Psychological morbidity assessments are of interest since mental health is part of a person's overall health and early detection promotes emotional well-being.
AimTo determine the association between common mental disorders and related factors in dental students from Cartagena, Colombia.
MethodsWe conducted a cross-sectional study in 858 dental students from Cartagena, Colombia; who answered a structured anonymous self-report questionnaire to assess the presence of common mental disorders (CMD) (General Health Questionnaire-12), problematic alcohol consumption (CAGE), sociodemographic and other related variables. Data were analysed using descriptive statistics and bivariate analysis was conducted later using χ2 tests. The strength of association was obtained with prevalence ratios (PR) and 95% confidence intervals (95%CI). Finally adjusted PRs, and 95%CIs were obtained using a log-binomial regression model. Statistical analysis was performed using Stata v.13.2 for Windows (Stata Corp.; TX, USA).
ResultsThe average age was 20.8±3.01 years of age, and more than half were females. CMD overall prevalence was 30.3% (95%CI, 27.3–33.5). The regression model suggested as associated factors: sex (PR, 1.54; 95%CI, 1.21–1.96), recent economic changes (PR, 1.70; 95%CI, 1.37–2.12), family conflicts [PR, 2.29; 95%CI, 1.89–2.77), abandonment (PR, 1.58; 95%CI, 1.23–2.03), history of abuse (PR, 2.05; 95%CI, 1.27–3.31), and problematic alcohol consumption (PR, 1.35; 95%CI, 1.02–1.78).
ConclusionsCMD prevalence was high. Being female, family conflicts, history of abuse and problematic alcohol consumption are considered as risk factors for CMD development and should be carefully assessed to predict emotional well-being.
La valoración de morbilidad psicológica resulta de interés porque la salud mental hace parte de la salud integral de un individuo, y la detección precoz de casos propende al bienestar emocional.
ObjetivoEstimar la asociación entre trastornos mentales comunes y factores relacionados en estudiantes de Odontología de Cartagena, Colombia.
MétodosEstudio de corte transversal en 858 estudiantes de Odontología de Cartagena, Colombia, que respondieron a un cuestionario estructurado anónimo autoaplicado para evaluar la presencia de TMC (Cuestionario General de Salud-12), consumo problemático de alcohol (CAGE), variables sociodemográficas y otras relacionadas. Se realizó estadística descriptiva y análisis bivariable con pruebas de la χ2. La fuerza de asociación se computó con razones de prevalencia (RP) e intervalos de confianza del 95% (IC95%). Con regresión log-binomial, se obtuvieron RP e IC95% ajustados. El análisis se realizó empleando Stata v.13.2 para Windows (Stata Corp.; College Station, Texas, Estados Unidos).
ResultadosEl promedio de edad fue 20,8±3,01 años y más de la mitad eran mujeres. La prevalencia de TMC fue del 30,3% (IC95%, 27,3–33,5). El modelo de regresión indicó como factores asociados: sexo (RP, 1,54; IC95%, 1,21–1,96), cambios económicos recientes (RP, 1,70; IC95%, 1,37-2,12), conflictos familiares (RP, 2,29; IC95%, 1,89-2,77)], abandono (RP, 1,58; IC95%, 1,23-2,03), historia de abuso (RP, 2,05; IC95%, 1,27-3,31) y consumo problemático de alcohol (RP, 1,35; IC95%, 1,02-1,78).
ConclusionesLa prevalencia de TMC fue alta. Ser mujer y tener conflictos familiares, historia de abuso y consumo problemático de alcohol son factores de riesgo de TMC y deben ser cuidadosamente evaluados para la predicción del bienestar emocional.
Common mental disorders (anxiety, depression and somatoform disorders), also known as minor psychiatric disorders, are mild psychic problems that over the years can have a huge social and biophysical impact if they are not detected early.1 They include symptoms such as fatigue, insomnia, memory lapses, difficulty concentrating, irritability and somatic manifestations.2 They may also indicate psychiatric suffering and lead to more serious mental disorders, which take on new importance in the case of healthcare professionals, due to their role in caring for the population.3
Studying Dentistry is a challenge and often requires students to use mental resources that decrease their psychological resilience and make them susceptible to poor states of physical and mental health.4,5 Compared to the general population, dental students report levels of anxiety and depression which are a few times higher.6,7 In Colombia, Divaris et al.8 in 2013 indicated alarming levels of psychological distress (PD) among dental students in a multicentre study. They also described multiple related trigger factors for PD, such as gender, class, sources of financial support and curriculum characteristics. Moreover, some factors, such as having children and working at the same time, or even clinical rotations, may overload these students and make them more susceptible to psychiatric outcomes such as burnout or even lead to suicidal ideation.7
Previous local studies on symptoms of depression, anxiety and stress in dental students at a public university reported a prevalence of 37.4%, 56.6% and 45.4%, respectively, which are alarming figures in a context that should not cause PD in students. There are a significant number of studies which have examined the main roots of this phenomenon among dental students. Situations such as a lack of support from friends, family dysfunction and financial difficulties are usually described as being linked to the onset of symptoms.9 The results of research on the mental health of dental students are far from encouraging and agree on the need for a favourable academic environment.10 Most of these studies have focussed their efforts on studying the causes, but few have focussed on studying the occurrence of triggers such as common mental disorders, assessed as a single trigger but not individually, and other factors such as personal environment, which may be related. In this context, mental health research in dental students takes on new importance, since it guarantees adequate knowledge and the possibility of intervening early on in order to avoid negative consequences on their states of health and to ensure their future wellbeing.
In consideration of the foregoing, the objective of this study was to describe the prevalence of common mental disorders in dental students and to estimate the association with personal (familial and financial) and academic factors.
MethodsA cross-sectional study on a population of dental students from three faculties in Cartagena, Colombia. Due to the fact that the study population is deemed to be defined geographically and temporally, and is easy to reach, no sample size calculation was performed. Thus, through a census, we determined the presence of common mental disorders and related factors.
This research was conducted in accordance with the ethical regulations applicable in Colombia (Resolution 008430 of 1993) and worldwide (Declaration of Helsinki, revised in Edinburgh, 2000), and was endorsed by the University of Cartagena Research Ethics Committee. Through a written informed consent form, the students expressed their willingness to take part and the risks, confidentiality guarantee and anonymity of information were explained to them.
To take part in the research, the students had to be enrolled and academically active in the second academic period of 2014 and the first period of 2015 and voluntarily declare their participation. The Academic Department of each Faculty of Dentistry was asked for a full list of students per semester and surveys were then carried out in lectures, where we hoped they would be completed in full.
For information gathering, a self-applicable and anonymous questionnaire was used, containing 16 questions with polytomous responses, designed based on the existing theory. Two judges assessed its face validity, taking into account its relevance, the adequacy of the categories, plausibility, semantics, syntax and structuring of the items.
The form comprised a questionnaire and two scales. The questionnaire included sociodemographic characteristics such as age, gender (male, female), semester or academic cycle (clinical 6–10 and basic 1–5), marital status (married, consensual union, separated, and single), children (yes, no) and professional activity (yes, no). Other aspects related to the student's role within the university institution were also assessed, such as academic status (regular when no modules in their academic record have been failed and they attend all possible modules for the cycle in which they are enrolled; irregular if they have failed a module as per their academic record or they have dropped one), lack of time to relax (yes, no), recent financial difficulties (yes, no) and relationship problems with friends, a partner or spouse (yes, no), history of abuse or maltreatment (yes, no) and having been or being a victim of some form of abuse (yes, no). The alcohol abuse assessment was performed with the CAGE scale, which consists of four questions on the perceived need to cut down on drinking (C), social criticism (A), feelings of guilt (G) and morning consumption (E), assessed with dichotomous responses. Answering “yes” to two or more questions is considered to indicate a high probability of alcohol abuse. The psychometric properties of the scale have been described in the Colombian population with a sensitivity of 66.7% (95% confidence interval [95%CI], 38.8–87.0%) and internal consistency between 0.753 and 0.834.11
Common mental disorders (CMDs) were assessed using the 12-item General Health Questionnaire (GHQ-12), an instrument designed to assess emotional symptoms, psychological wellbeing and CMDs in adolescents and adults; the 12-point version is preferred due to its short length and faster administration.12 It consists of 12 questions (six worded positively and six worded negatively) which are generally assessed on a Likert-type scale exploring symptoms in the past month, traditionally with a four-option ordinal response pattern varying from never to always (0-1-2-3). However, for this study, the originally-proposed binary score system was chosen (0-0-1-1), which suggests a one-factor structure. To identify possible cases, 4 was determined as the cut-off point.12 The psychometric properties of the GHQ-12 have been described previously in the Colombian population, indicating an internal consistency for the ordinal and dichotomous scoring systems of 0.779 and 0.708, respectively.13
ProcedureUse of the instrument was subjected to a pilot test with a group of students who shared similar characteristics; two trained research assistants took part as the interviewers, who requested the students’ voluntary collaboration and guaranteed the anonymity and confidentiality of the information. Moreover, the questionnaires also went through auditing and monitoring phases, including a review by the investigators during data gathering to assess the interviewers’ adherence to the operational protocols, as described in a previously published article.14
Once the information had been gathered, it was subsequently digitised and a matrix table was created with the software package Microsoft Excel v.2010 for Windows. In order to minimise errors, double digitations were performed, with periodic checks by one of the investigators.
Statistical analysisAssumptions of normality were initially verified for continuous variables using the Shapiro–Wilk test. The descriptive analysis was initiated with descriptive statistics for all the variables being studied. If the data were normally distributed, the mean±standard deviation were reported for continuous variables; otherwise, the median [interquartile range] was reported. For the qualitative variables, frequencies and percentages were reported with their 95% CIs. The inferential analysis involved exploring associations using the χ2 test. Subsequently, to calculate the strength of association, prevalence ratios were obtained with adjusted estimators using a multivariate analysis and 95%CI through log-binomial regression. The decision to use log-binomial regression instead of logistic regression was based on the fact that odds ratios (ORs) derived from logistic regression tend to overestimate the true size of the effect when the outcome is common (>20%) and the prevalence ratios are also quickly interpretable, compared to ORs in cross-sectional studies.15
Psychometric properties of the GHQ-12Through the exploratory factor analysis, the factor structure was estimated for the GHQ-12 within the context of this study by using binary scoring with principal factors with oblique rotation (promax). Moreover, using a sedimentation graph, the number of factors to be retained and the proportion of variance explained were determined. Inspection of the sedimentation graph shows a better performance than other criteria (Kaiser, eigenvalues≥1).16,17
To determine construct validity (CV), confirmatory factor analysis (CFA) was used, assessing the model fit obtained in the exploratory phase: one-dimensional with response bias correction using the binary scoring system. Fit indices for this model were then obtained: χ2, degrees of freedom, root mean square error of approximation (RMSEA) and confidence interval of 90% (90%CI), comparative fit index (CFI) and Tucker–Lewis index (TLI). Using the criteria proposed by Hu and Bentler, the fit of the model was deemed acceptable if: χ2p>0.05, RMSEA≤0.06, CFI≥0.95 and TLI≥0.95.18
Finally, internal consistency was estimated using the Kuder–Richardson formula-20.19
The descriptive, inferential and factor analysis were performed using Stata v.13.2 for Windows (StataCorp.; College Station, TX, USA) and CFA was performed using Mplus v.7.31 (Muthén & Muthén, Los Angeles, CA, USA).
ResultsOf the total 1072 students enrolled on Dentistry programmes (undergraduate and postgraduate), 858 were included in the study. The remaining students were difficult to locate, did not agree to take part in the study or did not correctly complete the data collection instrument. With this in mind, the total participation rate was 80%.
Population characteristicsThe sample mostly consisted of females (66.2%) with an average age of 20.8±3.01 years, from basic cycle semesters (53.6%) and belonging to the middle socioeconomic class (49.7%).
Psychometric properties of the GHQ-12The indicators of fit obtained in the CFA for the one-dimensional structure with response bias correction were: χ2, p=0.15; RMSEA=0.035; CFI=0.982 and TLI=0.966. The internal consistency of the scale, on the other hand, was 0.74.
Prevalence of common mental disorders and related factorsThe total prevalence of CMDs using the GHQ-12 was 30.3% (95%CI, 27.3–33.5).
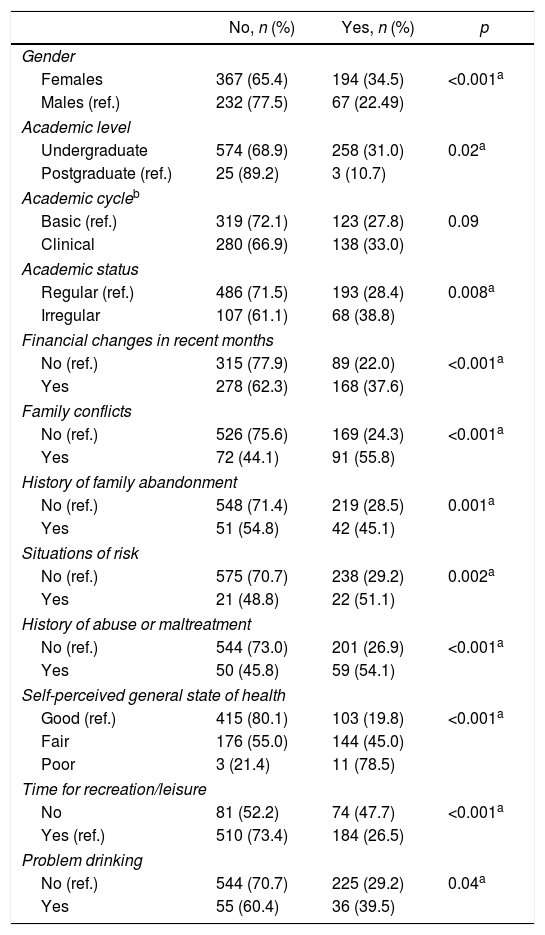
Table 1 shows the bivariate analysis between the presence of CMDs and diverse factors. With crude estimators, statistically significant associations were observed between CMDs and gender, academic level, academic status, financial changes in the past month, family conflicts, a history of family abandonment, situations of risk, a history of abuse or maltreatment, self-perceived state of health, recreation time and problem drinking.
Occurrence of factors and their relationship with common mental disorders.
| No, n (%) | Yes, n (%) | p | |
|---|---|---|---|
| Gender | |||
| Females | 367 (65.4) | 194 (34.5) | <0.001a |
| Males (ref.) | 232 (77.5) | 67 (22.49) | |
| Academic level | |||
| Undergraduate | 574 (68.9) | 258 (31.0) | 0.02a |
| Postgraduate (ref.) | 25 (89.2) | 3 (10.7) | |
| Academic cycleb | |||
| Basic (ref.) | 319 (72.1) | 123 (27.8) | 0.09 |
| Clinical | 280 (66.9) | 138 (33.0) | |
| Academic status | |||
| Regular (ref.) | 486 (71.5) | 193 (28.4) | 0.008a |
| Irregular | 107 (61.1) | 68 (38.8) | |
| Financial changes in recent months | |||
| No (ref.) | 315 (77.9) | 89 (22.0) | <0.001a |
| Yes | 278 (62.3) | 168 (37.6) | |
| Family conflicts | |||
| No (ref.) | 526 (75.6) | 169 (24.3) | <0.001a |
| Yes | 72 (44.1) | 91 (55.8) | |
| History of family abandonment | |||
| No (ref.) | 548 (71.4) | 219 (28.5) | 0.001a |
| Yes | 51 (54.8) | 42 (45.1) | |
| Situations of risk | |||
| No (ref.) | 575 (70.7) | 238 (29.2) | 0.002a |
| Yes | 21 (48.8) | 22 (51.1) | |
| History of abuse or maltreatment | |||
| No (ref.) | 544 (73.0) | 201 (26.9) | <0.001a |
| Yes | 50 (45.8) | 59 (54.1) | |
| Self-perceived general state of health | |||
| Good (ref.) | 415 (80.1) | 103 (19.8) | <0.001a |
| Fair | 176 (55.0) | 144 (45.0) | |
| Poor | 3 (21.4) | 11 (78.5) | |
| Time for recreation/leisure | |||
| No | 81 (52.2) | 74 (47.7) | <0.001a |
| Yes (ref.) | 510 (73.4) | 184 (26.5) | |
| Problem drinking | |||
| No (ref.) | 544 (70.7) | 225 (29.2) | 0.04a |
| Yes | 55 (60.4) | 36 (39.5) | |
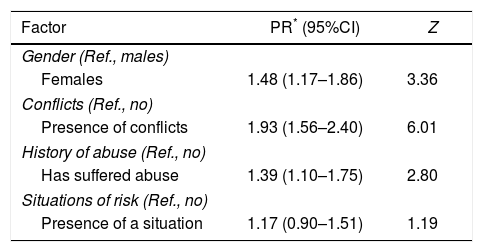
The model that best explained the presence of CMDs comprised gender, presence of conflicts, history of abuse or maltreatment and situations of risk: AIC, 973.9; χ2=5.68; Hosmer–Lemeshow goodness of fit test, 0.84 (Table 2).
Log-binomial regression model between the occurrence of common mental disorders and related factors.
| Factor | PR* (95%CI) | Z |
|---|---|---|
| Gender (Ref., males) | ||
| Females | 1.48 (1.17–1.86) | 3.36 |
| Conflicts (Ref., no) | ||
| Presence of conflicts | 1.93 (1.56–2.40) | 6.01 |
| History of abuse (Ref., no) | ||
| Has suffered abuse | 1.39 (1.10–1.75) | 2.80 |
| Situations of risk (Ref., no) | ||
| Presence of a situation | 1.17 (0.90–1.51) | 1.19 |
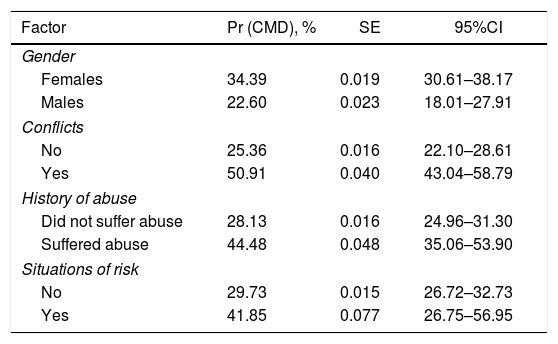
Table 3 shows the probability predictions and their 95% CIs for each of the factors derived from the final log-binomial regression model.
Probability prediction for factors related to the occurrence of common mental disorders.
| Factor | Pr (CMD), % | SE | 95%CI |
|---|---|---|---|
| Gender | |||
| Females | 34.39 | 0.019 | 30.61–38.17 |
| Males | 22.60 | 0.023 | 18.01–27.91 |
| Conflicts | |||
| No | 25.36 | 0.016 | 22.10–28.61 |
| Yes | 50.91 | 0.040 | 43.04–58.79 |
| History of abuse | |||
| Did not suffer abuse | 28.13 | 0.016 | 24.96–31.30 |
| Suffered abuse | 44.48 | 0.048 | 35.06–53.90 |
| Situations of risk | |||
| No | 29.73 | 0.015 | 26.72–32.73 |
| Yes | 41.85 | 0.077 | 26.75–56.95 |
95%CI: 95% confidence interval; Pr (CMD): probability of occurrence of common mental disorders; SE: standard error for estimated probability.
One of the most important findings in this study is the considerable prevalence of CMDs among dental students. This prevalence matches that reported in various local and international studies.6,9 However, it should be taken into account that the GHQ-12 was not designed for the purpose of making specific clinical diagnoses, like most scales, but as a quick, easy and economical way to assess the emotional state of patients or medical service users over the previous four weeks and in epidemiological studies.13
The GHQ-12 traditionally uses a Likert-type ordinal response pattern, with four options ranging from never to always (0-1-2-3). Nonetheless, recent studies indicate that response biases occur when this scoring system is used, due to the ambiguous wording of the responses in the negative items.20 Moreover, the first two responses apply equally well to subjects wishing to indicate the absence of a negative mood state. This response bias may lead to false factor structures for the construct, known as a reification error.21 To eliminate this effect, the originally-proposed binary scoring system (0-0-1-1) is recommended and used in this study, which thus proposes a one-factor solution.12 Various studies with confirmatory factor analysis (CFA) techniques compared the various models proposed (three-factor ordinal versus one-dimensional binary), and indicate acceptable measures of fit only for the one-dimensional factor structure using the dichotomous response system (response bias correction) and correlating the covariance of the six positively-worded items with the six negatively worded items,22 results which coincide with those reported with CFA in this study.
Even when a scale offers an overall score (sum of all items), it also offers assessment of possible cases by using a cut-off point that must be determined according to the total mean obtained in each particular research context. In this sense, for this study, given that we obtained a mean>2.7, the cut-off point of 4 offers a better psychometric performance for the identification of possible cases.23
Among the factors related to the presence of CMDs was gender; the differences observed in the distribution of the CMDs coincide with the distinct profile of psychological disorders of males and females.24,25 The greater presence of anxious, depressive and eating disorders in females has been corroborated in multiple studies. In this regard, some studies have identified a set of factors that may explain the female predominance in anxious and depressive disorders, as well as gender differences in the presence of other psychiatric disorders,26 such as the influence of sociocultural factors (greater willingness and ease among women to report and admit anxious and depressive sentiments and multiple roles in the family), biological factors (genetic predisposition, sex hormones, endocrine stress reactivity, neurotransmission systems and neuropsychological determinants)25 and the forms of expression of depressive disorders in males.25,27 Nevertheless, there is a consensus that these gender differences cannot only be explained by psychosocial and sociocultural factors and, given the concordance of findings between the different cultural groups, it could be concluded that gender differences in the occurrence of psychiatric disorders are mediated to a large extent by psychobiological variables.26
The presence of conflicts is another factor related to CMDs. Various studies report the presence of stressors associated with depression,28 such as the death of a family member, health problems in the family, changes in the family dynamic due to separation, divorce or abandonment, moving house, a parent remarrying, parents being overprotective, sibling conflicts, birth of a sibling and neighbour disputes. As well as these factors, the presence of stressors associated with the tasks of adolescence and enrolling in university education, entail specific demands and challenges. The transition through university is a complex experience for many young adults, in which various skills and competencies come into play in order to achieve their vocational goals. Students face various progressive stressors, such as responding to greater academic demands, changes in their social support network, a demand for greater autonomy and protagonism, vocational or academic failure, being uprooted and living alone if they come from provincial areas, etc., all of which are factors that could increase their risk of clinical symptoms.29
The results of this study also indicate that a history of abuse or maltreatment is a factor that explains the high occurrence of CMDs. This is supported by the literature, which highlights that traumatic events in childhood30,31 might constitute frequent, non-specific and non-determinant risk factors for certain diseases such as affective, anxious, eating and somatisation disorders, dissociative disorders and alcohol abuse.32,33 Females who suffer physical or sexual abuse have a high probability of aggressive behaviour, depression, anxiety or post-traumatic stress.34 It is estimated that, in the long term, the risk of attempted suicide in maltreated adolescents is five times greater than in those who were not abused in childhood.31
The cross-sectional design of this study, rooted in the simultaneous measurement of exposure and outcome, could pose a limitation, since it prevents us from establishing causal relationships between the associations detected. Moreover, the objective of this study was restricted to the assessment of responses, given the structure of the questionnaire applied, which enables the detection of CMD symptoms, but does not establish a formal diagnosis. As a result, longitudinal studies are needed which include a psychiatric interview (reference standard) to detect CMDs. Despite these possible limitations, this study's results support the hypothesis that preventive measures should be adopted in this population.
In conclusion, and without establishing a linear or exclusive relationship, it is possible to link the high occurrence of CMDs to the presence of family conflicts, being female, a history of abuse, conflicts and problematic situations. These factors must be carefully assessed in order to predict students’ wellbeing during their training.
The high prevalence of CMDs found in this study highlights that short-term preventive measures must be adopted, such as ongoing psycho-pedagogical support for students and psychological intervention for students (and relatives) who report that they have been abused in the past. Moreover, future healthcare professionals should note the importance of maintaining their physical and mental health, which can impact their capacity to care for patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Please cite this article as: Arrieta-Vergara K, Fortich-Mesa N, Tirado-Amador L, Simancas-Pallares M. Trastornos mentales comunes y factores asociados en estudiantes de Odontología en Cartagena, Colombia. Rev Colomb Psiquiat. 2019;48:10–16.