Telepsychiatry is defined as the use of information and communication technology (ICT) in providing remote psychiatric services. Telepsychiatry is applied using two types of communication: synchronous (real time) and asynchronous (store and forward).
ObjectiveTo determine the cost-effectiveness of a synchronous and an asynchronous telepsychiatric model in prison inmate patients with symptoms of depression.
MethodsA cost-effectiveness study was performed on a population consisting of 157 patients from the Establecimiento Penitenciario y Carcelario de Mediana Seguridad de Manizales, Colombia. The sample was determined by applying Zung self-administered surveys for depression (1965) and the Hamilton Depression Rating Scale (HDRS), the latter being the tool used for the comparison.
ResultsInitial Hamilton score, arrival time, duration of system downtime, and clinical effectiveness variables had normal distributions (p>0.05). There were significant differences (p<0.001) between care costs for the different models, showing that the mean cost of the asynchronous model is less than synchronous model, and making the asynchronous model more cost-effective.
ConclusionsThe asynchronous model is the most cost-effective model of telepsychiatry care for patients with depression admitted to a detention centre, according to the results of clinical effectiveness, cost measurement, and patient satisfaction.
La telepsiquiatría se define como la utilización de las tecnologías de la información y la comunicación (TIC) en la prestación de servicios de psiquiatría a distancia. La aplicación de la telepsiquiatría está dada por dos tipos diferentes de comunicación: sincrónico (tiempo real) y asincrónico (tiempo diferido).
ObjetivoDeterminar la costo-efectividad de un modelo de telepsiquiatría sincrónico frente a otro asincrónico en pacientes con síntomas de depresión internados en un centro de privación de libertad.
MétodosSe realizó un estudio de costo-efectividad. Constituyeron la población 157 pacientes del Establecimiento Penitenciario y Carcelario de Mediana Seguridad de Manizales, Colombia. La muestra se determinó con la encuesta autoaplicable Zung para la depresión (1965) y la escala de valoración de Hamilton para la evaluación de la depresión (Hamilton depression rating scale [HDRS]), instrumento con que se realizó la comparación.
ResultadosLas variables Hamilton inicial, tiempo de llegada, duración de caídas del sistema y efectividad clínica presentaron distribución normal con p > 0,05; entre los diferentes modelos hubo diferencias significativas (p < 0,001) en los costos de atención, y se evidenció que, en promedio, el costo del modelo asincrónico es menor que el del sincrónico; en promedio, la modalidad asincrónica es más costo-efectiva.
ConclusionesEl modelo de atención más costo-efectivo en telepsiquiatría para pacientes con trastorno depresivo internados en un centro de privación de libertad es el asincrónico según los resultados de efectividad clínica, medición de costos y satisfacción del paciente.
The World Health Organisation (WHO) estimates that in 2020, mental illness will affect 15% of the global population.1 At present, depression represents 4.3% of the world's disease burden, making it one of the main causes of disability worldwide.2 This has led to a search for innovative solutions to tackle mental health problems that go beyond any operational capacity of the current health services. According to the WHO, the future of medicine lies in transforming the exercise through communication and getting ahead of the looming crisis in patient care.3 Telepsychiatry is a clear example of this and constitutes an important tool for solving problems related to accessing health services in remote areas and/or areas that have a limited offering.4 In general terms, telepsychiatry is defined as the use of information and communication technologies (ICT) in the provision of remote psychiatry services.5 Telepsychiatry is applied using two different types of communication (synchronous and asynchronous), which are studied in this research.
In the synchronous or real-time modality, the patient and psychiatrist interact within the same temporal framework through live broadcasting systems, including telephone, chat and videoconferencing.6 The latter is the most widely used technology7 and the one with which most telepsychiatry sessions have been undertaken.8 The psychiatrist interviews the patient in real-time and issues a diagnosis and treatment on completing the consultation. It is worth mentioning that, due to regulatory provisions regarding telemedicine in Colombia, the patient must be accompanied by a general practitioner from start to finish, who attends to the patient if necessary and is responsible for completing and delivering the medical prescription to the patient.9 The second form of communication is the asynchronous or delayed-time modality, also known as store-and-forward. The aim of this technique is to obtain a psychiatrist's second opinion on the diagnosis and management of the patient. A general practitioner gathers and sends all the information (data, audio or video) to the psychiatrist, who responds within 8–24h (as previously agreed between the parties – there is no standard time frame); the general practitioner then delivers the respective treatment and management plan to the patient.10
In Colombia, the application of telepsychiatry forms part of Law 1419 of 2010, which also establishes the guidelines for implementing telehealth. It is likewise provided for in Agreement 029, regulating the use of telemedicine to facilitate timely access to services within the Mandatory Health Plan, and Resolution 2003 of 2014, which sets forth the technical procedures for its implementation. This resolution specifies the privacy and security conditions for patient data through the standard of medical histories and records; thus: “The remitting providers shall adopt the necessary safety measures during the transfer and storage of data, guaranteeing the privacy of the document and taking into account the guidelines established to that effect by the Ministry of Health and Social Protection” and “the provider shall encrypt the information for its transmission and create mechanisms of access to said information in accordance with institutional policies”. Statutory Law 1581 of 2012 also ratifies the privacy of personal data and their protection.
In 1995, researchers from Harvard Medical School presented the results of a research project on 26 patients treated in-person versus virtually, with similar results between the two groups.11 It should be emphasised that a significant percentage of psychiatric disorders can be diagnosed and treated by means of telepsychiatry, although there are certain situations that require specific considerations, such as patients with suicidal ideation and those who present decompensated borderline personality disorder, among others.4 In other systematic literature reviews, the benefits of telepsychiatry are presented as an effective alternative for patient care, although this is only in reference to the synchronous modality and thus evinces the need to consider cost-effectiveness studies in greater depth.12
Although telepsychiatry is seen to be an important strategy for remote populations,13,14 there are population groups with special characteristics, such as in prisons and penitentiaries, which make them particularly isolated and difficult-to-access.7 In Colombia, these detention centres present important limitations in terms of access and availability. In the survey conducted in 2010 by the Colombian Ombudsman's Office, it was found that only 22% of detention centres have a permanent psychiatrist, while the others use outpatient care, with considerable difficulties, according to patients and relatives, regarding the quality of care provided; they also state that the care given by the psychiatrist is slow, cumbersome and, in some cases, non-existent.15 This clearly demonstrates serious problems in the care model, as confirmed in an interview with healthcare personnel from the Medium-Security Penitentiary and Prison Establishment of Manizales and Pereira, which affirms the following: (a) difficult management of patient emergencies that require a psychiatric assessment due to there being no access to a specialist physician and difficulty transferring them to a care centre due to administrative and safety procedures; (b) short consultation time due to the high number of patients and the little time spent by the psychiatrist at the detention centre, and (c) impossibility of treating the entire population requiring the service, leading to the prioritisation of the most critical cases.
The first use of telepsychiatry in prisons was reported in Miami in 1974 through a microwave link. It was not possible to maintain the system due to its high cost.16 In the United States, around 2 million adults are detained in prisons, and more than half report some kind of symptom associated with a mental illness.17 Between 1993 and 1996, videoconferencing increased from 1750 to 18,766 cases in correctional and non-correctional centres.18 In another study, the use of telepsychiatry in prisons was assessed in seven American states, and it was concluded that this mode of care increases access to mental health services through treatment continuity, thus improving patients’ quality of life and prison safety. Similarly, a decrease in care-related costs was also evident.19
Moreover, as regards cost-effectiveness studies included in economic healthcare evaluations, these are defined as the comparison of two or more potentially competitive and, in general, mutually exclusive intervention alternatives.20 In the case of this study, the synchronous and asynchronous telepsychiatry care modalities were compared in prison inmates with depression, in order to determine which is the most cost-effective.
Material and methodsA cost-effectiveness study was conducted. The population comprised 157 patients from the Medium-Security Penitentiary and Prison Establishment of Manizales (MSPPE). The sample was determined using the Zung Self-Rating Depression Scale (1965).21 Subsequently, the people within the “mild depression” and “very severe depression” bracket of Zung's scale were selected and informed consent was requested. The people who consented were enrolled in the study. Those who did not give their consent and had assessed themselves as depressed were put in touch with the institution's health service for management. The Hamilton Depression Rating Scale (HDRS)22 was then applied, which is a 17-question scale used by general practitioners, designed to quantitatively evaluate symptom severity and assess changes in the depressed patient. The scoring range goes from 0 to >23. The sum of all the questions classifies people as: normal 0–7; mild depression 8–13; moderate depression 14–18; severe depression 19–22; and very severe depression >23. The people from the sample with a positive HDRS score, i.e. in the mild-very severe depression bracket, were randomly assigned to a synchronous or asynchronous telepsychiatry care model. The study sample comprised a total of 106 patients in whom depression was eventually reconfirmed. The following inclusion criteria were considered: male over 18 years of age, referred by the general practitioner with a positive HDRS score and signature of the informed consent form. As regards the exclusion criteria, the following aspects were taken into account: visual impairment, hearing impairment, currently undergoing psychiatric treatment and failure to sign the informed consent form. Subsequently, a date for telemedicine care was assigned in accordance with the permits granted by the Colombian Penitentiary and Prison Institute (INPEC) for this activity. The patients in the asynchronous modality were interviewed and assessed in the prison by a general practitioner who, in turn, sent all of the patient's clinical information to a psychiatrist via a telemedicine technology platform for assessment, who then issued a final diagnosis and treatment. The mean response time of the psychiatrist was 8 hours. The general practitioner then logged into the platform to check the management approach issued by the specialist and to complete the medical prescription, pharmacological treatment, where applicable, and follow-up appointment, as appropriate. The patients in the synchronous modality were directly assessed by the psychiatrist via videoconferencing; in this same consultation the diagnosis was issued and the medical prescription completed, along with the pharmacological treatment, if required, and the follow-up appointment, as appropriate. During the follow-up appointment, the HDRS was reissued in both models, which enabled assessment from the patient's perspective and determined whether the patient had improved, deteriorated or remained the same with respect to the first HDRS applied.
In the data analysis, the synchronous and asynchronous model was assumed as the independent variable, while the dependent variables were clinical progression, remission, patient satisfaction and costs. The statistical analysis consisted in establishing the relationship between the different variables proposed. Parametric tests (Student's t test, χ2 and ANOVA, as appropriate) were applied to the normal distribution variables, while non-parametric tests (Fisher's exact test, Mann–Whitney U test, Wilcoxon W test, Wilcoxon T test, McNemar's test and Kruskal–Wallis test) were applied to non-normally distributed variables. For the cost-effectiveness analysis, the direct costs of the study were estimated, which include, among others, the technology platform, connectivity, human resources and consumables.Study 1 hypothesis The effectiveness on the mental health of prison inmates treated in the synchronous and asynchronous telepsychiatry modalities is the same. The consultation costs of the synchronous and asynchronous telepsychiatry models are different, and are higher in the synchronous model since this seemingly involves more of the psychiatrist's time due to the duration of the consultation and a more complex infrastructure.
The informed consent form was approved by the Bioethics Committee of the University of Caldas, Act no. 002 of 2014, based on the Ministry of Health Resolution 008430 of 1993 on scientific, technical and administrative standards for health research, in this case for a vulnerable population/subordinate subjects.
ResultsThe Kolmogorov–Smirnov test was applied to establish normality. The results obtained in the test indicate that the baseline Hamilton variables, arrival time, duration of system failures and clinical effectiveness present normal distribution (p>0.05).
Component: clinical effectivenessThis provides a response to the study 1 hypothesis, which considers the need to establish whether the effectiveness on the mental health of prison inmates treated in the synchronous and asynchronous telepsychiatry modalities is the same. Clinical effectiveness is defined by the progression of the depression symptoms shown by a patient through the baseline and final HDRS score. The following statistical tests were performed to that effect:
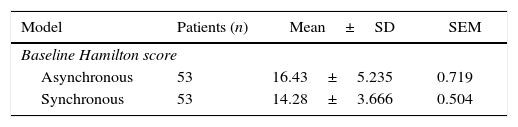
Test of means to demonstrate any differences in the baseline Hamilton scores between the synchronous and asynchronous modalitiesSignificant differences were found in the means corresponding to the baseline Hamilton score between both models (p=0.016), with a higher level of mean depression in the asynchronous model (16.43>14.28) (Table 1), thus demonstrating that, on average, the patients treated with the asynchronous model presented more severe symptoms of depression than those treated with the synchronous model.
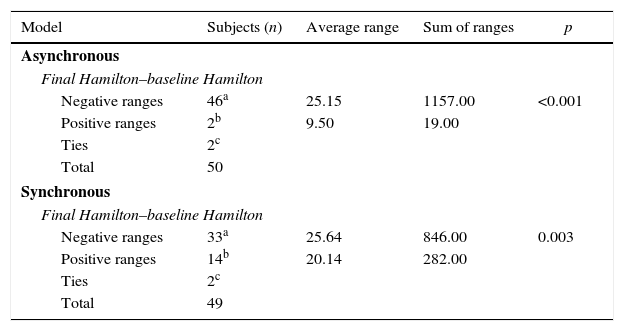
Paired means test on baseline versus final Hamilton variables for the asynchronous versus synchronous models to demonstrate progression in the treatmentThe results of the Wilcoxon test for the progression of paired variables showed that there is a progression in the final versus baseline score of the Hamilton scale in the two models, which demonstrates that both present significant advances in treating depression (asynchronous model, p<0.001, i.e. highly effective; synchronous model, p=0.003, i.e. very effective) (Table 2).
Paired means test on baseline versus final Hamilton variables.
| Model | Subjects (n) | Average range | Sum of ranges | p |
|---|---|---|---|---|
| Asynchronous | ||||
| Final Hamilton–baseline Hamilton | ||||
| Negative ranges | 46a | 25.15 | 1157.00 | <0.001 |
| Positive ranges | 2b | 9.50 | 19.00 | |
| Ties | 2c | |||
| Total | 50 | |||
| Synchronous | ||||
| Final Hamilton–baseline Hamilton | ||||
| Negative ranges | 33a | 25.64 | 846.00 | 0.003 |
| Positive ranges | 14b | 20.14 | 282.00 | |
| Ties | 2c | |||
| Total | 49 | |||
Differences were seen in the average scores of the final Hamilton scale between the two telepsychiatry models, with the average value being better in the asynchronous model (p=0.010<p=0.05). This lower result indicates an improvement in the depressive symptoms suffered by the assessed patients.
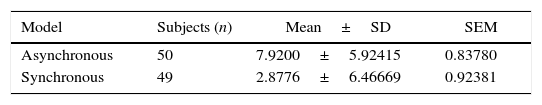
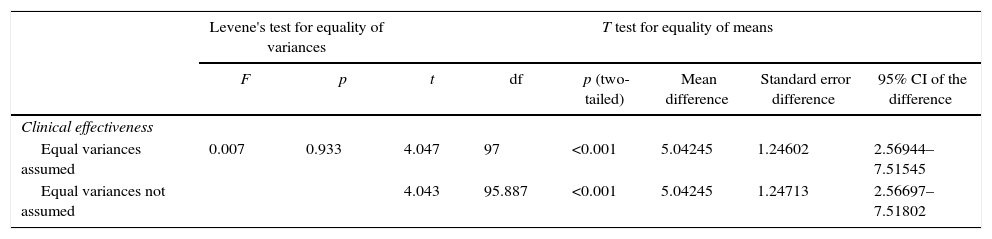
Tests for the equality of the mean progression in the Hamilton scale, with the asynchronous versus synchronous modalities, in order to demonstrate differences in the effectiveness of each modelThere were significant differences (p<0.001) regarding the mean clinical effectiveness of each model, which was greater with the asynchronous model with an average change close to 8 points on the HDRS, compared to 3 points with the synchronous model (Tables 3 and 4).
Independent sample test.
| Levene's test for equality of variances | T test for equality of means | |||||||
|---|---|---|---|---|---|---|---|---|
| F | p | t | df | p (two-tailed) | Mean difference | Standard error difference | 95% CI of the difference | |
| Clinical effectiveness | ||||||||
| Equal variances assumed | 0.007 | 0.933 | 4.047 | 97 | <0.001 | 5.04245 | 1.24602 | 2.56944–7.51545 |
| Equal variances not assumed | 4.043 | 95.887 | <0.001 | 5.04245 | 1.24713 | 2.56697–7.51802 | ||
Conclusions on study 1 hypothesis: Although it is certain that both models (asynchronous and synchronous) present proven clinical effectiveness, i.e. progression in the HDRS following treatment, this is not associated with variables such as age, sentence duration, perceived quality of treatment and time employed, which is an excellent result that indicates the significance of telepsychiatry care. Nevertheless, it is worth noting that the clinical effectiveness results obtained with the asynchronous model are higher than those with the synchronous model.
Component: cost-related care timesAnalysing consultation costs in the synchronous and asynchronous telepsychiatry models is based on the variability of the care times that each modality involves, in the sense that the costing of wage factors of the health professionals involved in treatment may be used to establish the variable costs that influence the cost-effectiveness model through consultation times and poor quality times that affect the total cost. On a preliminary basis, it can be established that a higher cost is expected in the synchronous model, as this seemingly requires more professional time due to the duration of the consultation as well as a more complex infrastructure.
There are no differences (p=0.140) in the average initial consultation time with each model, which indicates regularity in the time spent by health professionals on comprehensive care processes.
The variables related to consultation time and clinical effectiveness were independent, thus indicating that time is not a determining factor in the patients’ progression. Clinical and professional management variables through a specific model (synchronous or asynchronous), which enable the generation of effective telepsychiatry results, on the other hand, are determining factors.
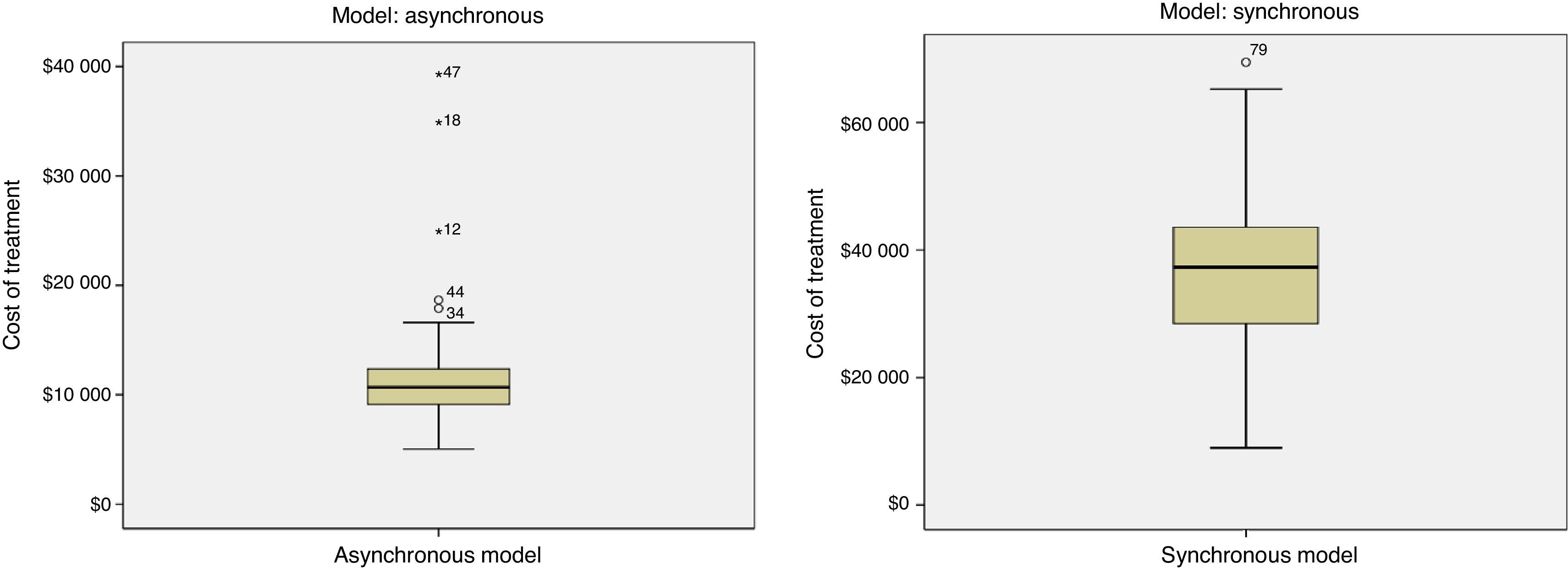
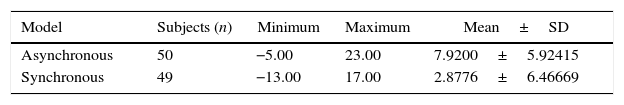
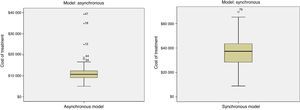
Equality analysis in average treatment costs and the different modalities in order to establish any significant differencesOn applying the Kruskal–Wallis test, significant differences were found between the different models (p<0.001) for treatment costs: on average, the cost of the asynchronous model is less than half of the synchronous model treatment cost (Fig. 1).
Poor quality costs (time lost due to internet outage, delays in starting the medical consultation for logistical reasons, technology platform failure during the consultation, etc.) for consultations in the synchronous and asynchronous models are statistically equal (p=0.108), which continues to indicate equality among the service provision conditions in treating depressed patients though one telepsychiatry modality or another.
Conclusions on study 2 hypothesis: The consultation costs of the synchronous and asynchronous telepsychiatry models are different and were found to be much higher in the synchronous model. Poor quality costs are equal in both modalities.
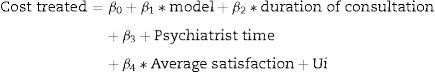
Predictive model for the cost of treatment with each modalityThe model that best explains and predicts the cost of care was determined by establishing the following regression model:
It may be established that the cost of care is explained in 93.8% by the variables considered, that the model is correctly specified and that the validations relating to the significance of the coefficients in individual and group tests are significant and different from zero.
Cost-effectiveness analysis of treatment in the asynchronous and synchronous models using the mean ratio methodFinally, the cost-effectiveness analysis was performed using the mean ratio method, in which the average treatment cost variables were compared to the clinical effectiveness of treatment with each model (Table 5).
According to the results, the cost-effectiveness analysis of treatment using the mean ratio method for the asynchronous and synchronous modalities allows us to conclude that, on average, the asynchronous modality is most cost-effective.
DiscussionTelepsychiatry has traditionally been provided in two modalities: synchronous and asynchronous.23 Effectiveness studies, cost studies and some cost-effectiveness studies can be found in the literature,7,24 applied to each of these modalities independently, but no research projects involving a comparative cost-effectiveness study on both modalities were discovered after searching the main scientific databases (MEDLINE, PubMed, PsychInfo, EMBASE, Science Citation Index, SciELO, Science Direct, LILACS, OVID, ProQuest and The Cochrane Library) and relevant scientific journals (Psychiatr Serv, Journal of Telemedicine and Telecare and Telemedicine and e-Health).
The results of this research study showed the effectiveness of the intervention in both telepsychiatry models (synchronous and asynchronous, which is the most effective). Moreover, synchronous telepsychiatry effectiveness studies through videoconferencing have been compared to face-to-face care, and the results demonstrate that telepsychiatry is a more effective alternative for providing mental health services.25–27 Corroborating the above, a meta-analysis including 500 patients distributed across 14 studies concluded that there was no significant difference in precision and patient satisfaction in the provision of in-person versus virtual psychiatry services.28 That said, no studies were found that assess the effectiveness of asynchronous telepsychiatry; one retrospective study conducted in India on 94 patients exclusively addressed the feasibility of this email-based care model and found that it could be used to establish a definitive diagnosis and recommend a suitable treatment in 95% of patients.29 Moreover, the feasibility of the asynchronous model was also measured in a study sponsored by the University of California, this time by means of sending a video recording of the consultation to the psychiatrist, obtaining a comparable result to the Indian study.23
In this research project, although no comparison was made between the in-person and virtual models, a relevant result was obtained in the sense that the effectiveness of the intervention with both telepsychiatry models—synchronous and asynchronous—was determined, the latter being the most effective.
Some studies recommend analysing not only effectiveness, but also the costs associated with telepsychiatry.30,31 With regard to this variable, one study was identified that compared the synchronous and asynchronous models to face-to-face care. It found asynchronous care to be the most cost-effective due to a reduction in the specialist's intervention time, which is assumed by a general practitioner.32
On average, the asynchronous modality was found to be the most cost-effective in this research. Other studies also indicate factors contributing to this conclusion: basic infrastructure, easy management for healthcare personnel (e.g. via email),25 reduction in the time required by the specialist to conclude consultations and exploiting specialists’ downtime.26
As regards the synchronous modality, a study conducted in Israel concludes that it is even more costly than in-person care due to the technological infrastructure and human resources required.33 The aforementioned Indian study adds to the cost analysis of the synchronous modality that, although the specialist's time is similar to face-to-face care, only travel costs are reduced. Moreover, it may even take more time because, on occasions, the logistics of connecting the patient and specialist in real-time is complex.25
In contrast, the costs analysed in a prison environment take on another dimension. There are studies in the United States that address the costs of telepsychiatry care in the synchronous modality versus in-person care, which calculate an average consultation cost of $173 compared to $71 when said care is carried out using videoconferencing.34
In summary, synchronous telepsychiatry has been shown to be just as effective as face-to-face psychiatric care. In contrast, in the asynchronous modality there are no previous studies that assess effectiveness, though there are some that prove its feasibility, i.e. that the provision of telepsychiatry services is possible in this modality.
That said, with regard to the costs of both modalities, the literature concludes that the asynchronous model is less costly, as opposed to the synchronous model, as the latter requires more time spent by the specialist, as well as a complex logistical and technological infrastructure.
Prison inmates are one of the population groups that could benefit most from telepsychiatry. Previous studies positively assessed the improvement in access to mental health services thanks to the continuity of the service provision, reduced care costs in this field,20 improved safety of healthcare personnel20 and the effectiveness of care.35 Moreover, there are even reports that indicate that telepsychiatry has proven more effective than in-person care in the treatment of diseases such as depression.36
With the results obtained in this research, it may be affirmed that both telepsychiatry models were effective in treating depression in prisons. However, the cost-effectiveness analysis, which compared two intervention alternatives,37 found the asynchronous modality to be superior to the synchronous model for the same condition. The reasons leading to this conclusion are grouped into three main categories: (a) clinical effectiveness; (b) care costs for each model, and (c) degree of satisfaction regarding the care received.
This research opens a new door for future analyses in the field, as, although positive results were obtained, the study was limited to a disease and population group with unique characteristics. The formation of interdisciplinary working teams to prepare the prison environment for a project such as this one is recommended, along with a multidimensional approach to patients that goes beyond purely clinical considerations, given the social, cultural, legal and institutional problems specific to a prison environment.
ConclusionsThe most cost-effective telepsychiatry care model for prison inmates with depression is the asynchronous model, as shown by the clinical effectiveness, cost measurement and patient satisfaction results.
This study has highlighted the need to carry out further research that assesses the synchronous versus asynchronous care models in telepsychiatry, in order to validate other conditions and different population groups with a greater number of experiences.
The novelty of this project stems from its contributions to the generation of new knowledge, as the literature review found no references of other research projects that assessed the cost-effectiveness of the synchronous versus asynchronous modalities in telepsychiatry.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestAlexis Vladimir Benito Devia owns shares in CREIMED, a beneficiary of the research project, and states: “We have received an entry from COLCIENCIAS and an offsetting entry from CREIMED. Neither institution has influenced or intervened in the conduct of the research or results, for which we were free to choose the team to perform the research, who were only selected for their technical and professional abilities”.
To the Ministry of Information and Communication Technologies (MinTIC) with the Innovation Hub programme; to the COLCIENCIAS Science, Technology and Innovation Department; to the University of Caldas and its Telehealth programme; to IPS CREIMED; to the Penitentiary and Prison Institute (INPEC) of the city of Manizales and the inmates who took part in the research project, for their support and collaboration in its conduct; and, finally, to the healthcare professionals and those from other fields who were involved in and supported the conduct of this study in one way or another to ensure a successful outcome.
This article is registered within COLCIENCIAS summons 604-2012, with the research project entitled “Effectiveness of a synchronous vs asynchronous telepsychiatry model on the mental health of prison inmates”.
Please cite this article as: Barrera-Valencia C, Benito-Devia AV, Vélez-Álvarez C, Figueroa-Barrera M, Franco-Idárraga SM. Costo-efectividad de telepsiquiatría sincrónica frente a asincrónica para personas con depresión privadas de la libertad. Rev Colomb Psiquiat. 2017;46:65–73.