This objective of this study is to examine the association between suicidal behaviour and substance use, depression, aggressiveness and borderline personality traits among adolescents from Sincelejo, a rural city in the north of Colombia.
MethodsThis cross sectional study included 352 participants selected by purposive sampling, from a public and a private school located in Sincelejo, Sucre district, in the north of Colombia. Students ages ranged from 12 to 18 years old (mean, 15.09±1.82). The participants completed three screening tools: a socio-demographic questionnaire, a screening instrument to collect information related to the frequency of use of some substances, such as tobacco and cannabis, and a self-report inventory to assess various personality and psychopathology domains. A series of t-tests, ANOVA and linear regression analyses were conducted.
ResultsPhysical aggression (t=7.74; p <0.01), cognitive depression (t=5.03; p <0.01), affective depression (t=8.24; p <0.01), affective instability (t=3.46; p <0.01), few social relationships (t=3.36; p <0.01), self-harm (t=3.45; p<.01), cannabis and tranquilizer use (t=2.83; p <0.05; and t=2.37; p <0.05) had a significant independent relationship with suicidal behaviour. Aggression (t=2.59; p <0.05), components of depression (t=9.03; p <0.01) and borderline personality traits (t=4.12; p <0.01) also predicted suicidal behaviour.
ConclusionsMore longitudinal studies are needed in this area to identify the causal relations between the factors studied and the suicidal behaviour of young people in Sincelejo.
El objetivo de este estudio es examinar la asociación del comportamiento suicida con el consumo de sustancias, síntomas depresivos, agresividad y rasgos de personalidad límite en adolescentes de Sincelejo (Sucre), una ciudad rural del norte de Colombia.
MétodosEste estudio transversal incluyó a 352 participantes seleccionados por muestreo intencional de una escuela pública y privada ubicada en Sincelejo, distrito de Sucre, en el norte de Colombia. Las edades de los estudiantes oscilaron entre los 12 y los 18 años (media, 15,09±1,82). Los participantes completaron 3 instrumentos de cribado: uno de datos sociodemográficos, uno sobre consumo de algunas sustancias, tales como tabaco y cannabis, y su frecuencia y un instrumento de autoinforme para evaluar varios dominios de la personalidad y algunas psicopatologías. Se realizaron una serie de pruebas de la t, ANOVA y análisis de regresión lineal.
ResultadosLa agresión física (t=7,74; p <0,01), el componente cognitivo de la depresión (t=5,03; p <0,01), el componente afectivo de la depresión (t=8,24; p <0,01), la inestabilidad afectiva (t=3,46, p <0,01), las pocas relaciones sociales (t=3,36, p <0,01), las autolesiones (p <0,01; t=3,45, p <0,01), el cannabis (t=2,83; p <0,05) y la toma de tranquilizantes (t=2,37; p <0,05), se asociaron con el comportamiento suicida. La agresión (t=2,59; p <0,05), los componentes de la depresión (t=9,03; p <0,01) y los rasgos de personalidad límite (t=4,12, p <0,01) predijeron el comportamiento suicida.
ConclusionesSe requieren más estudios longitudinales en esta área con el fin de identificar las relaciones causales entre los factores estudiados y el comportamiento suicida de los jóvenes en Sincelejo.
According to the World Health Organization, suicidal behaviors include suicidal ideations, planning, attempting suicide and completed suicide.1 The latter is considered the act of killing oneself voluntarily. Suicide is a serious public health problem that affects, persons who commit the act as well as their families, friends and the wider society.1 Suicidal behaviors are very complex and multifacetted with limited understanding of predictive indicators. Researchers and clinicians constantly investigate methods which can help them to identify and prevent persons from trying to end their own lives.2–4 As such, various aetiological theories and risk factors have been proposed regarding suicidal behaviors.
Durkheim posited that suicide is the result of the confluence of biological, psychological, social, economic and cultural factors.2,5 Joiner, in 2005, argued that in all cases of suicidal behaviors, there are three main tenets, the social isolation, perceived burdensomeness, and acquired capability, which must be present to enact self-harm.3 He proposed the Interpersonal Psychological Theory of Suicidal Behaviors, which states that individuals will not die by suicide unless they have the desire and the will to commit suicide. In order to develop the desire, one must experience social isolation and perceived burdensomeness. To overcome, the motivation of self-preservation, Joiner argued that one must have repeated exposure to self-harm behaviors.
In 1999, Mann et al. proposed the Stress-Diathesis Model of Suicidal Behavior, which postulates that the risk for suicidal behavior results from an interaction of neurobiological and psychopathology factors.6 Psychiatric disorders and psychosocial crises may establish the stress component of this model, while early childhood trauma as well as genetic factors may provide the diathesis element.
Suicidal behaviors are associated with psychiatric disorders, such as Major Depressive Disorder (MDD), Borderline Personality Disorder (BPD), Bipolar Affective Disorder (BAD) and Substance Abuse (SA), which lead to impaired judgment, impulsive actions and mood disturbance.7,8 Psychiatric disorders in adolescents are usually coupled with substance use.9–11 The use of alcohol and tobacco smoking are correlated with suicidal behaviors in adolescents.12–14 Furthermore, the blood alcohol levels and legal impairment caused by alcohol are strongly elevated in persons who commit suicide.15 Diatheses such as the psychological trauma associated with childhood abuse and neglect increases the risk of developing depression later in life and correlated suicidal behaviors.16 Some researchers have posited that exposure to childhood adversity is associated with increased aggressiveness, impulsivity, and substance abuse in later life.13,17 These sequelae may escalate suicidal behaviors by up to 4.3 times.18 While these theories are insightful, Cole-King et al. in 2017 asserted that identification of specific suicidal risks are more meaningful, than suicidal behavior theories, in identifying and preventing suicidal behaviors.19
Risk factors associated with suicidal behaviorPrevious research suggest that there are several risk factors for suicidal behaviors, including childhood abuse, neglect, depression (with hopelessness and worthlessness), the use of substances (such as alcohol), a history of prior suicide attempts and a family history of suicide.1,6,13,15–17,20–22 Multiple risk factors within the same individual have an additive, but not necessarily imminent effect on the probability of future suicidal behaviors.1
Researchers have determined that there are multiple executive functioning problems such as emotional (affective) dysregulation or instability and poor self control or impulsivity (leading to self-harm) that have produced pathways to suicidal behaviors in persons with borderline personality disorder.23 Le Gris et al., in a review article published in 2006, found that persons with borderline personality disorder (characterised by poor or unstable relationships, unclear or poor self image, affective —emotional— instability and aggression) are similar to other individuals who exhibit suicidal behaviors (with ideations and suicidal plans) because they both have common executive function deficits which lead to impaired decision making capacity.23
Previous suicide research in the Colombian populationIn Colombia, the crude suicide mortality rate per 100 000 population was 7.2 in 2016.24 Additionally, according to the World Health Organization (WHO), from 2000 to 2016 the suicide mortality rate in Colombia has remained at an average of 7.4.24 The risk factors for suicidal behaviors in the Colombian youth population are mainly related to gender (suicide itself is characteristic of males and suicide ideation of females), age,25–31 having an internalizing psychiatric disorder such as depression (which is more common in teeenagers from lower socioecnomic classes), or affective instablity, alcohol misuse, family dysfunction, aggression and poor quality of relationships, exposure to childhood sexual abuse leading to poor self image, neglectful parental style and authoritarian parenting.27,29,32–39
Research on youth in Sincelejo, ColombiaSincelejo is a city in the rural farming department of Sucre, near Columbia's northern coast line. Most of the population (over 90%) is Roman Catholic and the majority of the families are nuclear families with 2 parent headed homes.40,41 There are over 31 public schools and 14 private schools in Sincelejo.42 Similar to the rest of Colombia, approximately 20% of students attend private institutions. The private schools cater to wealthier households and are generally better equipped and staffed, and lead to better learning outcomes than the poorly funded public schools.43
Previous research demonstrated that youth in Sincelejo who perceived their caregivers’ parenting style as authoritarian or neglectful, or who attended public schools, reported higher levels of depression.44 Furthermore, teenagers in Sincelejo, who used tranquilizers and cannabis were more likely to report high levels of depressive symptoms.8 However, very little research has been done to demonstrate a relationship between suicidal behaviors and the components of depressive symptoms, substance use, aggression and borderline personality features among Sincelejo youth. It is important to understand these relationships in order to plan better preventative and intervention strategies for the youth of this rural city.
We hypothesized that there would be higher levels of suicidal behaviors among middle adolescent (15-16 years old) youth from Sincelejo who attended public schools or use tranquillizers and cannabis. We also hypothesized that students who reported higher levels on the components of depressive symptoms, greater levels of aggressive behaviors and borderline personality features would also report higher suicidal behaviors.
MethodsParticipantsOur cross-sectional study included 352 participants with an age range of 12 to 18 years-old (mean, 15.09±1.82) (table 1). Our sample contained almost 53% (n=186) boys and 47% (n=186) girls. Approximately 30% (n=104) of the students were chosen from a private high school, and 70% (n=248) from a public secondary school. The study participants were chosen by purposive convenience sampling, from a public and private secondary school located in Sincelejo, a district in Sucre, in the North of Colombia. The schools were selected to represent the students from the diverse socioeconomic background in the Sincelejo secondary student population. The public high school primarily registered students from the low-income families while the private school population consisted of middle- and upper-class pupils. Based on our G*Power sample size calculations, we conveniently chose 30 students from each school (public and private) for each age, 12 through to 18 years old, whose parents gave consent for their youngster to participate in this study.
Our inclusion criteria comprised students chosen from the 2 schools who were between 12 year and 18 years old, and whose parents gave consent for them to participate in the study. Our exclusion criteria comprised those students who were not chosen to participate in the project or whose parents did not give consent for them to participate in the study.
MeasuresAlcohol, Smoking and Substance Involvement Screening Test (ASSIST).45 This self-reporting screening tool collects information related to the frequency of use of the following substances: tobacco, alcohol, cannabis, cocaine, amphetamines, inhalants, tranquilizers or sleeping pills, hallucinogens and opioids and the health, social, family and legal issues related to those substances. It was developed by the World Health Organization (WHO) and has different linguistic versions, including Spanish.45 The WHO ASSIST contains 8 sections: the first assesses the lifetime use of the nine substances mentioned. The second part enquires about the frequency of the substance use during the last 3 months while the next 5 sections obtain information on issues related to the substances used, such as: health, social, family, economic and legal problems. The eighth section consists of only one question which asks if participants have ever used a drug by injection. The WHO ASSIST was validated in adolescents by Gryczynski et al.46 (2015). In the current study, substance use scores were calculated for each of the 9 substances by summing scores from questions 1 to 8 for each of the substances. Higher scores on each item suggests more problems related to the substance which the item refers to.
The Personality Assessment Inventory for Adolescents(PAI_A).47,56 It is a self-report inventory that assesses various domains of personality and psychopathology in adolescents between 12 and 18 years of age. This instrument contains 264 items divided into 22 scales, organized as follows: 4 scales of validity, 11 clinical scales, 5 scales regarding considerations for treatment and 2 scales of interpersonal relationships. Within 11 of these scales, there are specific subscales that allow a wide range of complex clinical constructs to be assessed. For the purposes of this study, we examined the following 11 clinical subscales: suicidal behaviors (despair, suicidal thoughts and suicide plans); aggressive attitude (hostility, little control of the expression of anger and belief in the instrumental utility of aggression); verbal aggression (verbal expressions of anger as well as the tendency to express anger to others); physical aggression (the tendency to physically manifest anger, by damaging property, get into physical fights and use threats of violence; cognitive dimension of depression (thoughts of hopelessness, worthlessness, indecisiveness); emotional dimension of depression (feelings of sadness, anhedonia); physiological dimension of depression (low levels of activity and energy, fatigue, changes in sleep patterns, appetite changes and weight loss); affective instability (emotional sensitivity, affective lability and poor emotional control); poor self-awareness (doubts about the main aspects of one's life, lack of objectives, the feelings of emptiness, feelings of de-realization); problematic interpersonal relationships (history of intense and ambivalent relationships in which the individual has felt betrayed and exploited), and lack of self-control (impulsivity in areas that have a high potential for negative consequences). For the purposes of our analyses, we included subscales 2-4 in the clinical dimensions of aggression grouping, subscales 5-7 in the components of depression and subscales 8-11 in the composite borderline personality features.
The subscale scores of the PAI-A 56 were obtained using standardized scores (t-scores) and e-profile online (http://www.teacorrige.com), an online software which provides immediate subscale scores, once the participants responses are entered into the program. The standardized t-scores which were used, have a mean of 50 and 1 standard deviation of 10. The internal consistency reliability was .79 with a test-retest stability coefficient of .78 for this sample.
Socio-demographic questionnaire. A self-reporting, data collection instrument was used to obtain socio-demographic information on participants’ school, grade, gender, and date of birth from each of the participants.
ProcedureDuring the spring and summer of 2017, research assistants provided a brief introduction to the participants of the study at the beginning of their regular class time. Participants were supervised by their class teacher as well as the research assistants, while the questionnaires were administered. Confidentiality was emphasized as well as the option to decline or withdraw from the process, at any time during the data collection. On average, students completed the study questionnaires in 40minutes. After submission, questionnaires were scrutinized to ensure that there were no unanswered questions.
Prior to commencement of the project, ethical approval was sought and obtained from the Research and Ethical Committee of the Corporación Universitaria del Caribe CECAR to conduct this study. The schools were chosen using purposive convenience sampling, to represent the high, middle and low socioeconomic classes of secondary schools in Sincelejo. Both school principals agreed to participate in the project and written informed consent was obtained from the parents of the participants. Additionally, written assent was obtained from the students who participated on the days of data collection. G*Power software was used to estimate the sample size and a minimum of 360 children were needed to give a confidence level of 95%, a 5% margin of error and medium effect size. Eight of the students who were chosen to participate were absent on the days of data collection.
Statistical analysesAn examination was done to determine the extent of missing data and no variable was missing more than 10% of the data. As such, we estimated the value for missing data and substituted values on each variable, with the exception of nominal data such as gender. Frequencies and mean average were calculated for substance use, depression and aggressiveness. After performing the Shapiro-Wilk test of symmetry, a value of .853 was obtained which was significant. However, because we used standardized t-scores in our analyses, we were able to perform independent t-tests and analyses of variance (ANOVA) which were used to investigate the relationship between sociodemographic variables and components of depression as well as dimensions of aggressiveness. A series of 2-stage hierarchal regression analyses were performed, firstly the background factors such as gender, school type and age were entered into the regression equation. Then, controlling for background factors, substances used, the components of depression, dimensions of aggression and borderline personality features were entered into the regression equation as predictors of suicidal behaviors.
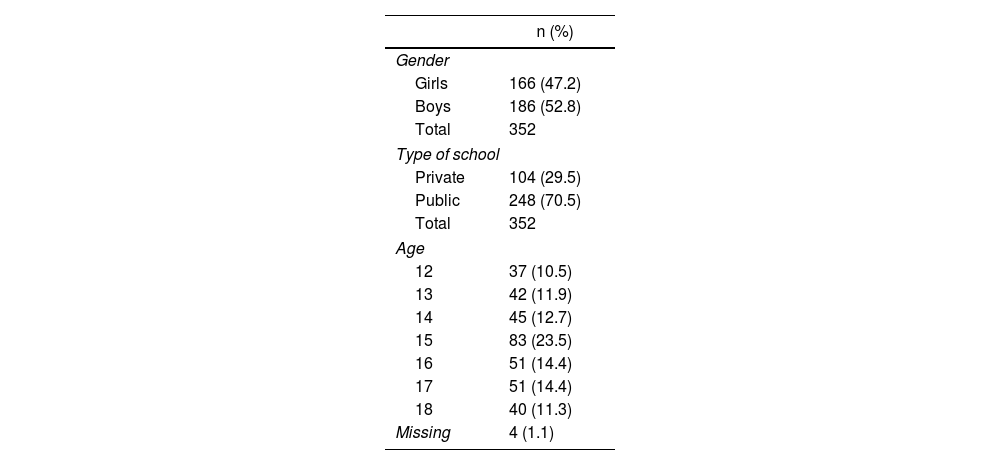
ResultsOver half of the participants in the study (54.8%, n=193) reported using a substance at least once in their lifetime. Of these substances, alcohol (32.6%), tobacco (13.6%), sedatives (2.8%) and cannabis (2.3%) were most frequently chronicled. Apart from these 4 substances, lifetime substance use of any of the other listed substances was less than 1% of the sample. There were generally no differences in the percentages of male and female students or students from public or private schools who had ever used one of the itemized substances from the ASSIST scale. The only difference which was noted was that 1 in every 2 students attending private schools (50.0%) reported they had ever used alcohol while only 1 in 4 students (25.4%) from public schools reported using alcohol (table 2).
Frequency of lifetime substance use by gender and type of school.
| Gender | Type of school | ||||
|---|---|---|---|---|---|
| Overall, n (%) | Male, n (%) | Female, n (%) | Public | Private | |
| Tobacco | 48 (13.6%) | 20 (10.8%) | 28 (16.9%) | 31 (12.5%) | 17 (16.3%) |
| Alcohol | 115 (32.6%) | 61 (32.8%) | 54 (32.5%) | 63 (25.4%) | 52 (50.0%)* |
| Cannabis | 8 (2.3%) | 4 (2.2%) | 4 (2.4%) | 5 (2.0%) | 3 (2.9%) |
| Cocaine | 2 (0.6%) | 2 (1.1%) | 0 | 2 (0.8%) | 0 |
| Amphetamines | 3 (0.8%) | 3 (1.6%) | 0 | 3 (1.2%) | 0 |
| Inhalants | 3 (0.8%) | 2 (1.1%) | 1 (0.6%) | 3 (1.2%) | 0 |
| Sedatives | 10 (2.8%) | 3 (1.6%) | 7 (4.2%) | 6 (2.4%) | 4 (3.8%) |
| Hallucinogens | 1 (0.3%) | 1 (0.5%) | 0 | 1 (0.4%) | 0 |
| Opioids | 1 (0.3%) | 1 (0.5%) | 0 | 1 (0.4%) | 0 |
| Other illegal drugs | 2 (0.6%) | 2 (1.1%) | 0 | 2 (0.8%) | 0 |
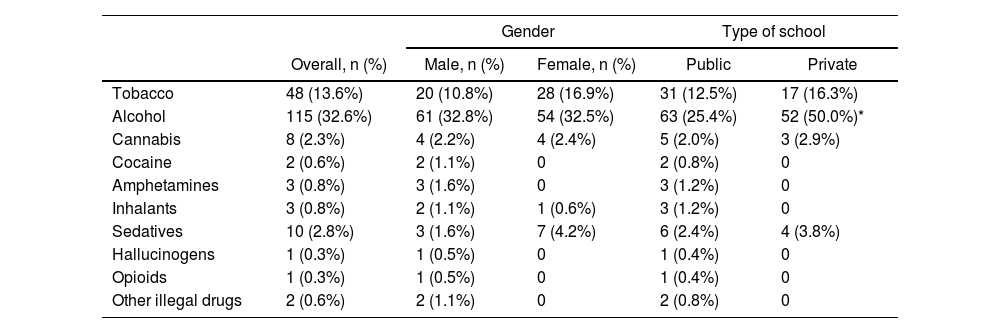
A series of t-tests were used to explore the differences in children's reported suicidal behaviors, dimensions of aggression and components of depression by their gender and school type. Mean depression score for the total sample was 56.26±8.39. Girls reported significantly higher levels of affective depression than boys (58.99±10.78; p<.01). Additionally, girls reported significantly higher aggressive attitudes (54.66±6.80; p<.01) and verbal aggressive scores (49.71±7.13; p<.01) than boys (table 3).
Mean suicidal behavior scores, depression scores and aggression scores by gender.
| Boys | Girls | t | p-value | |
|---|---|---|---|---|
| Suicidal behaviors | 53.02±9.60 | 53.66±11.38 | –.568 | .571 |
| Depression total | 55.59±7.96 | 57.02±8.81 | 1.602 | .110 |
| Cognitive depression | 52.66±9.58 | 53.63±10.02 | –.929 | .353 |
| Affective depression | 56.62±9.04 | 58.99±10.78 | –2.198 | .029* |
| Physiological depression | 54.95±8.34 | 55.36±8.70 | –.557 | .578 |
| Aggression total | 50.99±6.97 | 52.25±6.60 | –1.734 | .084 |
| Aggressive attitude | 52.52±7.50 | 54.66±6.80 | –2.799 | .005** |
| Verbal aggression | 48.14±6.75 | 49.71±7.13 | –2.122 | .035* |
| Physical aggression | 51.93±8.86 | 51.36±8.30 | .626 | .532 |
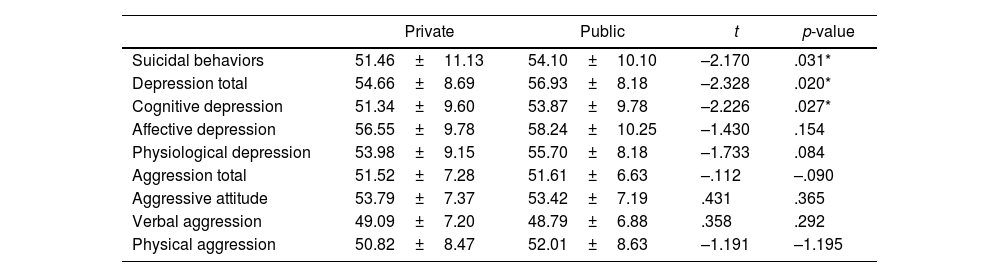
Individuals attending public school reported higher overall depression as well as cognitive depression scores than those attending private school. Public school adolescents (54.10±10.10) also reported higher levels of suicidal behaviors than those enrolled in private school (51.46±11.13; p<.05) (table 4).
Mean suicidal behavior scores, depression scores and aggression scores by school type.
| Private | Public | t | p-value | |
|---|---|---|---|---|
| Suicidal behaviors | 51.46±11.13 | 54.10±10.10 | –2.170 | .031* |
| Depression total | 54.66±8.69 | 56.93±8.18 | –2.328 | .020* |
| Cognitive depression | 51.34±9.60 | 53.87±9.78 | –2.226 | .027* |
| Affective depression | 56.55±9.78 | 58.24±10.25 | –1.430 | .154 |
| Physiological depression | 53.98±9.15 | 55.70±8.18 | –1.733 | .084 |
| Aggression total | 51.52±7.28 | 51.61±6.63 | –.112 | –.090 |
| Aggressive attitude | 53.79±7.37 | 53.42±7.19 | .431 | .365 |
| Verbal aggression | 49.09±7.20 | 48.79±6.88 | .358 | .292 |
| Physical aggression | 50.82±8.47 | 52.01±8.63 | –1.191 | –1.195 |
A series of one way ANOVAs were conducted to examine the differences by age of students’, their mean reported levels of suicidal behaviors, components of aggression, depression and borderline personality features (using adolescents’ responses to the PAI-A). Adolescents differed by age on the total depression scores such that 12 year olds reported significantly higher total depression scores than 18 year olds (F(6, 345)=2.14; p<.05). Adolescents significantly differed in their mean cognitive depression scores such that 12 and 13 year olds reported significantly higher levels of cognitive depression than 18 year olds (F(6,345)=2.67; p<.05). Similarly, 12 and 13 year olds reported significantly higher physiological depression scores than 18 year olds (F(6, 345)=2.99; p<.05).
Age differences were also found with the total aggression scores such that 16 year old reported significantly higher total aggression scores than 14 year olds and 18 year olds (F(6, 345)=2.42; p<.05).
In terms of verbal aggression scores, 16 year olds reported significantly higher levels of verbal aggression than 14 or 18 year olds (F(6,435)=3.76; p<.05). Finally, 16 year olds reported significantly higher physical aggression scores than 13 year olds (F(6,435)=2.39; p<.05).
There were no significant differences by age of mean suicidal behaviors (F(6,435)=0.51; p>.05).
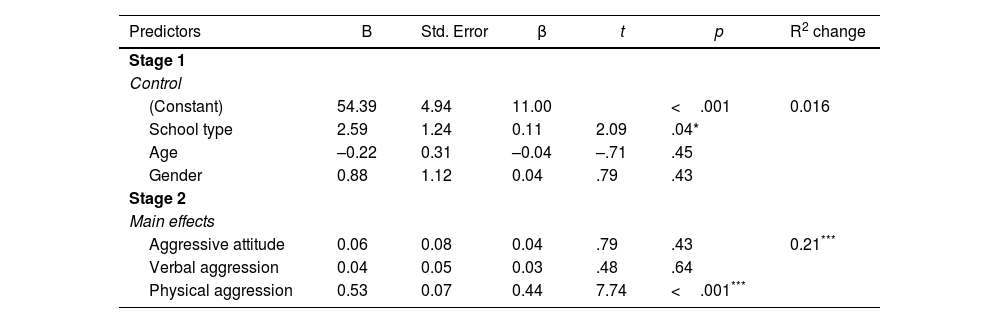
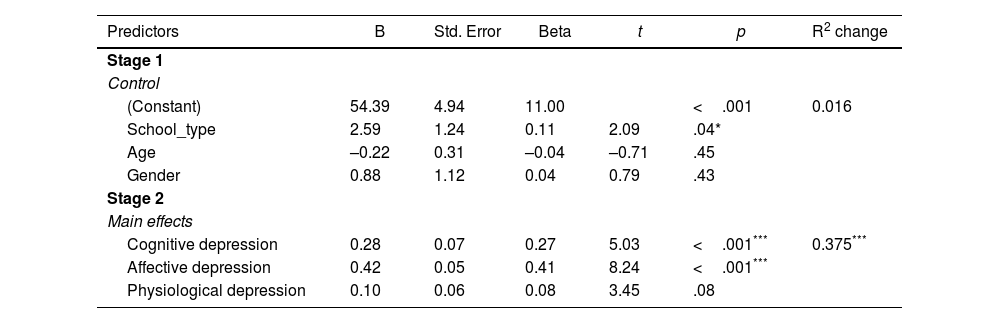
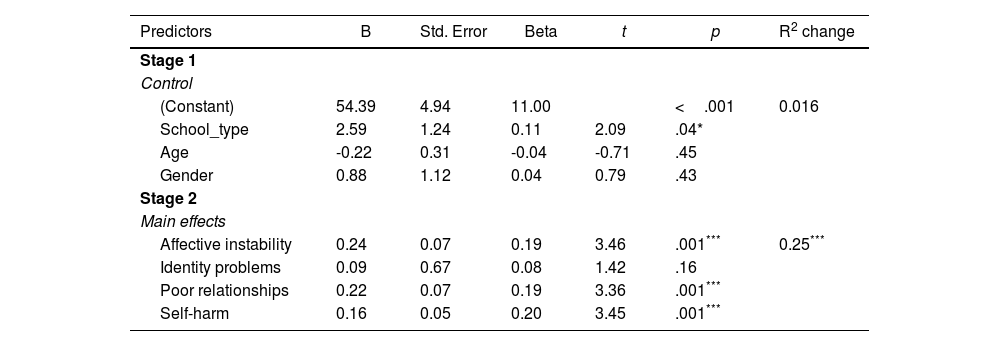
Components of aggressiveness, depression and borderline features of personality predicting suicidal behaviorsA series of 2-stage hierarchical linear multiple regression analyses were performed controlling for sociodemographic variables (students’ gender, age and school type). Separate regression analyses examining the students’ reported dimensions of aggression (table 5), components of depression (table 6), borderline personality features (table 7), overall dimensions of aggression, components of depression and borderline personality features (table 8) as well as the substances most commonly, ever used in their lifetime (table 9) as predictors of their reported suicidal behaviors were then conducted.
Linear regression analysis of dimensions of aggression predicting suicidal behaviors score, controlling for student's gender, school type, and age (n=352)**
| Predictors | B | Std. Error | β | t | p | R2 change |
|---|---|---|---|---|---|---|
| Stage 1 | ||||||
| Control | ||||||
| (Constant) | 54.39 | 4.94 | 11.00 | <.001 | 0.016 | |
| School type | 2.59 | 1.24 | 0.11 | 2.09 | .04* | |
| Age | –0.22 | 0.31 | –0.04 | –.71 | .45 | |
| Gender | 0.88 | 1.12 | 0.04 | .79 | .43 | |
| Stage 2 | ||||||
| Main effects | ||||||
| Aggressive attitude | 0.06 | 0.08 | 0.04 | .79 | .43 | 0.21*** |
| Verbal aggression | 0.04 | 0.05 | 0.03 | .48 | .64 | |
| Physical aggression | 0.53 | 0.07 | 0.44 | 7.74 | <.001*** | |
Multiple regression analysis of components of depression predicting suicidal behavior score, controlling for student's gender, school type, and age (n=352)**
| Predictors | B | Std. Error | Beta | t | p | R2 change |
|---|---|---|---|---|---|---|
| Stage 1 | ||||||
| Control | ||||||
| (Constant) | 54.39 | 4.94 | 11.00 | <.001 | 0.016 | |
| School_type | 2.59 | 1.24 | 0.11 | 2.09 | .04* | |
| Age | –0.22 | 0.31 | –0.04 | –0.71 | .45 | |
| Gender | 0.88 | 1.12 | 0.04 | 0.79 | .43 | |
| Stage 2 | ||||||
| Main effects | ||||||
| Cognitive depression | 0.28 | 0.07 | 0.27 | 5.03 | <.001*** | 0.375*** |
| Affective depression | 0.42 | 0.05 | 0.41 | 8.24 | <.001*** | |
| Physiological depression | 0.10 | 0.06 | 0.08 | 3.45 | .08 | |
Linear regression analysis of borderline personality features predicting suicidal behaviors score, controlling for student's gender, school type, and age (n=352)**
| Predictors | B | Std. Error | Beta | t | p | R2 change |
|---|---|---|---|---|---|---|
| Stage 1 | ||||||
| Control | ||||||
| (Constant) | 54.39 | 4.94 | 11.00 | <.001 | 0.016 | |
| School_type | 2.59 | 1.24 | 0.11 | 2.09 | .04* | |
| Age | -0.22 | 0.31 | -0.04 | -0.71 | .45 | |
| Gender | 0.88 | 1.12 | 0.04 | 0.79 | .43 | |
| Stage 2 | ||||||
| Main effects | ||||||
| Affective instability | 0.24 | 0.07 | 0.19 | 3.46 | .001*** | 0.25*** |
| Identity problems | 0.09 | 0.67 | 0.08 | 1.42 | .16 | |
| Poor relationships | 0.22 | 0.07 | 0.19 | 3.36 | .001*** | |
| Self-harm | 0.16 | 0.05 | 0.20 | 3.45 | .001*** | |
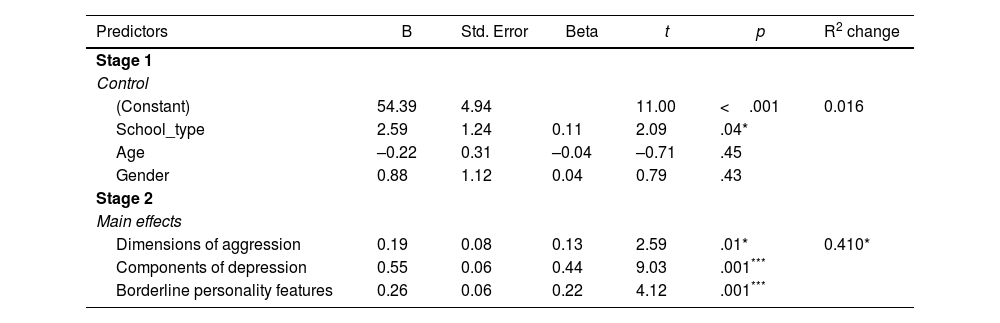
Linear regression analysis of dimensions of aggression, components of depression and borderline personality features predicting suicidal behaviors score, controlling for student's gender, school type, and age (n=352)**
| Predictors | B | Std. Error | Beta | t | p | R2 change |
|---|---|---|---|---|---|---|
| Stage 1 | ||||||
| Control | ||||||
| (Constant) | 54.39 | 4.94 | 11.00 | <.001 | 0.016 | |
| School_type | 2.59 | 1.24 | 0.11 | 2.09 | .04* | |
| Age | –0.22 | 0.31 | –0.04 | –0.71 | .45 | |
| Gender | 0.88 | 1.12 | 0.04 | 0.79 | .43 | |
| Stage 2 | ||||||
| Main effects | ||||||
| Dimensions of aggression | 0.19 | 0.08 | 0.13 | 2.59 | .01* | 0.410* |
| Components of depression | 0.55 | 0.06 | 0.44 | 9.03 | .001*** | |
| Borderline personality features | 0.26 | 0.06 | 0.22 | 4.12 | .001*** | |
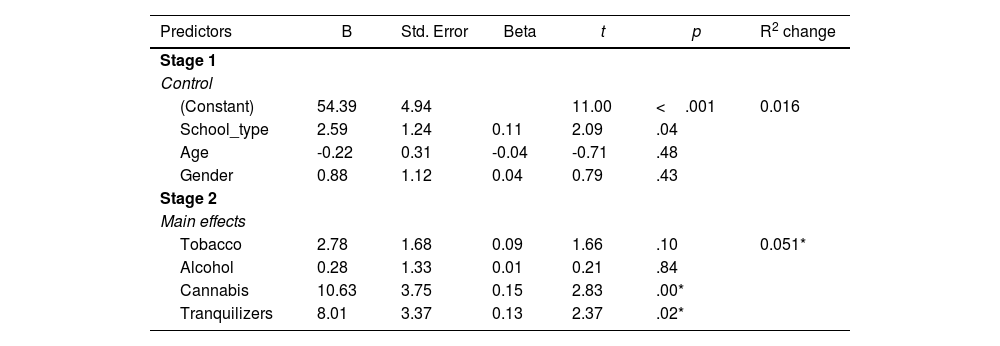
Ever in lifetime use of alcohol, tobacco and tranquilizers predicting suicidal behaviors (n=352).
| Predictors | B | Std. Error | Beta | t | p | R2 change |
|---|---|---|---|---|---|---|
| Stage 1 | ||||||
| Control | ||||||
| (Constant) | 54.39 | 4.94 | 11.00 | <.001 | 0.016 | |
| School_type | 2.59 | 1.24 | 0.11 | 2.09 | .04 | |
| Age | -0.22 | 0.31 | -0.04 | -0.71 | .48 | |
| Gender | 0.88 | 1.12 | 0.04 | 0.79 | .43 | |
| Stage 2 | ||||||
| Main effects | ||||||
| Tobacco | 2.78 | 1.68 | 0.09 | 1.66 | .10 | 0.051* |
| Alcohol | 0.28 | 1.33 | 0.01 | 0.21 | .84 | |
| Cannabis | 10.63 | 3.75 | 0.15 | 2.83 | .00* | |
| Tranquilizers | 8.01 | 3.37 | 0.13 | 2.37 | .02* | |
Controlling for the background sociodemographic variables, the students’ reported levels of aggressive attitude, verbal aggression and physical aggression, as a group (table 5) were significant predictors of suicidal ideation (R2 change=0.21) with only the reported physical aggression scores having a significant independent relationship (t=7.74; p<.01) with suicidal behaviors.
After the background sociodemographic variables were controlled, the students’ reported levels of cognitive depression, affective depression and physiological depression scores, as a group (table 6) were significant predictors of suicidal ideation (R2 change=0.38) with the cognitive depression and affective depression scores, each having a significant independent relationship (t=5.03; p<.01; and t=8.24; p<.01) with suicidal behaviors.
Regarding the independent variables comprising the cluster of borderline personality features (affective instability, self-identity problems, poor relationships and self-harm), background sociodemographic variables were again controlled, and our findings showed students’ reported levels of affective instability, self-identity problems, poor relationships and self-harm as a group (table 7) were significant predictors of suicidal ideation (R2 change=0.25) with the affective instability, poor relationships and self-harm scores, each having a significant independent relationship (t=3.46; p<.01; t=3.36; p<.01; and t=3.45; p<.01) with suicidal behaviors.
Similarly, we controlled the background sociodemographic variables, and found that the students’ reported overall scores for all dimensions of aggression, all components of depression and composite borderline personality features scores as a group (table 8) were significant predictors of suicidal ideation (R2 change=0.41) with the dimensions of aggression, components of depression and composite borderline personality features scores each having a significant independent relationship (t=2.59; p<.05; t=9.03; p<.01; and t=4.12; p<.01) with suicidal behaviors.
Finally, after controlling for the background sociodemographic variables, the students’ reported uses of alcohol, tobacco, cannabis or tranquilizers, ever in their lifetime (table 9) were significant predictors of suicidal ideation as a group (R2 change=0.05) with only cannabis and tranquilizer use, each having a significant independent relationship (t=2.83; p<.05; and t=2.37; p<.05) with suicidal behaviors.
DiscussionThis study mainly aimed to examine the association of suicidal behavior with substance use, depression, aggressiveness, and borderline personality features among adolescents from Sincelejo, a rural city in the North of Colombia. Guided by the clinical stress-diathesis model of suicide proposed by Mann et al., we decided to examine these four aspects of Colombian adolescents.6 This model suggested that suicidal behaviors are associated with a predisposition or diathesis to experience high levels of impulsiveness and aggressiveness. The existence of a stressor, that could be a psychiatric disorder such as depression, substance use or borderline personality disorder, increased the risk of those suicidal behaviors. This study examined some of the critical dimensions in some of these factors to observe the level of prediction of each dimension separately.
Our study confirmed the 2 hypotheses in that: a) we found higher levels of suicidal behavior among middle adolescent (15-16 years old) from Sincelejo who attended public schools or use tranquillizers and cannabis, and b) students who reported higher levels of the components of depressive symptoms, greater levels of aggressive behaviors and borderline personality features also report higher levels of suicidal behaviors. The factors associated with elevated levels of suicidal behavior were using cannabis and tranquilizers at some time in their lifetime, experiencing affectively instability, having mainly cognitive or affective symptoms of depression, exhibiting physically aggressiveness, engaging in self-harm activities, and having poor quality of relationships.
Suicidal behaviors and cannabis and tranquilizer lifetime useIn keeping with our hypotheses, we found that cannabis and tranquilizers use predicted suicidal behaviors, not alcohol use as was mentioned in previous Colombian and international youth suicide research.13,14,20,48–50 This is in keeping with Borges et al., who found that cannabis use and an early diagnosis of drug use increased the risk ratio of suicide ideations.20 Furthermore, they found that only those adolescents who began the alcohol consumption before age 15 had a higher risk of suicide attempt. The social acceptability associated with alcohol use among Sincelejo teenagers and the wider Sucre society may provide a possible reason for this finding. Sincelejo youth who consume minimal to moderate quantities of alcohol, in social contexts are generally accepted.8,51 Additionally, earlier findings demonstrated that Sincelejo adolescents who use cannabis and tranquilizers were significantly more depressed that their no-user peers.8 Brodsky et al. previously mentioned a strong correlation between substance use, depressive disorder and suicidal behaviors among adolescents.7 It's possible that the youth from our study who use cannabis and tranquilizers were more depressed and eventually develop suicidal behaviors.
Suicidal behaviors and depressionDepression is more common among post pubertal girls in Colombia and is associated with suicidal behaviors.52,53 In accordance with past literature, our study found that girls were more depressed than boys.8,52,53 More specifically, the girls in our study reported higher affective depression scores. Our results are consistent with those found by Pérez-Olmos et al. in 309 adolescents from 3 secondary schools in Bogotá (Colombia).51 They found that the probability of having depression or suicidal behavior was associated with being a girl.
In keeping with our hypotheses, public school attendees (boys and girls) reported higher suicidal behaviors as well as greater cognitive and total depression scores. Researchers have found strong correlations between social class, depression and suicidal behaviors among children and adolescents.54 This may be due to neighbourhood factors of crime and violence as well as the lack of basic amenities such as adequate school supplies, lack of running water, food and proper shelter.
Furthermore, in our study, higher affective and cognitive depressive scores were predictive of greater suicidal behaviors. Reminiscent of Caribbean adolescents depression research, we found that Colombian teenagers from Sincelejo reported mainly cognitive-affective components of depression.55 Lewinsohn et al. said that the cognitive components of depression occur in the later stage of the illness, and were more reflective of severe depression, which is manifested by suicidal behaviors and cognitive deficits.56 It is possible that adolescents from Sucre, on the Caribbean coast, as well as teens from the wider Caribbean communities, especially those from lower socioeconomic classes, may suffer quietly with depression for a longer period of time before getting profession attention.
Suicidal behaviors, aggressiveness, borderline personality features and stress-diathesis modelConsistent with our findings that physical aggression, affective instability, having poor quality of relationships and engagement in self-harm activities all correlate with suicidal behaviors in Sincelejo youth, previous research has suggested that individuals with suicidal behaviors show high levels of aggressiveness, affective (emotional) instability, poor self-control (impulsiveness), self-harm behaviors and poor family relationships.13,17,32,39,57,58 The research team of Zhang et al. found that high levels of aggressiveness were risk factors for 3 types of suicidal behavior (suicide ideation, plans and attemps) in a large sample of 16 271 adolescents.57 Zhang et al. posited that aggression, impulsive and self-harm behaviors are the result of genetic factors or early experiences of childhood adversity, which form the diathesis or framework in the stress-diathesis model for suicidal behavior.57
In our research, we used 3 subscales to measure aggressiveness: physical aggression, aggressive attitude and verbal aggression. Physical aggression, but not aggressive attitude and verbal aggression, predicted suicidal behaviors. In this study the physical aggression subscale, focused on the tendency to manifest anger using physical means such as damaging property and physical fights, while aggressive attitude and verbal aggression focused on more covertly on belief in use of aggression and the use of words to express anger.
Conner et al. explained that persons with the personality features of aggression/hostility and impulsivity, experience more affective instability and engage in self-harm behaviors which tend to cause more problematic interpersonal relationships.17 As a result, they have less support and experience more social isolation and psychosocial stress, leading to depression and increased anxiety, hence completing the stress-diathesis model related to suicidal behavior.
Risk factors for suicidal behaviorsComparable with previous research, we observed that the risk factors associated with suicidal behaviors, in our study, were use of cannabis or tranquilizers, cognitive and affective components of depression.15,16,20–22,52,53. In addition, our findings also reported that suicidal behaviors are related to the borderline personality features of emotional (affective) instability, engagement in physical aggression, impulsive self-harm behaviors and poor quality of relationships. Le Gris et al. also included those risk factors in their research and explained that there are similar multiple executive function issues which lead to both borderline personality features and suicidal behaviors.23
We believe that our findings will assist clinicians, managing youth from Sincelejo, as well as the wider Colombian adolescent population, to better identify teens at risk for suicide and organize more effective prevention strategies. The strategies should target parents, educators and the youth themselves, to minimize the risk teenagers’ substance use as well as identify depression and personality features which may lead to suicidal behaviors.
Finally, financial and social assistance for the vulnerable adolescents from lower socioeconomic classes may also assist in decreasing teen suicidal behaviors. Consistent with Cole-King et al.,19 our research has contributed to the identification of risk factors that increase suicidal behaviours, which will improve our understanding of adolescent suicidal behaviours.
LimitationsThis is a cross-sectional study therefore we could not derive causal relations among variables. However, despite this limitation, based on this research in the community of Sincelejo, Sucre (Colombia), where, to our knowledge, this type of research is extremely sparse, we now understand more about the association of youth suicidal behaviors, with social class, cannabis and tranquilizer use, borderline personality features and internalizing disorders. It is possible that our findings may help to inform more effective prevention and treatment programs for youngsters in this community.
ConclusionsAmong the youngsters of Sincelejo, Columbia, their use of cannabis, tranquillizers as well as levels of components of depression, aggression and borderline personality features were associated with their reported levels of suicidal behaviors. Additionally, social class is associated with their levels of suicidal behaviors. More robust longitudinal research is needed in this area to identify causal relations between these factors and Sincelejo youth suicidal behaviors.
Author contributionsDr. K. Romero-Acosta and S. Verhelst conceived the paper and oversaw data collection, conducted data analysis, and wrote the initial version of this manuscript. J. Restrepo and L. Fonseca assisted with writing the initial version of this manuscript. At the invitation of Dr. Romero-Acosta, Dr. G. Lowe and Professor G. Lipps re-analysed the data and interpreted the findings of this revised version of the paper. Dr. G. Lowe and Professor G. Lipps also re-wrote the method, results and discussion sections as well as portions of the introduction. They also approved this final version of the manuscript.
Conflicts of interestsThere are no conflicts of interests in this study.
This study was supported by a grant from the Corporación Universitaria del Caribe CECAR. The authors thank the study participants, project staff, and research assistants. Also, we would like to thank our research assistant Diego Pérez for his effort in collecting parents and children data. We would further like to thank Janelle Green from The University of the West Indies, Mona, for her assistance with editing and formatting the tables.