To classify the staff of two reference institutions for COVID-19 care in Antioquia according to the intensity of anxiety and depression symptoms, and to determine the factors associated with these classes.
MethodsCross-sectional study in which the GAD-7, PHQ-9, fear of COVID-19, and the Copenhagen Burnout scale were used. Latent class analysis was performed to identify the classes, and the factors associated with these were determined using multinomial logistic regression.
Results486 people participated. The three-class model had the best fit: class I with low scores on the scales; class II with mild degrees of anxiety and depression, and intermediate levels of fear of COVID-19 and perceived stress; and class III with moderate and severe degrees of anxiety, depression, and perceived stress. The factors associated with belonging to class III were age (OR = 0.94; 95%CI, 0.91−0.96), change of residence to avoid exposing relatives (OR = 4.01; 95%CI, 1.99–8.09), and a history of depressive disorder (OR = 3.10; 95%CI, 1.27–7.56), and anxiety (OR = 5.5; 95%CI, 2.36–12.90). Factors associated with class II were age (OR = 0.97; 95%CI, 0.95−0.99), history of depressive disorder (OR = 3.41; 95%CI, 1.60−7.25), living with someone at risk of death from COVID-19 (OR = 1.86; 95%CI, 1.19−2.91), family member being healthcare staff (OR = 1.58; 95%CI, 1.01−2.47), and change of residence to avoid exposing relatives (OR = 1.99; 95%CI, 1.11−3.59).
ConclusionsThree classes of participants were obtained, two of them with anxiety and depression symptoms. Younger age and a history of mental disorder were factors associated with the two classes of symptomatic patients; other factors may be causes or consequences of the symptoms.
Clasificar al personal de 2 instituciones de referencia para la atención de la COVID-19 en Antioquia según la intensidad de los síntomas ansiosos y depresivos y determinar los factores asociados con estas clases.
MétodosEstudio de corte transversal en el que se usaron las escalas GAD-7, PHQ-9, miedo a la COVID-19 y escala Burnout de Copenhague. Se hizo análisis de clases latentes para identificar las clases y se determinaron los factores asociados mediante regresión logística multinomial.
ResultadosParticiparon 486 personas. El modelo con mejor ajuste fue el de 3 clases. La I, con puntajes bajos en escalas; la II, con grados leves de ansiedad y depresión, e intermedios de miedo a la COVID-19 y estrés percibido; y la III, con grados moderados y graves de ansiedad, depresión y estrés percibido. Los factores asociados con pertenecer a la clase III fueron: edad (OR = 0,94; IC95%, 0,91–0,96), cambio de vivienda para no exponer a familiares (OR = 4,01; IC95%, 1,99–8,09), y antecedente de trastorno depresivo (OR = 3,10; IC95%, 1,27–7,56) y ansioso (OR = 5,5; IC95%, 2,36–12,90). Los factores asociados con la clase II fueron: edad (OR = 0,97; IC95%, 0,95–0,99), antecedente de trastorno depresivo (OR = 3,41; IC95%, 1,60–7,25), convivir con alguien con riesgo de muerte por COVID-19 (OR = 1,86; IC95%, 1,19–2,91), familiar personal de salud (OR = 1,58; IC95%, 1,01–2,47) y cambio de vivienda para no exponer a familiares (OR = 1,99; IC95%, 1,11–3,59).
ConclusionesSe obtuvieron 3 clases de participantes, 2 de ellas con síntomas ansiosos y depresivos. La menor edad y el antecedente de un trastorno mental fueron factores asociados con las 2 clases de pacientes sintomáticos; otros factores pueden ser causa o consecuencia de los síntomas.
The 2019 pandemic caused by the acute respiratory syndrome coronavirus (COVID-19) has entailed an important challenge for the world's health systems; in this setting, the need for physicians specialising in various fields has become apparent, and in general there has been increased demand for health services in all levels of care, owing to which the existence of mental health risk for health workers has been postulated.1 In the field of medicine, several stress factors have been identified: increased workload, night shifts, working in emotionally demanding environments, the need to take rapid decisions, information overload, lack of positive comments, low salaries, and a substandard work environment.2 In emergency departments, emotional exhaustion, depersonalisation, avoidance-focused coping, being a doctor and smoking on a daily basis are related with a higher probability of suffering from mental health problems.3
In a systematic review of the literature up to 17 April 2020, to determine the prevalence of depression, anxiety, and insomnia among health workers during the COVID-19 pandemic,4 Pappa et al. estimated a clustered prevalence of depression of 23.2% 95% confidence interval [95% CI], 17.77–29.12; I2 = 99%), of depression of 22.8% 95% CI, 15.1–31.51; I2 = 99.62%) and of insomnia of 38.9% (95% CI, 27.45–41.54; I2 = 98%); with the prevalence of anxiety and depression being higher in females than in males (20.92 vs. 29.06%; and 20.34 vs. 26.87%, respectively).
In Colombia, surveys have also been carried out to evaluate the prevalence of the symptoms of anxiety and depression in healthcare personnel. In April 2020, Monterrosa et al. distributed a survey, via the social networks and email, to Colombian physicians who had worked during the month of March 2020; their aim was to evaluate anxiety with the General Anxiety Disorder-7 Scale (GAD-7), stress with the work-related stress test, and fear of COVID-19 with a specific scale. In this study, the response rate was 37.9% and anxiety was found (GAD-7 > 10) in 39.3% of participants; this group included the younger members, and there was a greater proportion of females. Subjects with symptoms of anxiety reported fear of having suffered symptoms of COVID-19, fear of taking the virus home with them, disappointment in the workplace, feeling anxious about going to work the following day, and considering leaving their jobs to protect the members of the family, in comparison with those with no symptoms of anxiety.5 In the city of Medellín, between 1 March and 31 May 2020, a further survey on the prevalence of symptoms of depression and anxiety was conducted with the PHQ-9 and GAD-7 scales on 1247 healthcare workers in one of the city's institutions. Symptoms of depression were found in 26.0%: moderate (PHQ-9 = 10–14) in 8.2%, moderately severe (PHQ-9 = 15–19) in 4.7% and severe (PHQ-7 > 20) in 1.7%. With regard to anxiety, they found moderate symptoms (GAD-7 > 10) in 13.4%, and severe (GAD-7 > 15) in 5.1% of the participants: 14.6% reported symptoms of depression, and 18.5% reported clinically significant symptoms of anxiety.6
Symptoms of depression and anxiety generally coexist in individuals and, as has been observed in prevalence studies, affect a high proportion of the population. Accordingly, there are subgroups of individuals depending on the intensity of the symptoms, which have factors are associated with belonging to each group. Latent class analysis is a statistical classification technique which assumes that the individuals in a population find themselves in classes that are homogeneous within the same, but differential compared to other classes according to the variables analysed.7 Ascertaining the factors associated with the different profiles or subgroups according to the intensity of the symptoms enables the design of preventive and early detection interventions for the workers' health problems. The objective of this study is to classify the healthcare personnel from two referral hospitals in Antioquia for the treatment of COVID-19 according to the intensity of their symptoms of anxiety and depression, and to determine the factors associated with membership of these classes, at a time when the first peak of infections has already occurred (July and August 2020), and in the middle of a second peak (December 2020 and January 2021), when there were fewer hospital beds available.
MethodsThis was a cross-sectional study, whose population was the healthcare personnel of two referral hospitals for the department of Antioquia (Hospital Universitario San Vicente Fundación [San Vicente Foundation University Hospital and the IPS Universitaria [University Service Provider Institution]). The study was approved by the university bioethics committee and the research committees of the two hospitals, and was conducted in accordance with the ethical principles of the Declaration of Helsinki. Informed consent was included in the survey.
The inclusion criteria were agreeing to participate in the study, being 18 years of age or older, and working in the participating institutions attending to patients (physician, nurse, therapist, psychologist, bacteriologist, dentist, surgical instrument technician, nurse's aide, therapist or technician, orderly etc.) or in administrative, maintenance, cleaning or food service work. Trainee staff were excluded. The survey was sent by email to all the workers in the institutions who, before filling it in, had to agree to participate in an informed consent process.
The survey was sent from the month of October 2020 and responses were accepted up until the month of January 2021; a Google Drive Form was used, which included the evaluation of the symptoms of anxiety, depression, perceived stress, and fear of COVID-19 through the GAD-7 Scale,8 PHQ-9 Scale,9 Perceived Stress Scale (PSS-10)10 and Fear of COVID-19 Scale.11 Data on demographic characteristics and the medical and psychiatric histories of the population were also collected.
Data collection instrumentsPatient Health Questionnaire-9. A nine-item scale published in 2001, which is used in primary health care to screen for depression and measure the intensity of depressive symptoms.12 It forms part of the PHQ, a self-administered version derived from the Primary Care Evaluation of Mental Disorders (PRIME-MD), to screen for various psychiatric disorders.13 It has been translated into various languages, and is one of the most highly recommended owing to its accuracy in screening for major depressive disorder.14,15 It has been validated in Colombia, where it showed an area under the curve (AUC) for receiver operating characteristics (ROC) of 0.92 (95% CI, 0.88−0.963), a sensitivity of 90.38 (95% CI, 81.41–99.36) and a specificity of 81.68 (95% CI, 75.93–87.42).9,16 The cut-off points for symptoms of mild, moderate, moderately severe and severe symptoms of depression are 5, 10, 15 and 20, and there is evidence of sensitivity to change.17
Seven-item anxiety scale. A scale for identifying probable cases of anxiety disorders and measuring the severity of depression, published by Spitzer17 in 2007. It comprises seven items with four response options, and scores from 0 to 21. It is widely used and has been validated in Spanish; it has only one dimension and has demonstrated adequate internal consistency (α = 0.936), test-retest reliability (intra-class correlation coefficient [ICC] = 0.926; 95% CI, 0.881−0.958) and construct validity owing to its correlation with other anxiety scales.8,13 With regard to criterion validity, it has an AUC ROC = 0.957 (95% CI, 0.930−0.985), and at the cut-off point of 10, a sensitivity of 86.8% and a specificity of 93.4%.8 The thresholds used were <5 (no anxiety), 5–10 (mild symptoms), 10–15 (moderate symptoms) and >15 points (severe symptoms).
Perceived stress scale. This was initially designed with 14 items, which were then reduced to 10, with five response options18,19 and scores between 0 and 40. It has been validated in Colombia, with adequate internal consistency in each of its dimensions (α = 0.82 and α = 0.83), stress perception and coping capacity. A cut-off point of 26 was used, on statistical grounds.
Fear of COVID-19 scale. A seven-item scale developed in Iran with five Likert-type response options and possible scores between 7 and 35.20 It has one single dimension with high internal consistency (α = 0.82) and items presented difficulty between –0.83 and 0.98; it has no differential item functioning by age and gender. Its construct validity was tested with the correlation with the dimensions of anxiety and depression from the Hospital Anxiety and Depression Scale (HADS) and the dimensions “perceived infectability” and “germ aversion” from the Perceived Vulnerability to Disease Scale, with correlation coefficients of 0.51, 0.42, 0.48 and 0.45, respectively.21,22 Validated in Spanish for Peru, it showed that the most suitable model according to the confirmatory factor analysis is with two dimensions, one general and another emotional and somatic, adequate convergent construct validity due to its moderate correlation with the impact of event scale (IER-S) and of depressive symptoms (PHQ-9) and both dimensions showed good internal consistency (α >0.8).10
Copenhagen Burnout Inventory. A questionnaire with three sub-dimensions: personal burnout, work-related burnout, and client-related burnout. The focus of the scale analysis is fatigue and exhaustion, and the principal aim is to respond to the question “How tired or distressed do you feel?”. This questionnaire is based on the Maslach Burnout Inventory (MBI).23 The questions in the work-related exhaustion scale are based on the emotional exhaustion subscale of the MBI/MBI-GS questionnaires. The questions on client-related burnout were formulated by the development group. It has very high Cronbach's alpha values for internal reliability (0.85/0.87).24 Validated in Spanish, it has been reported that all items showed positive and moderate discrimination (between one and two categories). The three scales exhibited a correct mean correlation between items (between 0.42 and 0.60), low variance (between 0.008 and 0.012) and an adequate corrected item-total correlation (between 0.49 and 0.83, except for one item which obtained 0.39), indicating acceptable homogeneity. The internal consistency of the three scales was satisfactory: 0.90 (95% CI, 0.88−0.92) for PB; 0.83 (95% CI, 0.81−0.86) for WB, and 0.82 (95% CI, 0.78−0.85) for CB. Cronbach's alpha coefficient was satisfactory for all the COPSOQ scales used.25
Statistical analysisThe characteristics of the participants were described by means of descriptive statistical measures. The mean ± standard deviation for variables whose distribution was assumed to be normal, or otherwise, the median [interquartile range] was used. The data distribution was evaluated by examining graphs (histogram and Q–Q plot) and with the Shapiro-Wilk test, skewness and kurtosis. For qualitative variables, frequencies and percentages were used.
The profile of depressive and anxiety symptoms was established by means of a latent class analysis (LCA),7 for which the results according to categories in the GAD (no anxiety, mild anxiety, moderate anxiety and severe anxiety), PHQ (no depression, mild depression, moderate depression and severe depression) and PSS (high perceived stress, >26 points) scales were included. The LCA is widely applied in clinical research for diagnosis, to establish “hidden” phenotypes, in prevention and to direct treatment, and specifically in mental health studies to determine patient profiles on the basis of signs and symptoms.26–29 The LCA allows the study population to be stratified into classes on the basis of sample data for categorical variables that are assumed to be unobserved (latent) on the basis of the manifest or observed variables (in our case, GAD, PHQ and PSS). The model initially assumes a homogeneous population (one class) and it is compared with models of two to 10 classes (rule of thumb); if no suitable solution is found up to 10 classes, models with more than 10 classes can be evaluated, although this may involve complexity in the interpretation by stratifying the population into a greater number of classes. The basic assumption of the LCA is that the population is already stratified into k classes, but it is the investigator who does not know them; it also assumes a reflexive model in which the probability or response function in the manifest variables depends on membership of a determined class (Ki) or is conditioned by the same. The other assumption is that the manifest variables are independent in each class (assumption of local independence). In studies on mental health, this assumption may be difficult to meet, given that the different signs and symptoms of psychiatric disorders may overlap or be correlated; hence it was decided to work at the level of the entire scale and its categories, and not at the level of each item of each scale and, additionally, owing to the limitations of sample size for the total number of items between the three scales. To estimate the model of k classes which is compatible with the data, the Bayesian Information Criterion (BIC) or the Akaike Information Criterion (AIC) was used, and the indices modified by adjusting the number of parameters (aBIC and cAIC). According to these indices, the model with the lowest values could be more compatible with the data observed. Also calculated was the entropy, allowing the evaluation of classification quality (or classification accuracy) which ranges from 0 to 1 (closer to 1 indicates a better classification quality). For this analysis, the poLCA30 was used.
The association of the clinical and demographic characteristics was examined using multinomial logistic regression analysis. The class with the lowest probability of symptoms of depression, anxiety or stress was selected as reference. The variables that were included in the model were selected taking into account their psychopathological plausibility and they were based on four groups of variables: a) individual sociodemographic; b) individual of clinical history; c) individual of perceived stress and contagion, and d) occupational. The odds ratio (OR) and adjusted odds ratio (ORa) are presented for age, sex, work experience, history of psychiatric disorders, and living with a person at high risk of death from COVID-19 with their respective 95% CIs. For this analysis, the multinom function of the nnet package in R was used.31 Generally, all analyses were conducted with version 4.0.5 of the R programming languages32 and R-studio, version 1.4.1106.33
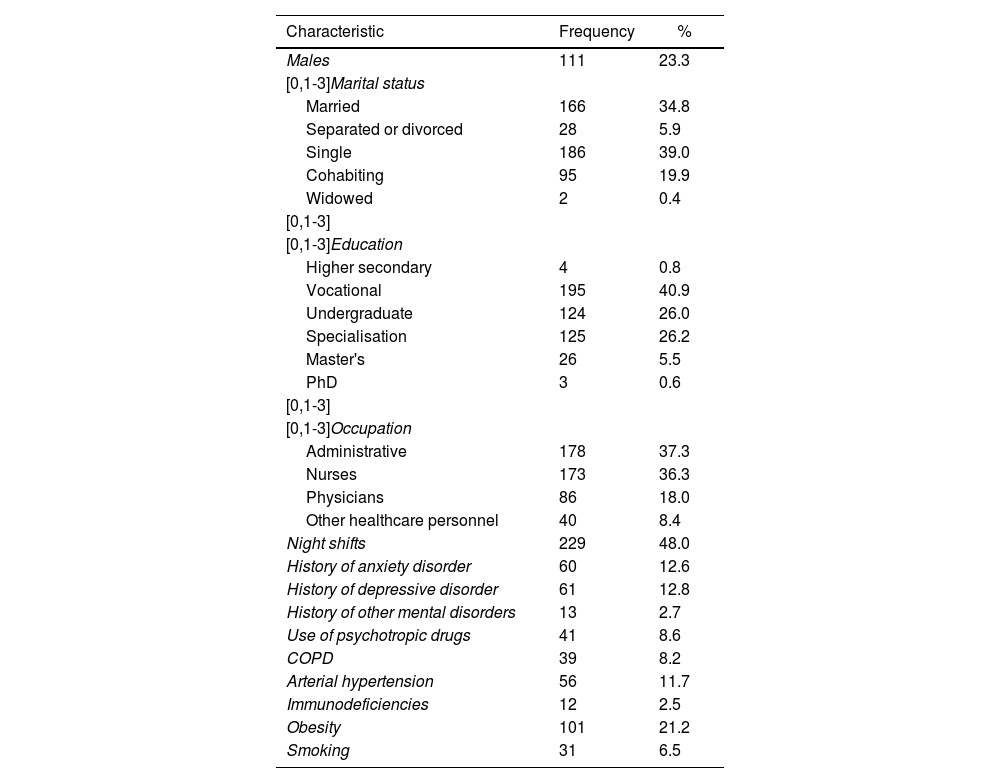
ResultsThe survey was sent to 5358 employees from the two institutions, and 486 responded (response rate of 9.07%). The mean age was 36.7 ± 9.5 years and the mean for work experience was 12.21 ± 8.5 years. Among the personal history aspects important for complications in case of infection with coronavirus, 21.2% had obesity and 11.7% a history of arterial hypertension. With regard to psychiatric background, 12.8% had a diagnosis of a depressive disorder and 12.6% of an anxiety disorder (Table 1).
Demographic characteristics and background of the study population.
| Characteristic | Frequency | % |
|---|---|---|
| Males | 111 | 23.3 |
| [0,1-3]Marital status | ||
| Married | 166 | 34.8 |
| Separated or divorced | 28 | 5.9 |
| Single | 186 | 39.0 |
| Cohabiting | 95 | 19.9 |
| Widowed | 2 | 0.4 |
| [0,1-3] | ||
| [0,1-3]Education | ||
| Higher secondary | 4 | 0.8 |
| Vocational | 195 | 40.9 |
| Undergraduate | 124 | 26.0 |
| Specialisation | 125 | 26.2 |
| Master's | 26 | 5.5 |
| PhD | 3 | 0.6 |
| [0,1-3] | ||
| [0,1-3]Occupation | ||
| Administrative | 178 | 37.3 |
| Nurses | 173 | 36.3 |
| Physicians | 86 | 18.0 |
| Other healthcare personnel | 40 | 8.4 |
| Night shifts | 229 | 48.0 |
| History of anxiety disorder | 60 | 12.6 |
| History of depressive disorder | 61 | 12.8 |
| History of other mental disorders | 13 | 2.7 |
| Use of psychotropic drugs | 41 | 8.6 |
| COPD | 39 | 8.2 |
| Arterial hypertension | 56 | 11.7 |
| Immunodeficiencies | 12 | 2.5 |
| Obesity | 101 | 21.2 |
| Smoking | 31 | 6.5 |
COPD: chronic obstructive pulmonary disease.
The mean for the scores on the GAD-7 scale was 5.34 ± 4.48 and in that of fear of COVID-19, 16.58 ± 6.66. The median for the PHQ-9 was 4 [2–8] and for the PSS, 20 [18–23]. The scores of the GAD-7 indicated mild symptoms of anxiety in 36.8%, moderate in 11.1% and severe in 4.1%. Based on the PHQ-9, symptoms of depression were mild in 30.5%, moderate in 11.7%, and severe in 6.5%. Twelve point six percent had a high degree of perceived stress according to the PSS scale.
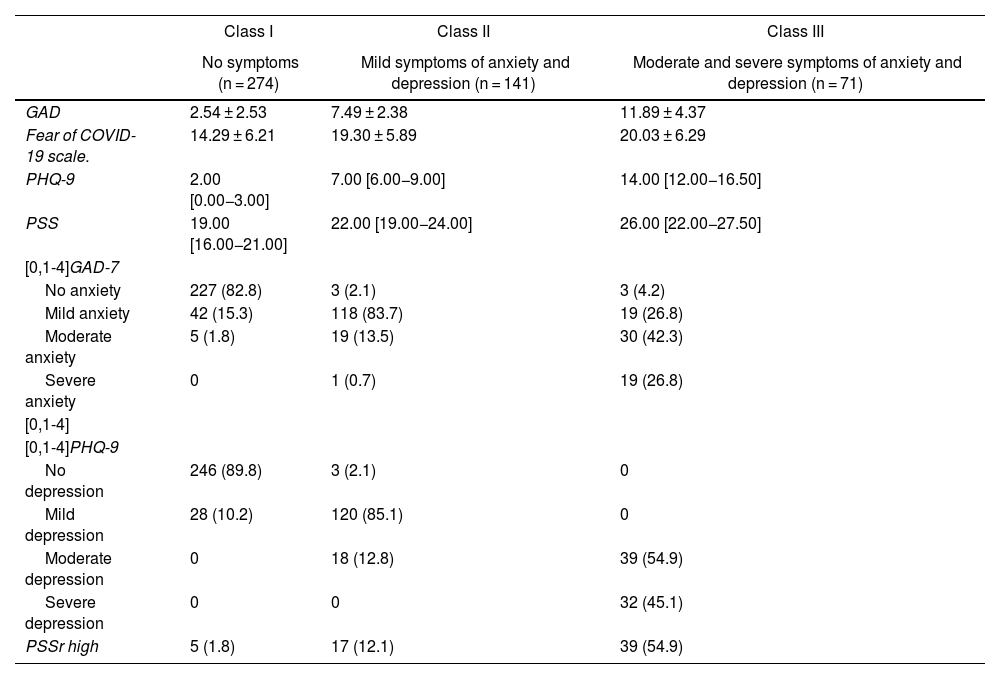
In the LCA, the model that had the best fit was three classes, with BIC of 2,335.586, AIC of 2,226.745, ABIC of 2,253.064, cAIC of 2,361.586 and entropy of 0.797 (see Appendix B Table 1 of the additional material). When observing the characteristics of each of the classes, in class I there are 274 participants (56.4%) who have predominantly low scores in anxiety, depression, fear of COVID-19 and perceived stress; in class II, which has 141 participants (29.0%), mild degrees of anxiety and depression, are more frequent, along with intermediate scores for fear of COVID-19 and perceived stress; and for class III, with 71 participants (14.6%), moderate and severe degrees of anxiety and depression are found, along with higher average scores for perceived stress (Table 2).
Profile of classes obtained according the symptoms of anxiety and depression.
| Class I | Class II | Class III | |
|---|---|---|---|
| No symptoms (n = 274) | Mild symptoms of anxiety and depression (n = 141) | Moderate and severe symptoms of anxiety and depression (n = 71) | |
| GAD | 2.54 ± 2.53 | 7.49 ± 2.38 | 11.89 ± 4.37 |
| Fear of COVID-19 scale. | 14.29 ± 6.21 | 19.30 ± 5.89 | 20.03 ± 6.29 |
| PHQ-9 | 2.00 [0.00−3.00] | 7.00 [6.00−9.00] | 14.00 [12.00−16.50] |
| PSS | 19.00 [16.00−21.00] | 22.00 [19.00−24.00] | 26.00 [22.00−27.50] |
| [0,1-4]GAD-7 | |||
| No anxiety | 227 (82.8) | 3 (2.1) | 3 (4.2) |
| Mild anxiety | 42 (15.3) | 118 (83.7) | 19 (26.8) |
| Moderate anxiety | 5 (1.8) | 19 (13.5) | 30 (42.3) |
| Severe anxiety | 0 | 1 (0.7) | 19 (26.8) |
| [0,1-4] | |||
| [0,1-4]PHQ-9 | |||
| No depression | 246 (89.8) | 3 (2.1) | 0 |
| Mild depression | 28 (10.2) | 120 (85.1) | 0 |
| Moderate depression | 0 | 18 (12.8) | 39 (54.9) |
| Severe depression | 0 | 0 | 32 (45.1) |
| PSSr high | 5 (1.8) | 17 (12.1) | 39 (54.9) |
PSSr: perceived stress scale; GAD: Generalised Anxiety Disorder-7; PHQ: patient health questionnaire 9.
Values are expressed as n (%), mean ± standard deviation or median [interquartile range].
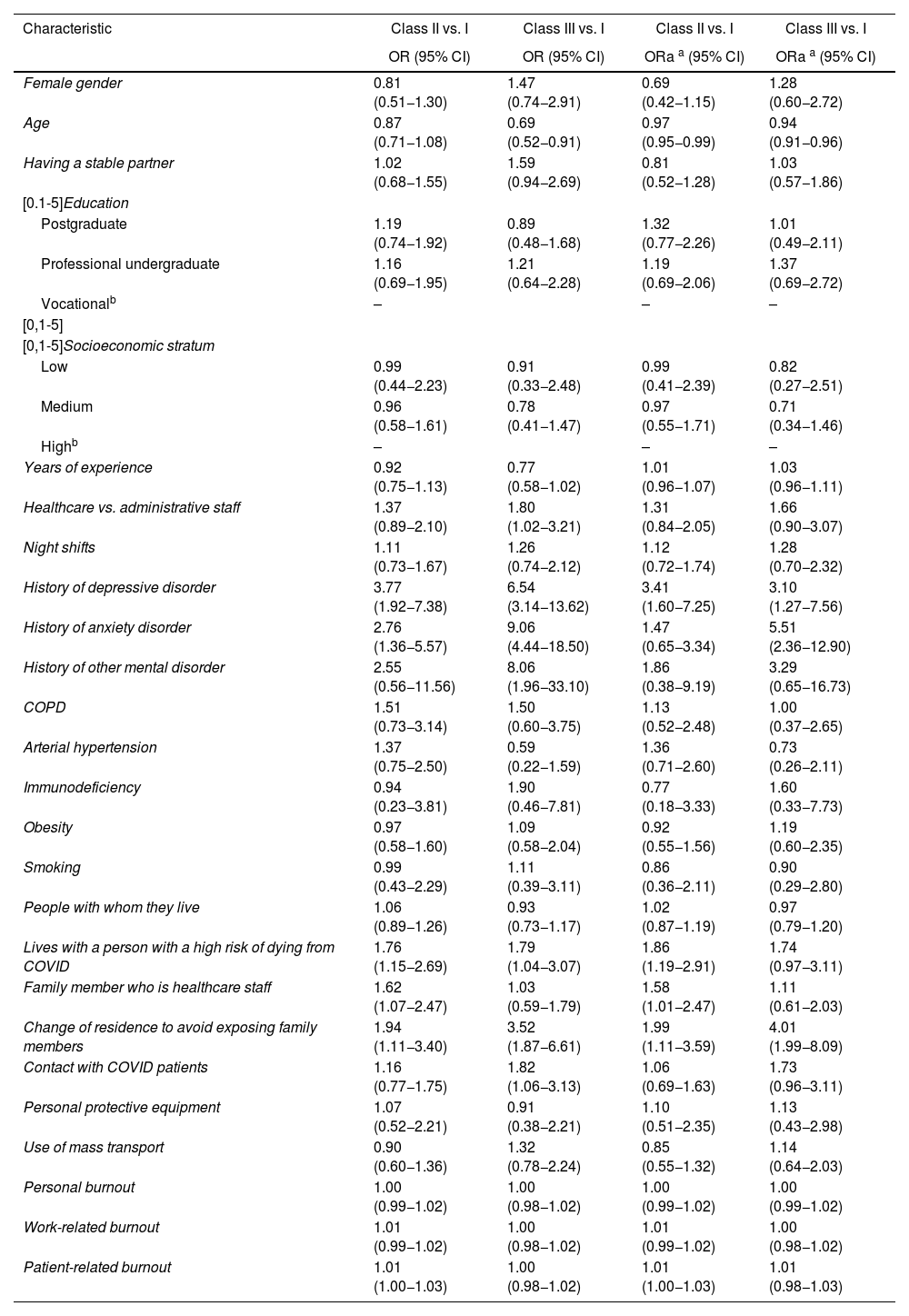
After adjusting for sex, age, work experience, history of psychiatric disorders and living with a person at high risk of death from COVID-19, the factors associated with membership of class II in comparison with class I were: age (OR = 0.97; 95% CI, 0.95−0.99), history of depressive disorder (OR = 3.41; 95% CI, 1.60−7.25), living with a person at high risk of death from COVID-19 (OR = 1.86; 95% CI, 1.19−2.91), having a family member who is healthcare staff (OR = 1.58; 95% CI, 1.01−2.47) and change of residence to avoid exposing family members (OR = 1.99; 95% CI, 1.11−3.59). The factors associated with belonging to class III in comparison with class I were age (OR = 0.94; 95% CI, 0.91−0.96), history of depressive disorder (OR = 3.10; 95% CI, 1.27−7.56), history of anxiety disorder (OR = 5.51; 95% CI, 2.36−12.90) change of residence to avoid exposing family members (OR = 4.01; 95% CI, 1.99−8.09) (Table 3 and Appendix B Tables 2 and 3 of the additional material).
Factors associated with belonging to classes I (no symptoms), II (mild symptoms of anxiety and depression) and III (moderate to severe symptoms of anxiety and depression).
| Characteristic | Class II vs. I | Class III vs. I | Class II vs. I | Class III vs. I |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ORa a (95% CI) | ORa a (95% CI) | |
| Female gender | 0.81 (0.51−1.30) | 1.47 (0.74−2.91) | 0.69 (0.42−1.15) | 1.28 (0.60−2.72) |
| Age | 0.87 (0.71−1.08) | 0.69 (0.52−0.91) | 0.97 (0.95−0.99) | 0.94 (0.91−0.96) |
| Having a stable partner | 1.02 (0.68−1.55) | 1.59 (0.94−2.69) | 0.81 (0.52−1.28) | 1.03 (0.57−1.86) |
| [0.1-5]Education | ||||
| Postgraduate | 1.19 (0.74−1.92) | 0.89 (0.48−1.68) | 1.32 (0.77−2.26) | 1.01 (0.49−2.11) |
| Professional undergraduate | 1.16 (0.69−1.95) | 1.21 (0.64−2.28) | 1.19 (0.69−2.06) | 1.37 (0.69−2.72) |
| Vocationalb | – | – | – | |
| [0,1-5] | ||||
| [0,1-5]Socioeconomic stratum | ||||
| Low | 0.99 (0.44−2.23) | 0.91 (0.33−2.48) | 0.99 (0.41−2.39) | 0.82 (0.27−2.51) |
| Medium | 0.96 (0.58−1.61) | 0.78 (0.41−1.47) | 0.97 (0.55−1.71) | 0.71 (0.34−1.46) |
| Highb | – | – | – | |
| Years of experience | 0.92 (0.75−1.13) | 0.77 (0.58−1.02) | 1.01 (0.96−1.07) | 1.03 (0.96−1.11) |
| Healthcare vs. administrative staff | 1.37 (0.89−2.10) | 1.80 (1.02−3.21) | 1.31 (0.84−2.05) | 1.66 (0.90−3.07) |
| Night shifts | 1.11 (0.73−1.67) | 1.26 (0.74−2.12) | 1.12 (0.72−1.74) | 1.28 (0.70−2.32) |
| History of depressive disorder | 3.77 (1.92−7.38) | 6.54 (3.14−13.62) | 3.41 (1.60−7.25) | 3.10 (1.27−7.56) |
| History of anxiety disorder | 2.76 (1.36−5.57) | 9.06 (4.44−18.50) | 1.47 (0.65−3.34) | 5.51 (2.36−12.90) |
| History of other mental disorder | 2.55 (0.56−11.56) | 8.06 (1.96−33.10) | 1.86 (0.38−9.19) | 3.29 (0.65−16.73) |
| COPD | 1.51 (0.73−3.14) | 1.50 (0.60−3.75) | 1.13 (0.52−2.48) | 1.00 (0.37−2.65) |
| Arterial hypertension | 1.37 (0.75−2.50) | 0.59 (0.22−1.59) | 1.36 (0.71−2.60) | 0.73 (0.26−2.11) |
| Immunodeficiency | 0.94 (0.23−3.81) | 1.90 (0.46−7.81) | 0.77 (0.18−3.33) | 1.60 (0.33−7.73) |
| Obesity | 0.97 (0.58−1.60) | 1.09 (0.58−2.04) | 0.92 (0.55−1.56) | 1.19 (0.60−2.35) |
| Smoking | 0.99 (0.43−2.29) | 1.11 (0.39−3.11) | 0.86 (0.36−2.11) | 0.90 (0.29−2.80) |
| People with whom they live | 1.06 (0.89−1.26) | 0.93 (0.73−1.17) | 1.02 (0.87−1.19) | 0.97 (0.79−1.20) |
| Lives with a person with a high risk of dying from COVID | 1.76 (1.15−2.69) | 1.79 (1.04−3.07) | 1.86 (1.19−2.91) | 1.74 (0.97−3.11) |
| Family member who is healthcare staff | 1.62 (1.07−2.47) | 1.03 (0.59−1.79) | 1.58 (1.01−2.47) | 1.11 (0.61−2.03) |
| Change of residence to avoid exposing family members | 1.94 (1.11−3.40) | 3.52 (1.87−6.61) | 1.99 (1.11−3.59) | 4.01 (1.99−8.09) |
| Contact with COVID patients | 1.16 (0.77−1.75) | 1.82 (1.06−3.13) | 1.06 (0.69−1.63) | 1.73 (0.96−3.11) |
| Personal protective equipment | 1.07 (0.52−2.21) | 0.91 (0.38−2.21) | 1.10 (0.51−2.35) | 1.13 (0.43−2.98) |
| Use of mass transport | 0.90 (0.60−1.36) | 1.32 (0.78−2.24) | 0.85 (0.55−1.32) | 1.14 (0.64−2.03) |
| Personal burnout | 1.00 (0.99−1.02) | 1.00 (0.98−1.02) | 1.00 (0.99−1.02) | 1.00 (0.99−1.02) |
| Work-related burnout | 1.01 (0.99−1.02) | 1.00 (0.98−1.02) | 1.01 (0.99−1.02) | 1.00 (0.98−1.02) |
| Patient-related burnout | 1.01 (1.00−1.03) | 1.00 (0.98−1.02) | 1.01 (1.00−1.03) | 1.01 (0.98−1.03) |
COPD: chronic obstructive pulmonary disease.
Although it was not the objective of this study, our frequency of moderate to severe anxiety symptoms was 15.2%, and for depression 18.3%. This is very much in line with that reported in other studies; the frequencies for any degree of anxiety symptoms are between 20 and 72% and for depressive symptoms, between 6 and 65%. When reported according to symptom intensity, the moderate forms of anxiety are between 5.7 and 32% and the severe ones between 1.9 and 60%; in depression, the moderate forms were between 4.8 and 40% and the severe ones between 0.3 and 35%.34–41 The high variability may be due to factors such as: the moment in the pandemic when the study was conducted, the type of contact with infected patients, the scales used and their cut-off points, the populations, and methodological problems, such as the non-representativeness of the majority of samples, most of which have been due to convenience. The studies which report higher frequencies of depression and anxiety are those conducted in areas of high prevalence of coronavirus at the start of the pandemic, and among front-line professionals.42,43 In a study conducted in a tertiary hospital in the United Kingdom with the same scales, highly similar data for depression and anxiety were found: symptoms of moderate anxiety in 12% and severe in 22%, and moderate in 6%, severe in 3% and highly severe in 6%.36 Figures similar to ours were also found in the study conducted between 1 March and 31 May 2020 in Medellín with the PHQ-9 and GAD-7 scales. They report symptoms of depression in 26%, moderate in 8.2%, moderately severe in 4.7% and severe in 1.7%. Anxiety was reported in 31.7%, moderate in 13.4%, and severe in 5.1% of the participants.6
As previously mentioned, measuring the prevalence was not the main objective of the study, and this should not be inferred from our data as the sampling was not based on probability, rather on convenience, and the response rate was low. Nonetheless, the moment in the pandemic when the study was conducted is important given that, as one lives with the disease, there is likely to be a sort of adaptation process, and the symptoms of anxiety and depression will be lower than at the start. This is possible as they could adapt to hospital response systems, more tools and information are acquired for patient care or as an inherent characteristic of human beings, who tend not to display the same emotional charge when exposed continuously to a stimulus.44
The participants were classified according to their symptoms of depression, anxiety and stress, and three classes were found corresponding to non-symptomatic participants (class I), with mild symptoms, or with moderate to severe symptoms of anxiety and depression (classes II and III); it was observed that the majority were located in class I, followed by class II.
In this model, it is found that the scores for fear of COVID-19 and perceived stress are higher in class III than in classes II and I. Even though one could think that fear of contagion with COVID-19 and perceived stress could act as triggering factors of emotional responses, the cross-sectional nature of this study does not allow us to establish a causal direction. It may also be the case that the presence of an anxious or depressive disorder increases the fear of contagion or perceived stress. In other studies, a positive association has been found with the scores reported in the fear of COVID-19 scale, for both depression and anxiety.45
Another association that was found in the study, which correlates with data found in other studies, is that there is a greater severity in symptoms in relation to fear of the risk of being infected, of being infected, and of infecting other people. In a study that included 1058 patients, Azoulay et al.46 reported, among other factors, that anxiety was associated with the fear of contagion, and depression was also related to the fear of infecting other colleagues.
One of the factors associated with belonging to class III (moderate and severe symptoms) was a history of having a diagnosis of anxiety and depression. Similarly, in the Turkish study by Elbay et al.,47 the presence of symptoms of anxiety and depression were found to be associated with having had a psychiatric disorder at some point in life (β = 6.00; 95% CI, 2.85–9.14). In the Chinese study by Zhu et al.48 an association was also found between history of mental disorder and more symptoms of anxiety and depression. These results lead us to think that patients with a history of prior mental disorders are a population more vulnerable to the psychological impact of COVID-19. In the study by Juhong et al.49 on first-line physicians in Gansu, it was reported that the history of depression or anxiety is a common risk factor to anxiety symptoms (T = –3.635; P < .001; 95% CI, –16.360 a –4.789) and symptoms of depression (T = –2.835; P = .005; 95% CI, –18.238 a –3.254).
Another factor associated with membership of class III is the need to change residence to protect their family members from contagion. This could be due to the additional isolation generated by being separated from the family nucleus and the fear of causing harm by infecting one of their loved ones.
It is striking that in this study no association was found with coming into contact with COVID-19 patients. In other studies, such as that of Cai et al.,50 which compared front-line workers versus clinicians with no direct exposure to infected patients, it was found that those on the front line had more anxiety (OR = 1.95; 95% CI, 1.46–2.61), and they also found that front-line workers presented with more depression, although the results were not conclusive. In the study by Buselli et al.,51 the scores for anxiety were associated with being a front-line worker and in intensive care.
Age is a risk factor that has been found to be associated with the presentation of symptoms of anxiety and depression; the majority of studies reported that being younger is associated with higher levels of anxiety and depression. In the Brazilian study by Civantos et al.,52 it was found that physicians had responses to the GAD-7 that differed significantly between the age groups, with higher scores in the youngest age group (25–44 years). Something similar was found in the study by Evanoff et al.,53 where subjects under 40 had higher scores. This is consistent with the present study, in which, for each year of increase in age, the possibility of belonging to class III dropped by 3%, and of belonging to class II by 6%.
Various studies have reported that being a woman is a risk factor for suffering greater levels of anxiety, depression and stress. For example, Lai et al.54 report that being a woman is a risk factor for depression (OR = 1.94; 95% CI, 1.26–2.98) and anxiety (OR = 1.69; 95% CI, 1.23–2.33). But in the case of the results reported here, this association was not compatible with these antecedents; one possible explanation for this difference with the other studies is that, in addition to care staff, this study includes administrative personnel (accounting for an important percentage), who are less exposed, and this may be reflected in a lower level of anxiety and depression.
Having suitable personal protection equipment is associated in the studies with a lower presence of depressive symptoms40 and being satisfied with the protective measures taken by the hospitals was associated with fewer symptoms of depression and anxiety,48 just as the absence of equipment was associated a greater risk of both depressive and anxiety symptoms.55 This association was not found here, which is due to almost all of the participants stating that they have suitable personal protection equipment.
An association between the years of experience or qualifications with the presence of depressive or anxiety symptoms has also been reported. In the study by Liu et al.,56 it was found that those participants who held senior posts had higher scores for depression than those with intermediate and junior posts (4.92 ± 6.03 vs. 4.41 ± 4.89 vs. 4.20 ± 5.07; P < .01). However, in another study, Song et al.57 found that depressive symptoms increased with fewer years of experience. But in this study, in a similar way to other studies conducted in high-complexity hospitals, no association was found between years of experience and symptoms of anxiety and depression.36
It is considered a strength of the study that it was conducted in hospitals that are referral centres for the treatment of patients con COVID-19. These institutions were in the department of Antioquia, one of the areas that was most affected by the pandemic, with a total of 561,985 confirmed cases of COVID-19 and 12,410 deaths up to the time of this review.58 Also considered to be a strength of study is the participation of healthcare personnel, which includes not only physicians and specialists, but also administrative and general services staff, making it possible to contrast the differences between these groups. Additionally, is the application of surveys in a second peak of the pandemic which makes it possible to identify how the risk factors are changing in comparison to other studies conducted at the start of the pandemic, and the application of scales that have been used in various studies around the world, which allows international comparisons to be made.
One of the limitations is that this study is cross-sectional, so it evaluates the presence of symptoms at a certain point in time, symptoms which may be temporary and may change as the circumstances of the pandemic change. Moreover, owing to the design of the study, it is not possible to establish causality between the factors associated with the onset of anxiety and depressive symptoms. Among the principal factors for having higher levels of psychopathology is a history of diagnosis of anxiety and depression. Being a cross-sectional study, and data from prior to the pandemic not being available, it is not possible to determine whether the symptoms are caused or worsened by COVID-19-related factors, or whether it is the underlying mental disorder. A further limitation of the study is the low rate of participation among the healthcare staff of the institutions. This is a problem that could result in selection biases, since the individuals who agree to respond to the questionnaire may not be representative of the entire population, and may be, for example, those who are suffering greater symptoms of anxiety and depression. Moreover, as it was conducted by email, it may have been the case that those participants using technology most were those who participated in the study, and they may be different in various aspects related with our objectives.
ConclusionsThe COVID-19 pandemic has had numerous consequences for the world, in the social, economic and political spheres, and has undoubtedly had an impact on health services in all countries. Healthcare personnel have been tasked with addressing the direct consequences of this global crisis; hence, it is to be expected that, as in the other epidemics and pandemics, the mental health of healthcare personnel has been affected.
The factors associated with membership of the group of persons with symptoms of anxiety and depression are: age, history of depressive disorders, living with a person with a high risk of dying from COVID-19, having a family member working in healthcare, and patient-related burnout. Conversely, the factors associated with membership of the group with moderate and severe symptoms of anxiety and depression are: age, history of depressive or anxious disorders and change of residence to avoid exposing family members. Some of these are factors that could be the cause or consequence of anxiety symptoms and could constitute an initial approach to designing interventions. Nonetheless, in order to be able to establish causal relationships that enable us to better understand the phenomenon, it would be desirable to have longitudinal studies.
FundingUniversidad de Antioquia [University of Antioquia], Medellín, Colombia.
Conflicts of interestNone.
We would like to thank the research committees of the School of Medicine at the University of Antioquia, the San Vicente Foundation University Hospital, and León XIII Clinic, as well as those individuals in the final two institutions who decided voluntarily to complete the survey.