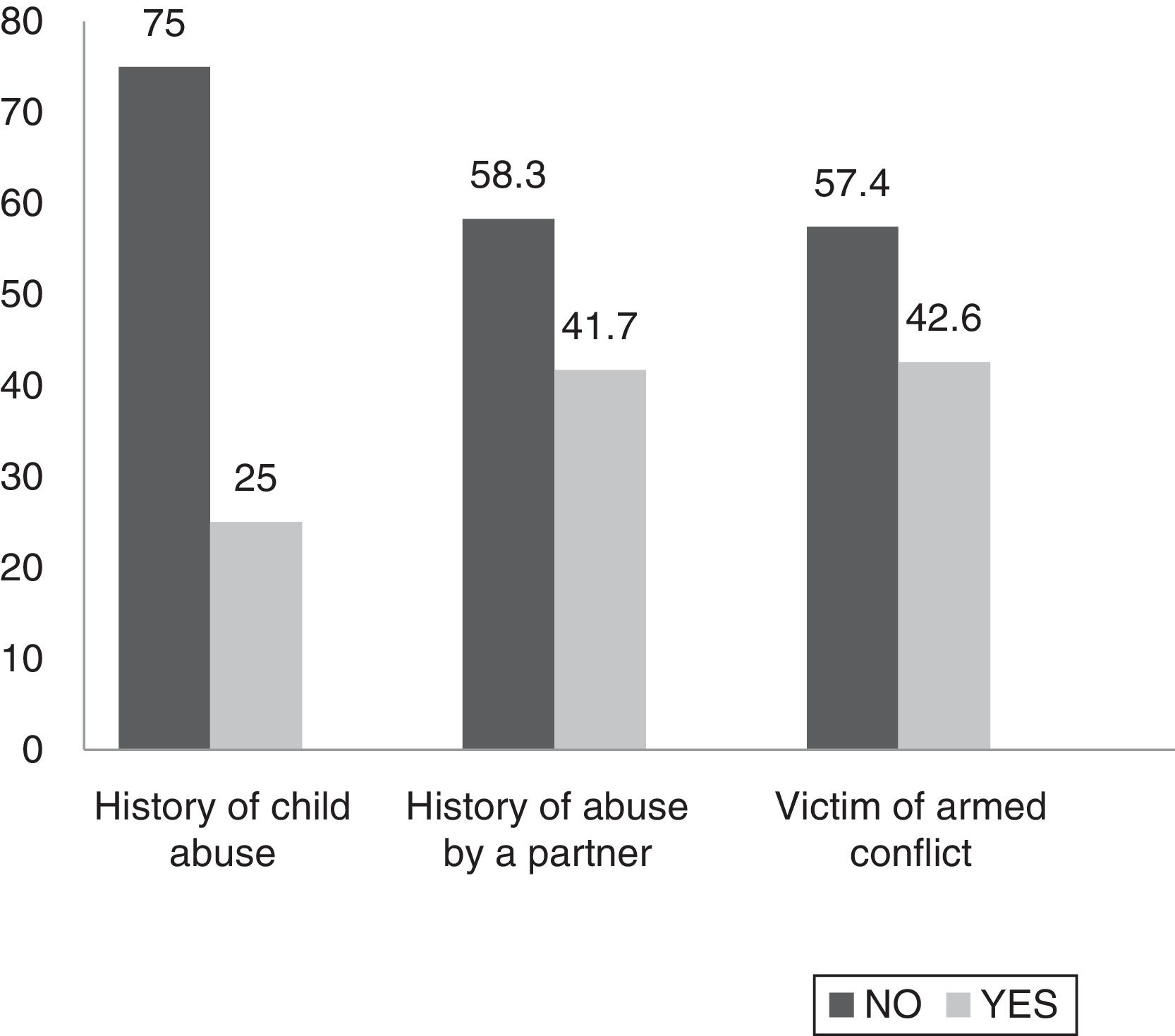
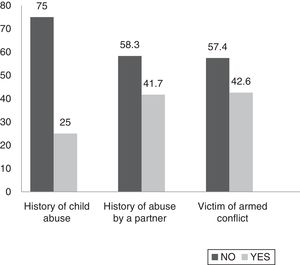
History of child abuse and other types of violence throughout lifeSome 25% of patients admitted having been victims of abuse in childhood. This child abuse was psychological in nature in 100% of cases, physical in 88.8% and sexual in 33.3% (Fig. 5). 41.7% stated that they had been abused by a partner. This abuse was psychological in 100% of cases, physical in 80% and sexual in 20% of cases. Regarding domestic violence, 38.9% stated that they had suffered it and 44.4% of patients stated that a relative living with them consumed psychoactive substances such as alcohol and drugs. Regarding the armed conflict in Colombia, 19.4% stated that they had been a direct victim, 22.2% had been indirect victims and 58.3% had not been victims (Fig. 6).
Depressive, anxiety and panic-related symptoms according to the PHQ scaleThe PHQ scale was used for depressive symptoms and symptoms of anxiety and panic, revealing that 30.6% had depressive symptoms, 36.1% symptoms of panic and 33.3% symptoms of anxiety.
DiscussionThis study sociodemographically and clinically characterises 36 patients identified in primary care with medically unexplained symptoms. The principal finding of this study is that around 8 out of 10 patients meet criteria for a functional somatic disorder with high symptom intensity, and around 3 out of 10 meet criteria for two functional disorders; most of these patients had no other underlying medical conditions. According to Kroenke,18 a quarter of patients with medically unexplained symptoms suffer from severe somatic symptoms and between half and two-thirds have two or more functional disorders, which is in keeping with our findings.
The other very important finding is the high prevalence of different types of violence to which these patients have been subjected throughout their lives. Numerous studies in recent decades5,7,19–31 have signalled traumatic events as an important factor associated with the presence of medically unexplained symptoms; however, most of these studies have focussed almost exclusively on child sex abuse. In our study, the “traumatic” context was expanded to include three of the four forms of child abuse (psychological, physical and sexual), abuse by a partner, domestic violence and armed conflict. All of these forms of violence were present in a high proportion in the patients, expanding the range of traumatic events in the context of medically unexplained symptoms.
Different prevalences of child abuse have been reported in patients with somatisation. In one study, Morrison30 found that 55% of patients with somatisation reported having experienced sexual abuse prior to 18 years of age. The figures for medically unexplained symptoms in patients who have been victims of child sex abuse are not yet clear from the literature.
Abuse by a partner, which can include physical, emotional, sexual and financial abuse as well as control of contraception or pregnancy, more often affects women32; however, the literature does not specify its association with medically unexplained symptoms.
With regard to the patients’ gender, we found a higher proportion of women than that reported by other authors. Steinbrecher et al.4 had a proportion of 7/10, whereas in our study it was 9/10.
The level of education of these patients—often low according to previous studies2—differs from that found in our study, which fell between completed technical studies and lower secondary education, higher than the national average, as only 3.9% of the population has technical qualifications.33
Finally, with regard to demographics, a higher proportion of young patients has been reported.4 This also differs from our results, which found a group of adults up to 65 years of age.
Regarding emotional symptoms and symptoms of anxiety, 77.7% of patients with medically unexplained symptoms presented clinically relevant emotional and anxiety symptoms; this association has been described in a number of studies, with prevalences varying depending on the method used.4,3,34–36 In our study, one in every three patients had clinically significant depressive symptoms or symptoms of anxiety or panic. This finding is particularly important at it indicates that, although there is significant comorbidity between emotional and anxiety symptoms and medically unexplained symptoms, the latter are not a somatic manifestation of the former, as would be the case in masked depression.34,36
This study has the following limitations: (a) given its cross-sectional methodology, it is not possible to consider a causal relationship between the variables studied and the presence of medically unexplained symptoms; (b) the results are based on a survey and may be influenced by possible memory biases; (c) given the sensitive nature of the questions, it is possible that the participants did not provide reliable information; (d) the number of patients was small and they were selected based on convenience, which limits generalisation of the results; and (e) the instruments used to screen for psychological symptoms in this study allowed specific psychological symptoms to be screened for with a certain level of sensitivity and specificity, whereas the reference standard for psychiatric diagnosis is the structured psychiatric interview, which must be taken into account by the reader.
In spite of these limitations, this study offers valuable information on medically unexplained symptoms in the context of primary care. Moreover, it is our opinion that this study can be used to generate hypotheses for future studies exploring other types of violence in patients with medically unexplained symptoms, especially in the primary care setting, which is where these patients frequently seek care.
In conclusion, this study establishes that patients with medically unexplained symptoms have significant psychosocial and mental health situations that can be closely linked to the medically unexplained symptoms; because of this, the traditional medical approach of primary care, wherein psychosocial aspects are of little interest, can fall short. An understanding of each patient as a whole and indivisible person can therefore be useful in light of such symptoms.
Ethical disclosuresProtection of people and animalsThe authors state that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and to the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mejía-Rodríguez D, Rodríguez R, Restrepo D. Caracterización sociodemográfica y clínica psiquiátrica de pacientes con síntomas médicamente inexplicables en una institución prestadora de salud de Medellín (Colombia). Rev Colomb Psiquiat. 2019;48:72–79.