The COVID-19 pandemic has represented an extraordinary challenge for health workers as they care for others while exposing themselves to contagion. Doctors, nurses, therapists and other non-care staff in clinics and hospitals are asked to be prepared to work in particularly complex and stressful situations, which makes them vulnerable to mental health problems.
ObjectiveTo determine the prevalence and clinical characteristics of anxiety and depression symptoms in staff working at a health institution in Medellin, Colombia.
MethodsObservational, descriptive and cross-sectional study, based on a survey designed for the investigation, which included two scales to screen depression and anxiety symptoms, as well as sociodemographic variables.
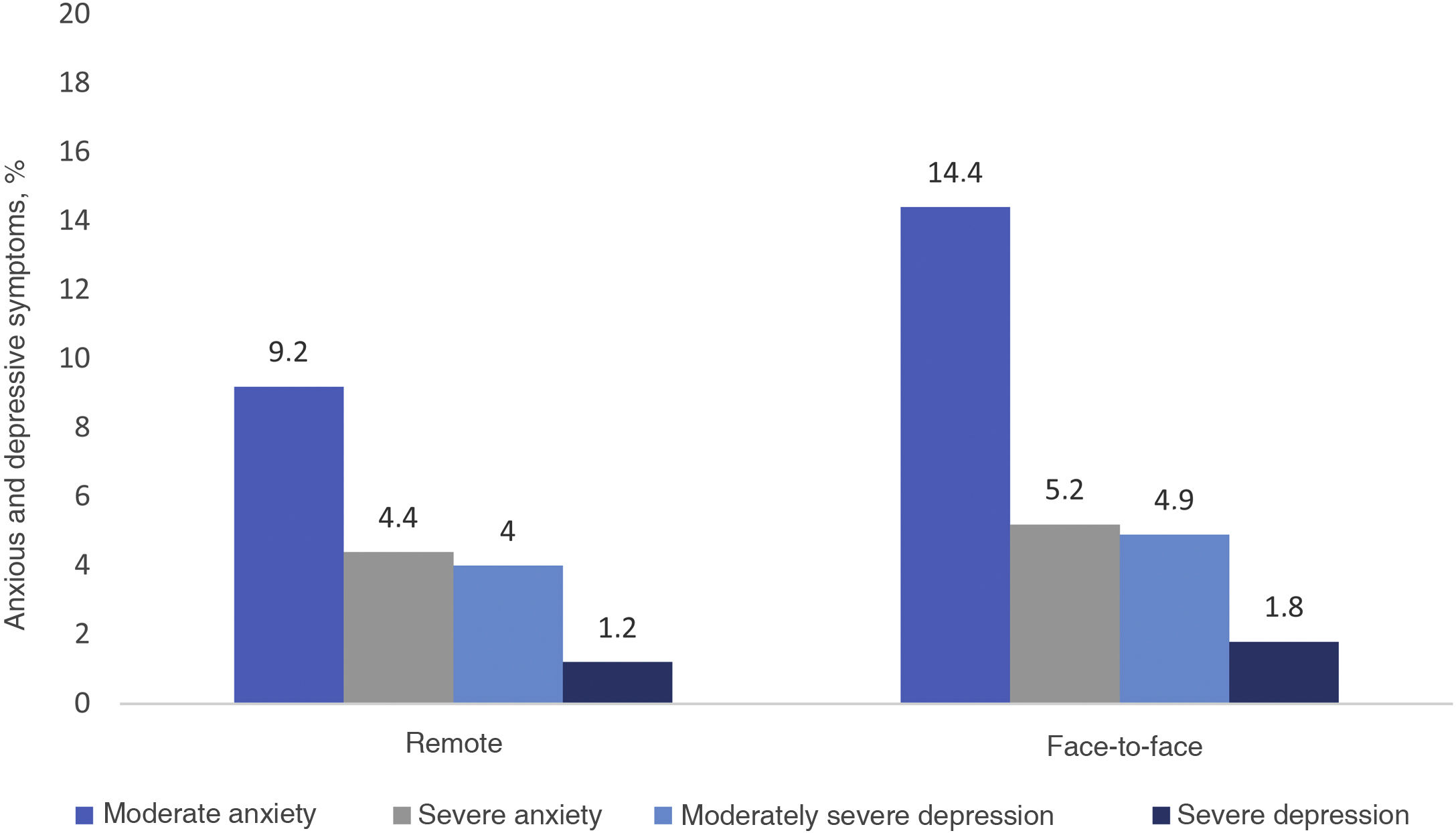
ResultsA total of 1,247 workers from the health institution were included. Of these, 14.6% reported symptoms of depression and 18.5% of clinically significant anxiety. A higher proportion of moderate to severe depression and anxiety symptoms was found in those working face to face.
ConclusionsAnxiety and depression symptoms are highly prevalent among staff at a health institution in Medellin, Colombia, during the COVID-19 pandemic. Given the vital role of the health sector in times of pandemic, the development of mental health programmes that address the problems of this population should be considered a priority.
Afrontar las circunstancias de la vida y el trabajo que la pandemia por COVID-19 ha impuesto al personal sanitario implica un reto extraordinario: cuidar y atender a otros, exponiéndose a sí mismos al contagio. A médicos, enfermeras, terapeutas y demás personal asistencial y no asistencial en clínicas y hospitales, se les pide estar preparados para trabajar en situaciones extraordinariamente complejas y estresantes, lo que los hace vulnerables a problemas mentales.
ObjetivoDeterminar la prevalencia y las características clínicas de los síntomas ansiosos y depresivos del personal que trabaja en una institución de salud en Medellín, Colombia.
MétodosEstudio observacional, descriptivo y transversal, a partir de una encuesta diseñada al efecto, la cual incluyó 2 escalas para tamizar síntomas depresivos y ansiosos, además de variables sociodemográficas.
ResultadosSe incluyó a 1.247 trabajadores de la institución de salud. El 14,6% reportó síntomas depresivos y el 18,5%, ansiosos clínicamente significativos. Se encontró una mayor proporción de síntomas depresivos y ansiosos moderados-graves en la modalidad de trabajo presencial.
ConclusionesLos síntomas ansiosos y depresivos son muy prevalentes entre los trabajadores de una institución de salud de Medellín durante la pandemia de COVID-19. Dado el papel vital del sector salud en tiempos de pandemia, el desarrollo de programas de salud mental que aborden los problemas de esta población debería considerarse una prioridad.
On 30 January 2020, the World Health Organization (WHO) declared a global state of emergency due to the emergence of a new strain of coronavirus, SARS-CoV-2,1 which was reported a month earlier in Wuhan, China, after an outbreak of pneumonia.2 By and large, every person's life has been affected in various ways, on all continents, in all countries and all socioeconomic groups.
More than six months after the first reported case, there is still no vaccine or specific treatment for COVID-19 and no end in sight to the spread of the disease.3 The implementation of prolonged lockdowns, physical distancing and other public health strategies aimed at reducing the rate of contagion appear to have a negative impact on the mental health of an important population group.4
From this perspective, health personnel face an extraordinary challenge: caring for others whilst exposing themselves to contagion. Doctors, nurses, therapists and other healthcare and non-healthcare personnel in clinics and hospitals are required to be prepared to work in extraordinarily complex situations of permanent exposure to COVID-19.5–7 Thus, health personnel seem to be the group that is most exposed to the psychological challenges of a new normal. This psychological burden is likely due to staff reorganisation, increased work intensity, and the anxiety of being exposed to the virus in hospital and, in turn, bringing the infection home.8
Shortly after the pandemic was declared, studies began to be published reporting high levels of stress in health personnel, now called "the first line" of care, which has been reflected in a higher prevalence of insomnia and anxious and depressive symptoms, in addition to a probable increase in suicide rates in this population.5,9 Continuing research on this topic makes it possible to generate information that helps to strengthen the response capacity of health systems, in addition to monitoring and positively influencing the mental health fatalities of health workers.10 The objective of this study is to determine the prevalence and clinical characteristics of depressive and anxious symptoms in the workers of a health institution in Medellín, Colombia.
MethodsA descriptive, observational and cross-sectional study was conducted. Auna is a regional health group with nearly 6,000 employees, which has a network of clinics and medical centres in Peru and Colombia.11 The Clínica Las Américas Auna is a health institution located in Medellín with 304 beds to provide care for children and adults who require emergency services, hospitalisation and intensive care for patients with highly complex medical and surgical diseases.
Since the declaration of the COVID-19 pandemic,12 the mental health area of Clínica Las Américas Auna wanted to align its efforts with the proposals made by the New Health Foundation (a non-profit institution for the observation and optimisation of health systems)13 to strengthen, support and act for health personnel in times of crisis.
This programme included: (a) training on precautions to take to prevent the spread of the coronavirus and emotional regulation techniques; (b) identification of people with anxious and depressive symptoms of clinical importance, who are offered individual intervention by psychology and psychiatry, and (c) short acupuncture sessions and active guidelines to promote well-being.
ParticipantsThe 2,100 employees of the institution in the healthcare and administrative areas were invited to participate in the study. Between 1 March and 31 May 2020, the Communications Department motivated participation in the study through the different internal communication channels such as the intranet, billboards, word-of-mouth, work group leaders and the email of each employee. The survey was available for eight weeks, the time that the sample collection lasted, and 1,247 employees took the surveys and agreed to participate in the study. There was one inclusion criterion: being an employee of the institution during the sample collection time. Those who did not give their informed consent were excluded.
VariablesSociodemographic variables were included: age, sex, job —healthcare, administrative—, work modality —face-to-face, teleworking— and psychiatric symptoms: nine depressive symptoms, seven anxious symptoms and scores from the Patient Health Questionnaire-9 (PHQ-9) and Generalised Anxiety Disorder (GAD-7) scales.
Data sourcesThe information was collected from a survey designed by the researchers for this study, which included 22 questions with Likert-type response options that were easy to understand and answer. It took 10−15 min to complete. No pilot test was carried out.
Instruments usedThis study employed two psychometric scales available for free use to apply to the Colombian population14: the PHQ-9 and the GAD-7. The PHQ-9 consists of nine Likert-type questions with answers scoring between zero and three points. Possible scores range from zero to 27. Cut-off points five, 10, 15, and 20 are for mild, moderate, moderately severe, and severe depression. With a cut-off point >10, there is a sensitivity of 88% and a specificity of 88%.15 The GAD-7 consists of seven Likert-type questions with answers scoring between zero and three points. Possible scores range from zero to 21. The proposed cut-off points of five, 10, and 15 are for mild, moderate, and severe symptoms, and clinical evaluation is recommended with scores >10. With these cut-off points, the scale has a sensitivity of 89% and a specificity of 82%.16 Both questionnaires are validated in Spanish.17–19
BiasesThe researchers took into account the following biases: (a) selection bias; a broad campaign was carried out to disseminate the research through the institution's communication channels and each person was given numerous opportunities to participate in the study; (b) information bias; the data was anonymised and only processed by the researchers, guaranteeing privacy and use of the information for strictly clinical and research purposes; in addition, validated instruments were used, which explored mental symptoms that occurred in the prior two weeks, which reduces recall bias, and (c) confounding bias; the scope of the study is descriptive, so its objective is not to search for associations. However, other variables that classify the cause or origin of the reported anxious and depressive symptoms according to the respondent were not included.
Sample sizeThe sample size was 1,247 individuals. The number of people who responded to the survey during the study period determined the sample size, so it is a non-probabilistic, non-representative sample, in which not all individuals had the same probability of being chosen.
Analysis of the informationThe information was analysed with the SPSS statistical software version 21 (SPSS Inc.; United States), licensed. The qualitative variables are presented as absolute and relative frequencies. The quantitative variables are presented as mean ± standard deviation, and median [interquartile range], based on assumptions of normality (Shapiro–Wilk test). Analysis was conducted by subgroups of age, sex and occupation using the Pearson or Fisher χ2 statistic, assuming significant differences from p < 0.05. The prevalence of clinically significant depressive (PHQ-9 > 10) and anxious (GAD-7 > 5) symptoms was determined. All surveys were fully completed, so there were no missing data.
Ethical considerationsThis investigation was approved by the Institutional Research Committee. According to Colombian regulations, it is classified as having a lower than minimal risk.20 Informed consent was obtained from each participant. The principles of the Declaration of Helsinki of the World Medical Association were taken into account.21 The confidentiality of and respect for the information provided were guaranteed. This manuscript was constructed following the guidelines of the STROBE Declaration.22
ResultsFifty-nine point zero nine percent of those invited to participate responded to the survey. Of the 1,291 completed surveys, 3.5% (n = 44) did not authorise the use of the information for research, so they were excluded from the sample. Results are presented from the 1,247 surveys that were fully completed. The median age was 36 15 (range, 18–80) years; the other characteristics are presented in Table 1.
Sociodemographic and work characteristics of the study population.
| Age (years) | 37.1 ± 10.5 |
| 36.0 [15] | |
| Sex | |
| Male | 288 (23.1) |
| Female | 959 (76.9) |
| Type of work | |
| Related to patient care | 842 (67.5) |
| Administrative | 405 (32.5) |
| Way of working during the pandemic | |
| Face-to-face | 998 (80.0) |
| Remote | 249 (20.0) |
| Type of healthcare personnel | |
| Nurse's aide | 404 (32.4) |
| Professional nurse | 114 (9.1) |
| Physician | 156 (28.3) |
| Respiratory therapist | 15 (1.2) |
| Other | 335 (26.9) |
Values are expressed as n (%), mean ± standard deviation or median [interquartile range].
The presence of symptoms of anxiety in the study population in the two weeks prior was investigated. Forty-nine point nine percent of the population studied did not have anxious symptoms of clinical importance. Mild anxious symptoms (GAD-7 > 5) were identified in 31.7%, moderate symptoms (GAD-7 > 10) in 13.4%, and severe (GAD-7 > 15) in 5.1% of the participants. Table 2 lists the anxious symptoms grouped into symptoms of lesser clinical importance (not at all-several days) and of greater clinical importance (more than half the days-nearly every day).
Anxious symptoms in the last two weeks.
| Symptoms | Not at all-several days, n (%) | More than half the days-nearly every day, n (%) |
|---|---|---|
| You have felt anxious | 997 (79.9) | 250 (20.0) |
| You have not been able to stop or control worrying | 1,051 (84.3) | 196 (15.8) |
| You have been worrying too much about different things | 1,005 (80.6) | 242 (19.5) |
| You have had trouble relaxing | 1,015 (81.4) | 232 (18.6) |
| You have felt so restless that it is hard to sit still | 1,114 (89.3) | 133 (10.6) |
| You have become easily annoyed or irritated | 1,079 (86.5) | 168 (13.4) |
| You have been afraid that something awful might happen | 994 (79.7) | 253 (20.3) |
The presence of symptoms of depression in the study population in the two weeks prior was investigated. Fifty-nine point four percent of the participants had no depressive symptoms; mild symptoms (PHQ-9 = 5–9) were identified in 26.0%, moderate (PHQ-9 = 10–14) in 8.2%, moderately severe (PHQ-9 = 15–19) in 4.7% and severe (PHQ-7 > 20) in 1.7%. Table 3 lists the depressive symptoms grouped into symptoms of lesser clinical importance (not at all-several days) and of greater clinical importance (more than half the days-nearly every day).
Depressive symptoms in the last two weeks.
| Symptoms | Not at all-several days, n (%) | More than half the days-nearly every day, n (%) |
|---|---|---|
| Little interest or pleasure in doing things | 1,139 (90.9) | 114 (9.1) |
| You have felt down, depressed, hopeless | 1,132 (90.8) | 115 (9.2) |
| You have had trouble falling or staying asleep, or have slept too much | 943 (75.6) | 304 (24.4) |
| You have felt tired or had little energy | 1,011 (81.1) | 304 (18.9) |
| You have had a poor appetite or have overeaten | 1,026 (82.3) | 221 (17.7) |
| You have felt bad about yourself or that you are a failure or have let yourself or your family down | 1,146 (91.9) | 101 (8.1) |
| You have had trouble concentrating on things, such as reading the newspaper or watching television | 1,120 (89.8) | 127 (10.1) |
| You have been moving or speaking so slowly that other people could have noticed; or so fidgety or restless that you have been moving around a lot more than usual | 1,177 (94.4) | 70 (5.6) |
| Thoughts that you would be better off dead or of hurting yourself in some way | 1,227 (98.4) | 20 (1.6) |
It was found that 19.3% of women and 12.5% of men had problems related to appetite, whilst 25.7% of women and 19.8% of men had problems related to sleep. Regarding death or suicidal ideation, 62 women (6.4%) and 19 men (6.6%) admitted to this type of ideation in the prior two weeks.
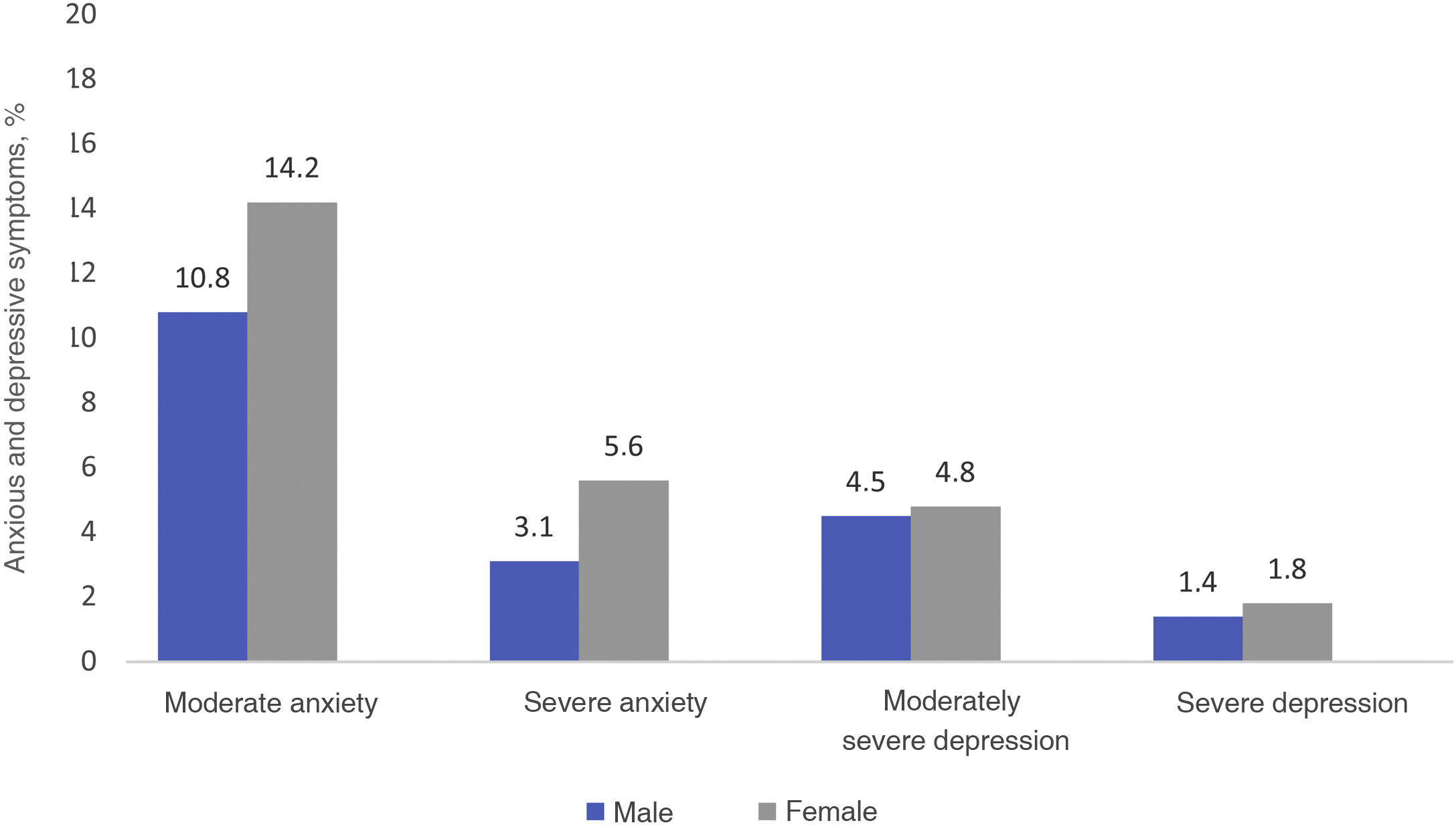
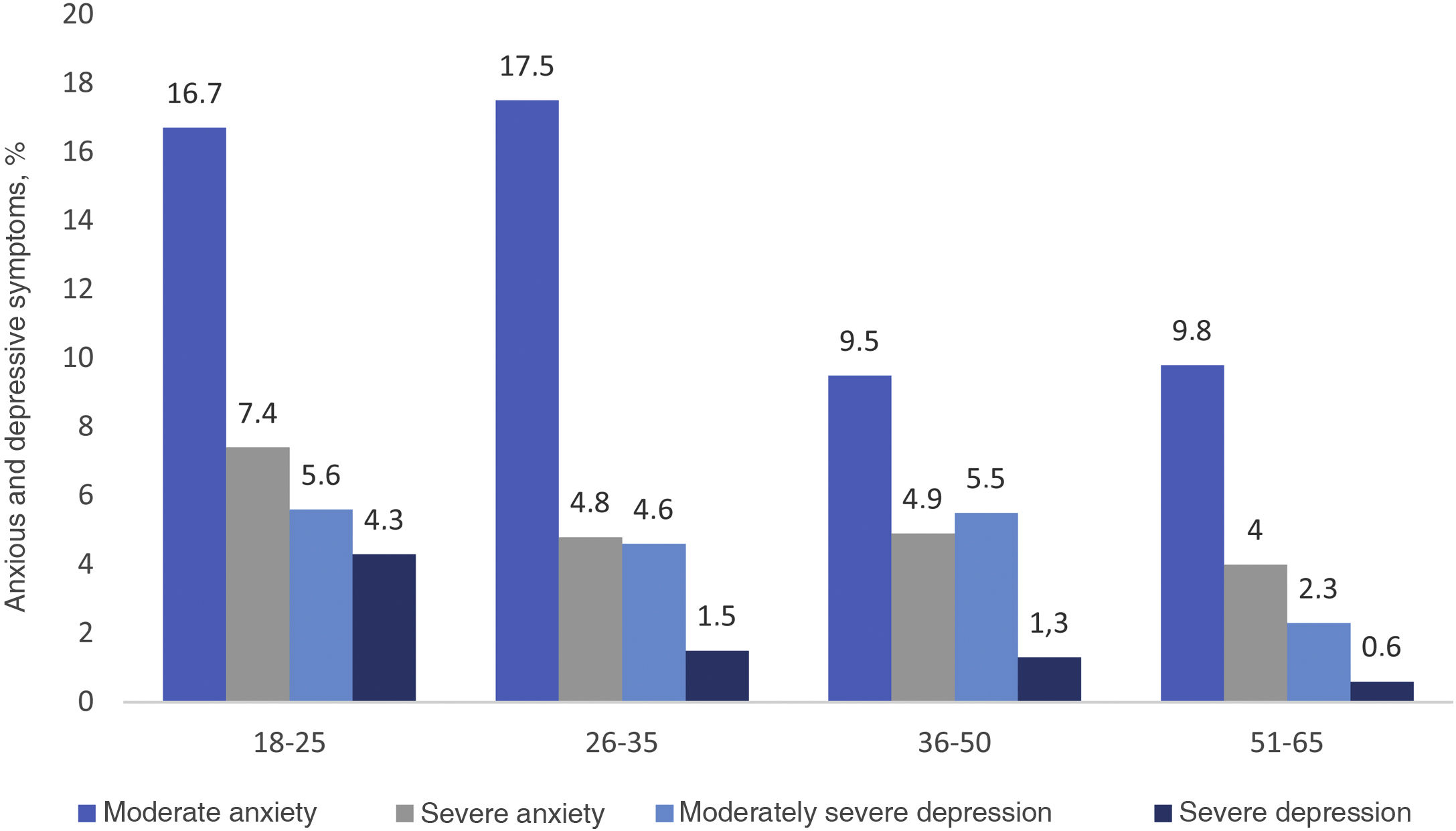
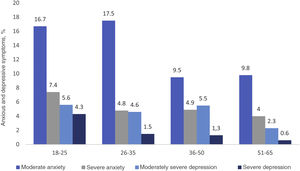
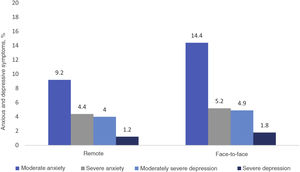
Moderate to severe symptoms of depression and anxietyClinically significant symptoms of depression and anxiety (of moderate and severe intensity) were reported by 14.6% and 18.5% of respondents, respectively. These were compared according to sex, age ranges and work modality (remote-virtual). A higher proportion of moderate to severe depressive and anxious symptoms was found in women, in the face-to-face work modality, and in the youngest participants (aged 18–25 years) (Figs. 1–3).
Possible associations of depressive and anxious symptoms with the other study variables were explored. The presence of symptoms of anxiety was associated with the female sex (p = 0.004) and the face-to-face work modality (p = 0.004). Symptoms of depression were associated with the female sex (p = 0.005), but not with the face-to-face work modality (p = 0.133). Likewise, the presence of moderate anxiety was higher in the personnel who carried out tasks associated with healthcare than in those with administrative tasks (p = 0.046).
DiscussionDuring 2020, workers in the health sector faced unprecedented situations: caring for patients with COVID-19, overcoming social changes, facing intense stressors such as the death of their peers, and making decisions in clinical scenarios of great uncertainty.8 This has led to health professionals being described in heroic terms. However, the potential mental health crisis that could develop among health workers has not received enough attention.9 The stress they are currently exposed to could affect the physical and mental health of the healthcare workforce and, in turn, reduce their ability to deal effectively with the current health emergency.8
The main finding of this study is that one in five people surveyed showed clinically-significant symptoms of anxiety, and one in six symptoms of depression. In the general population of Medellín, the prevalence of major depressive disorder in the last 30 days is 2.20% (that of any mood disorder, 2.82%) and that of generalised anxiety disorder, 0.46%, (that of any anxiety disorder, 5.08%).23 Therefore, the prevalence of depressive and anxious symptoms in our study with the health sector population was seven times higher for depression and up to 40 times for anxiety.
Our findings coincide with recent studies carried out in other countries, which have yielded alarming results regarding the mental health of health personnel.24,25 For example, the survey carried out by the team of Jianbo Lia et al.24 in 1,257 Chinese health personnel subjects, found depressive and anxious symptoms (from moderate to severe) in 14.8% and 12.3% of respondents, respectively. Also, in a recent systematic and meta-analytic review which included 13 studies and 33,062 participants, Pappa et al.25 found a prevalence of anxiety of 23.2%, of depression of 22.8% and of insomnia of 38.9%, which reveals the high prevalence of these mental symptoms in health workers.
Other authors have wanted to determine how some mental health symptoms are related according to the work carried out during the pandemic. In China, Zhang et al.7 conducted a study with 2,182 people with the aim of comparing psychosocial and mental health problems during the COVID-19 outbreak in two groups of workers. They found higher prevalences of insomnia (38.4% vs. 30.5%; p < 0.01), anxiety (13.0% vs. 8.5%; p < 0.01), depression (12.2% vs 9.5%; p < 0.04), somatisation (1.6% vs 0.4%; p < 0.01), and obsessive-compulsive symptoms (5.3% vs 2.2%; p < 0.01) in the medical group. Similarly, in our study it was observed that individuals with healthcare-related jobs reported anxious symptoms of moderate intensity more frequently than workers in non-clinical areas. Thus, the different stressors during long working hours, sleep deprivation, in addition to anxious and depressive symptoms, could constitute a significant source of fatigue and poor clinical judgement, which has a negative impact not only on the quality of life of the staff health, but also in the proper care of patients in need.
In addition, it is important to bear in mind that, even before the COVID-19 pandemic, health personnel constitute a vulnerable population in itself in terms of mental health problems. In fact, the suicide rate for physicians is 44%, higher than that of the general population. Nursing staff and other healthcare workers are also at high risk.26 Some authors point out that this risk could increase given the current situation.9 Accordingly, 6.5% of the individuals in our study admitted having had thoughts of death or suicide in the prior two weeks. Other studies have not reported findings on this particular aspect, which should be addressed as soon as possible.27
LimitationsAmong the limitations of this study are the following: first, because it is a cross-sectional study, the temporal relationship between exposure and disease cannot be accurately established; second, the instruments used to identify both depressive and anxious symptoms, although they are validated instruments and widely used in research, do not allow for diagnoses of depressive or anxiety disorder; third, the data presented only describe what happened at a specific time and cannot be generalised to another time, even in the same study population; fourth, recall biases are possible in this type of study; fifth, the participation of the employees was close, but it was <60%, and sixth, the previously mentioned inclusion and exclusion criteria did not take into account factors such as the time of employment contract, disabilities or annual leave and this will be reflected in a more heterogeneous sample, in itself not representative. However, this study provides important information regarding depressive and anxious symptoms in a large group of employees of a health institution in the city of Medellín during the COVID-19 pandemic.
ConclusionsHighly prevalent anxious and depressive symptoms were identified in workers of a health institution during the COVID-19 pandemic in the city of Medellín, Colombia. There was no clear predominance of anxious and depressive symptoms according to sex, as is usual in the general population. Despite the fact that more studies are necessary to measure the impact of these symptoms on health sector personnel, their high prevalence is already worrying.
Healthcare executives and managers need to be aware of the potential increase in psychological stress faced by healthcare workers during the times of COVID-19. Support for health sector personnel and their families could protect against adverse psychological outcomes. In view of the vital role played by this population in times of pandemic, the development of mental health programmes that address the problems of the health sector should be considered a priority.
Conflicts of interestThe authors have no conflicts of interest to declare.