To characterise the impact of the COVID-19 pandemic on psychiatric hospitalisations in the Latin American and Caribbean (LAC) region.
MethodsDescriptive study. 85 semi-structured interviews were conducted with health workers involved with psychiatric hospitalisations in general hospitals (GHs) and specialised psychiatric hospitals (SHs) from 18 LAC countries. The interviews were done between 8 May and 30 June 2020. The data were analysed quantitatively and qualitatively.
ResultsAn initial decrease in the demand for hospitalisation is reported, attributed to the population’s fear of approaching health services as well as restrictions on mobility. Stricter criteria for hospitalisation were reported with a double focus on the acute within the acute. The length of hospitalisations were mixed, with both increases and decreases in GHs and SHs. The therapeutic offer was drastically reduced, and interaction between hospitalised people and their support networks was restricted.
ConclusionsIn the COVID-19 context, hospitalisation seems to be not the last but the only alternative for psychiatric treatment. The decrease in the number of beds in SHs could be a positive aspect for the reform of psychiatric care, but it is questioned since this reduction also occurs in GHs.
Caracterizar el impacto de la pandemia por COVID-19 en las internaciones psiquiátricas en la región de América Latina y el Caribe.
MétodosEstudio descriptivo. Se realizaron 85 entrevistas semiestructuradas con trabajadores de hospitales generales (HG) y hospitales especializados (HE) en salud mental en 18 países de la región de América Latina y el Caribe entre el 8 de mayo y el 30 de junio de 2020. Los datos se analizaron cuantitativa y cualitativamente.
ResultadosSe reporta una disminución inicial en la demanda de internación, atribuida al temor de la población a acercarse a los servicios, así como a restricciones en la movilidad. Se indican criterios más estrictos para internar con una doble focalización de lo agudo dentro de lo agudo. Los tiempos de internación presentaron un comportamiento mixto, tanto de aumento como de disminución en HG y en HE. La oferta terapéutica durante la internación se vio drásticamente reducida, y se restringió la interacción de las personas internadas con sus redes de apoyo.
ConclusioneLa internación pareciera estar siendo no la última, sino la única alternativa de tratamiento psiquiátrico en el contexto de la pandemia. La reducción de camas en los HE podría ser un aspecto positivo para la reforma de la atención, pero es puesto en duda, ya que dicha reducción también se produce en los HG.
The COVID-19 pandemic has led to a reorganisation of healthcare services. Along with the preventive measures to restrict the movement of people, it has had an impact on healthcare for disorders that are not directly related to COVID-191. The WHO reports that the impact on the provision of other essential services entails the risk of significant setbacks in health and that a greater negative impact on vulnerable population groups is to be expected2.
One of these vulnerable groups is that of people with mental health problems who require hospitalisations to treat the crisis. Globally, and in the Latin American and Caribbean (LAC) region, psychiatric hospitalisation continues to be concentrated in psychiatric hospitals (PH), even though for three decades, mental health policies and legislation have insisted that hospitalisations must take place in general hospitals (GH)3, that a network of community-based services must definitively replace PHs and that the goal of "a continent without psychiatric hospitals by 2020" is being pursued4.
Specifically, recent data from the Americas region show that most psychiatric hospitalisation beds continue to be concentrated in PHs, with a median for the region of 16.7 beds per 100,000 inhabitants, compared to a median of psychiatric hospitalisation beds in GHs of 2.9/100,000 inhabitants5. This situation was already concerning before the pandemic, and progress towards the goal of closing psychiatric hospitals was delayed.
In this transitional scenario regarding reform of psychiatric healthcare, the pandemic introduces a series of challenges for inpatient services and the network of mental health services, due to the characteristics of the services and the population they serve.
Concern has arisen about the vulnerability of PHs to the rapid spread of COVID-19 due to the habitation conditions of such institutions, which in some cases are overcrowded, and the risk factors of the population hospitalised there for a long time in terms of age and comorbidities. PHs share these characteristics to a greater or lesser extent with other places that have also caused concern, such as nursing homes and prisons. In Belgium, Spain, the United States, and Argentina, a significant percentage of COVID-19 deaths have occurred in nursing homes6–10. Outbreaks have also been reported in prisons11. China, South Korea, Mexico and Bolivia have reported outbreaks of COVID-19 in some of their PHs12–15.
Besides that, GHs focused their work, at least at the beginning of the pandemic, on the care of COVID-19. Globally, much of the hospital infrastructure was geared towards pandemic care, and many GHs were re-purposed into "specialised" hospitals for COVID-19. In Italy, for example, where psychiatric hospitalisation occurs only in GHs, a reduction in the size of psychiatric units was observed, due to a decrease in staff and the allocation of beds to patients with COVID-1916. Also, and in general terms, the WHO Pulse survey indicated that 61% of responding countries reported disruptions in mental health service provision, 3% of which were severe or total2.
On the basis of the foregoing, it is necessary to identify the effects of the pandemic on psychiatric hospitalisations in both GHs and PHs in the LAC region, starting from the assumption that the pandemic reinforced the barriers to the occurrence of psychiatric hospitalisations, more markedly in GHs than in PHs.
Material and methodsIn order to characterise the impact of the COVID-19 pandemic on the provision of mental health services in the LAC region, a descriptive study was conducted, the field work for which was carried out in the months of May and June 2020. This study focuses on results regarding psychiatric hospitalisation in GHs and PHs, although in the wider study, other types of mental health services were investigated, such as rehabilitation, outpatient, and primary care services.
Intentional snowball sampling was employed17. The sampling began by identifying a potential interviewee for each of the countries in the region who met the selection criteria: work in management, provision of services or teaching and research in relation to a mental health service at the primary level of care, external consultation, rehabilitation, GH or PH. Thus, the sampling unit was mental health workers. In each of the countries, an attempt was made to interview at least one informant per type of service, and sampling was concentrated in capital cities and their metropolitan areas, as they were the ones with the highest number of COVID-19 cases at the time of the study. In Ecuador, where the epicentre was initially in the city of Guayaquil, efforts were made to establish contacts in that city as well. The first key informant per country was then asked if they could provide other contacts in the country or in the region who were linked by their work to mental health services. The internet pages of the region's psychiatric and psychological associations and colleges were also investigated in order to identify contacts. In turn, contacts were requested from people linked to international organisations that work in the region on mental health issues. Each potential interviewee was contacted twice, and if they did not respond, the previous contact was returned to in order to continue with the chain of contacts. The estimated response rate was 70%.
The size and final distribution of the interviews carried out by country and type of service was determined by the time established for the study, which was limited to two months, given the speed at which the context of the pandemic was changing and the infection prevention measures adopted by governments. An attempt was made to conduct interviews in all the countries of South America, Central America, and the Hispanic Caribbean, but it was not possible to establish contacts in the Dominican Republic or Puerto Rico.
For data collection, a specific semi-structured interview was conducted by type of service. The interviews were carried out by six members of the research team, all mental health professionals, and the interviewer was assigned according to the schedules that could be coordinated with the interviewee. Specifically for the interviews in Brazil, the option of doing them in Portuguese, English or Spanish was offered, according to the interviewee's preference, and in such cases the interviews were assigned to team members fluent in those languages.
The interview consisted of open and closed questions and inquired about: the impact of the pandemic on healthcare (demand, supply, and work organisation); subjective impact on service workers due to changes in their work; access to personal protection equipment and training, and perspective on the impact of the pandemic on psychiatric reform. Here we present the results referring to the impact of the pandemic on healthcare. The interview took 30−45 min, and was conducted by video call. When this was not possible, it was answered by filling in an electronic form. The interviewees gave their consent for the interview to be carried out and their identifying data and that of the institutions on which they reported was kept confidential. The protocol was evaluated by an ethics committee.
Quantitative descriptive analysis was used for the closed questions. For the open questions, analysis was qualitative. The interview questions were taken as macro themes and categorisation was carried out by pairs of researchers and discussed later with the wider team. Given the larger number of interviews from Argentina, a separate analysis was carried out to establish if there were differences and their potential weight in the comparative analysis between countries, but no significant differences were found.
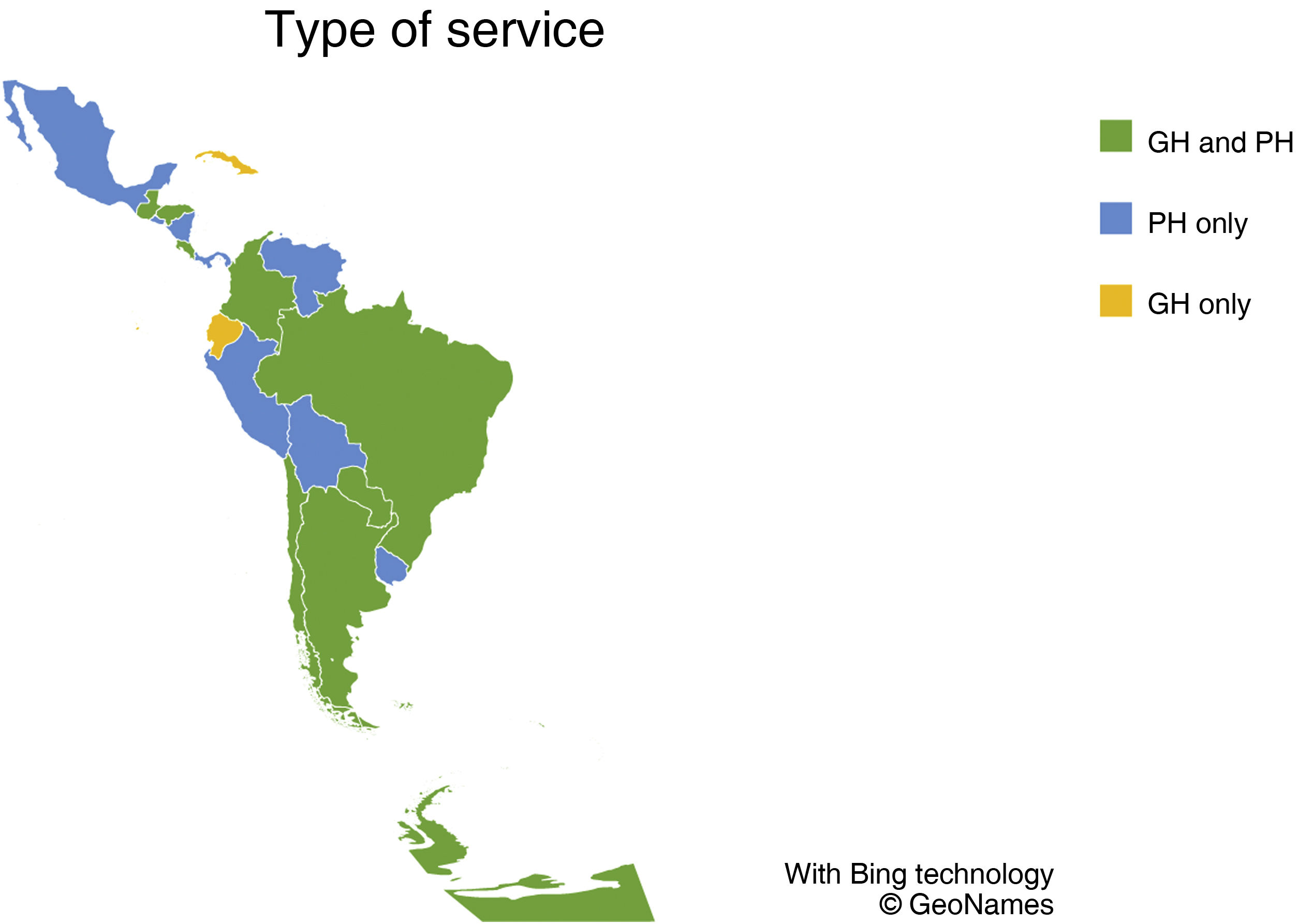
ResultsSpecifically, 85 of the interviews carried out in the general study corresponded to psychiatric hospitalisation services, distributed among 18 countries in the LAC region: 42 from psychiatric hospitals and clinics and 43 from GHs. Of the PH interviews, 20% (n = 8) corresponded to the emergency sector, and 30% (n = 13) in the GH interviews. Regarding the distribution of the interviews, fewer than five interviews were conducted in 14 countries, six to 10 interviews in three countries, and more than 10 in one country. Fig. 1 indicates the distribution by country according to responses by type of service.
It should be noted that during the study period most of the countries included had strict social distancing measures in force, with the exception of Nicaragua, Costa Rica and Uruguay18. Also, at the start of the study, 11 of the 18 included countries had a COVID-19 mortality rate of less than 1/100,000 inhabitants and at the end of the study, only five maintained rates <1/100,000 inhabitants, according to official data from each country.
The interviewees were 52% psychiatrists, 33% psychologists, 7% social workers, and the remaining 8% were from other professions. Eighty-eight percent of those interviewed worked in the direct provision of services.
The results corresponding to GHs and PHs are presented below. The quantitative results do not include emergency services, since the interview's closed questions were different for this type of service given their specific characteristics. Therefore, the quantitative responses correspond to 37 interviews for PHs and 30 for GHs. The qualitative results analyse all the interviews and are organised according to the areas of inquiry of the interview regarding healthcare: changes in demand, in healthcare processes and in the structure of services.
Admission to hospitals and psychiatric clinicsChanges in demandSixty-six percent of those interviewed reported a decrease in the demand for hospitalisation, although with variations over time from the beginning of the pandemic. The lower flow of people to substantiate a PH hospitalisation was mainly attributed to the preventive measures of restrictions on mobility and the population's fear of infection. An increase was subsequently recorded, due to receiving more complex crisis situations than usual, resulting from the interruption of the operation of outpatient services, as well as other inpatient services. This is also expressed by the personnel of the emergency services of these hospitals who, in addition, mentioned receiving the demand for hospitalisation not covered by the GHs. One interviewee pointed out: "… as the other specific health units have reduced their hours or have been suspended, we are treating serious cases that arrive practically ready for hospitalisation, decompensation of already known patients, decompensations, exacerbations of chronic patients (…) cases that truly merit attention because they have not been seen in recent weeks because they have not been able to access health services or they have not been able to pick up their medication.” (Paraguay).
Changes in healthcare processesSixty-eight percent of those interviewed reported greater difficulties in making an admission. They also pointed out that the hospitalisation criteria are stricter, due to the risk of infection for hospitalised people who, in general, are older adults and/or have comorbidities. In some hospitals, overcrowding aggravates the situation. For example: “we have an older population, which has a lot of comorbidities that are good cannon fodder for COVID. They also live in overcrowded conditions" (Argentina), and "we are trying to avoid admission at all costs to minimise the risk of infection" (Honduras).
Therapeutic resources during hospitalisation were reduced, and even complementary diagnostic tests were limited. As one interviewee pointed out: "there are no recreational or occupational therapy activities, so users are locked up all day doing nothing more than watching television." (Peru).
Furthermore, 92% of the interviewees reported a reduction in contact between hospitalised people and their support links, and as a strategy to reduce this distance, a greater use of telephone calls and video calls, which was an aspect valued positively by some interviewees. For example: "Now they have no choice but to get it going [the telephone link], WhatsApp groups were even set up with family members, the head of the ward and the nurses. It was unheard of." (Argentina).
Regarding the link between workers and hospitalised patients, there was unanimity in expressing the challenges that the use of personal protective equipment (PPE) introduces: "physical contact, paraverbal language, are very important things (…), emotional support with the patients (…) this has all diminished because we are like astronauts and people can only see our eyes," (Colombia); “I used my body more than I thought. There was less distance than I thought. If someone cried, I would do something with my body. Now it's a look or getting a tissue from the bathroom." (Argentina).
Likewise, it was indicated that the duration of hospitalisations has varied: 50% reported that they have decreased in cases in which the conditions of hospitalisation and the concern of family members due to the danger of infection required and allowed it, and 32% indicated that they have increased when the patient lives far away, has no support network and/or no resources for the continuity of treatment. For example: "A lot of patients have not been able to be discharged because their families have not come, coming from the interior (…) a lot of people have been stranded." (Bolivia). However, in health systems organised from demand-side subsidy, or in private services, the need of the institutions for financial equilibrium was indicated as an additional cause for the prolongation of hospitalisations, as new admissions were blocked. This confronts workers with the "ethical debate of understanding the financial need, but also the therapeutic indication." (Colombia).
Changes in the structure of servicesRegarding the physical space within the institutions, there was a reduction in the mobility of hospitalised people (with lockdown situations in the ward itself) and in the number of beds (to increase preventive distancing). Another notable factor was the reduction of staff due to: infection by COVID, preventive isolation, leave for belonging to an at-risk population, difficulties mobilising due to lockdown and/or reorganisation of services, and transfer of psychiatrists to clinical services. It should be noted that working multiple jobs in the health sector aggravates the situation. One interviewee commented: "(…) we had the case of a nurse who tested positive, but she had a contact at another institution (…), we locked down her ward, took samples from all the patients in that ward, and all the results were negative; luckily she took all the precautions when she was on duty and that way, luckily, she avoided massive infection." (Paraguay).
Hospitalisation in general hospitalsChanges in demandGH admission demand was similar to that of PH admission. At the beginning of the pandemic, there was a decrease of somewhat more than 50%, which is attributed to the fear of the population of coming to the hospital due to the risk of infection. Although some interviewees hypothesised that people "were more careful about decompensation" (Ecuador), they also agreed that later on demand increased, on the one hand due to people with anxiety, insomnia, situations of violence, consumption of alcohol, drugs and panic attacks due to isolation, and on the other to patients already in treatment who were destabilised due to lack of support. In some cases, the emergency teams directly request "referral to single speciality hospitals, to avoid infection and not occupy beds (…) for the care of patients with COVID-19." (Argentina).
Also, in some countries, GH workers redirected their work towards remote devices to address the impact of health workers the pandemic on the mental health of.
Changes in healthcare processesFocused on the care of COVID-19 cases, services from all specialties saw their healthcare process altered in the GH, although particularities in the mental health area were reported. Sixty-nine percent of interviewees mentioned difficulty in substantiating hospitalisations, with situations whereby only "hyperacute" cases were hospitalised or "(…) the admission of these people through emergency has been limited and referral to single speciality hospitals is requested by the emergency department's mental health team." (Argentina).
Although the reorganisation of work caused challenges for the continuity of treatment due to staff rotation and the limitation or elimination of group activities, this reorganisation was also valued positively as it implied greater efforts and coordination with families and other services to build alternatives to hospitalisation or expedite discharges.
Similarly to the PH, 90% of the interviewees indicated a reduction or suspension of the contact of hospitalised patients with their support links, with virtual alternatives implemented, and also highlighted the difficulties due to the use of PPE: "Visits were suspended, and I think this has and will continue to have a very profound therapeutic impact. We set up a telephone so that they can call, but clearly it is not the same. Symptoms get worse because there is no exchange of affection with family and friends." (Chile).
Regarding the duration of hospitalisations, 52% expressed a decrease in these due to the risk of infection and the limitation of the treatment programme, and 21% indicated an increase in hospitalisation times due to the closure of other community services or due to reluctance of some families to pick up their relative. They report that "it is difficult to externalise them because the outpatient places are not doing shifts" (Argentina), and add: "treatment has lost aspects that, for us, are fundamental. Emphasis had to be placed on the patient's physical health rather than mental health, unfortunately.” (Argentina)
Changes in the structure of servicesIn order to comply with the preventive measures of reduced movement of people, different strategies were implemented to reduce hours/days of work, alternation in shifts and by teams to avoid massive infection, and teleworking. Despite the fact that, in many cases, the number of working hours in the institution decreased, exhaustion stands out and the perception is of greater overburdening.
Finally, there was a decrease in hospital beds for mental health that were allocated to COVID-19 cases and, in many cases, the physical healthcare space was transferred to places outside the hospital. One emergency worker commented that, for consultations, "we began to see patients in the square in front of the hospital to avoid infection and care for them." (Argentina)
DiscussionBefore making a series of considerations based on the findings on the impact of the pandemic on psychiatric healthcare, it is necessary to state some of the limitations of the present study. To begin with, snowball sampling did not allow for a sample distribution that was representative of the services in the countries studied. Therefore, although they allow us to obtain valuable information, the results are limited by the fact that they may contain biases due to the characteristics of the sample. On the other hand, the instrument that was developed ad hoc could have been strengthened if it had been complemented with items from instruments for evaluating the quality of services for international use, developed by the World Health Organization, an aspect that would have made it possible to compare what was found in the pandemic with previous times, particularly in regard to questions about structure and healthcare processes.
Despite the indicated limitations, it is possible to raise some matters about what were approximately the first 100 days of the pandemic in the region's psychiatric hospitalisation services.
The results demonstrate a decrease in the demand for GH and PH admissions in all the countries at the beginning of the pandemic, which was reversed as, among other aspects, the effects of the reduction of territorial and community services began to appear in the population. This is an issue to consider from a perspective of transformation of healthcare, as despite this being something that is understood and promulgated with policies, the pandemic underscored the centrality of community services, since their absence or interruption further weakens the system and the population in need of care.
As the number of cases of COVID-19 increased, in countries with a certain development of outpatient services, it is also possible to see how the demand for hospitalisation in mental health is being redirected towards psychiatric clinics and hospitals, mainly due to the concentration of GH resources into COVID-19 care. Reference is made to the reflection of some crisis intervention service workers in the United States, who raised the dilemma regarding which risk to attend to as a priority: that of COVID-19 or that of the critical situation of the person with a mental health problem19. The mental healthcare systems in the region seem to have resolved the dilemma on the side of addressing the risk of COVID-19.
Under these circumstances, the consequences for the quality of mental healthcare from a rights perspective are clear: in many cases, people admitted to both PHs and GHs find themselves without the possibility of being discharged, without receiving visits from their relatives, with limited extra-institutional and institutional circulation, and with a limited treatment programme focused almost exclusively on pharmacological treatment. The care they are receiving in the current context, despite all efforts by the health personnel, is of low quality, evaluated according to international standards20, an aspect that is recognised and regretted by the workers themselves.
Despite this concerning situation, the health emergency scenario also demonstrated that it was possible to implement improvements in family, community, and inter-institutional coordination strategies to reduce hospitalisations, and increase and accelerate discharges, even at the risk of producing the revolving door effect. It is also clear that despite the difficulties and inequities regarding their access, communication technologies managed to establish themselves as a tool for work in mental health, with effects that can be analysed over time. Although it was expected that the migration to online platform support was more difficult in low- and middle-income countries than in high-income countries21, we can see that, although in some cases precariously, it was possible to incorporate such tools to work in the region.
The question that arises from observing the dynamics in the first 100 days of the pandemic in psychiatric hospitalisation services is: was it possible before COVID-19 to avoid hospitalisations with all the strategies that are currently being used due to the emergency or in the context of COVID-19, are people who would require it not being hospitalised?
On the other hand, the decrease in beds in clinics and psychiatric hospitals to respect the distance necessary to reduce the spread of COVID-19 provides an image of the state of many of these institutions. The progressive reduction in the number of beds could be a positive aspect, considering that it is an indicator of mental healthcare reform22. However, this must be evaluated in light of what has happened in the network of mental health services and, in particular, about the availability of beds in GHs. In the context of the focus of health systems on pandemic care, the decrease in beds in GHs and PHs, along with the interruption of outpatient and rehabilitation services, indicates a concerning outlook regarding access to care.
The human resources situation also introduces paradoxes. GH and PH staff are showing signs of exhaustion due to the intensity of work, exposure to infection and because they are in direct contact with suffering and death. Leave for reasons related to the pandemic and the conditions, in many, of working multiple jobs, are added to this. There is also the feeling in the workers of having seen their work capacity limited by the reorganisation of the services and by PPE being part of the biosafety strategies. In this concerning scenario, it is worth noting the demonstrated capacities for the reorganisation of work and the implementation of remote care mechanisms adopted, to a greater or lesser extent, in all countries.
In conclusion, it could be pointed out that COVID-19 revealed the shortcomings of mental healthcare. Although all the specialties of the GH were affected by the reorganisation necessary to attend to the cases of COVID-19, the transfer of inpatient mental health services from the PH to the GH is evidently still a weak process, further weakened by the current situation. This scenario places psychiatric hospitals and clinics at the centre of the mental healthcare model, with slowing down, and in many places regression of the processes aimed at complying with what was agreed on for the Region: "a continent without psychiatric hospitals in 2020"4.
Conflicts of interestThe authors have no conflicts of interest to declare.